Symptoms of dermatitis, causes and treatment in adults
Dermatitis is a chronic skin disease that manifests itself as a response to an irritant. In dermatology, this disease can often be found under the term neurodermatitis, eczema, in which there are similar symptoms, manifested in the form of skin itching, rashes on different parts of the body. Treating dermatitis in adults is quite difficult, since in order to achieve stable remission it is necessary to determine the cause of the disease, its type and stage of development.
Depending on the etiological factor, dermatitis is divided into several types, each of which requires an individual approach to treatment. The danger of dermatitis is that with improper treatment or its complete absence, the risk of extensive inflammation with the addition of bacterial flora increases. This condition can cause deep damage to the skin and purulent-inflammatory processes, which significantly complicates the treatment and course of the disease itself.
Very often, the first symptoms of dermatitis appear in childhood, but over time the disease returns and worries in adulthood.
Causes
The main types/forms of the skin disease in question can develop for distant and close reasons. The first category of reasons includes predisposition:
| Acquired | We are talking about those patients who suffered atopic dermatitis in childhood - they develop a predisposition to the occurrence of various types and forms of the skin disease in question. Moreover, the parents never had a history of dermatitis. |
| Genetic | according to statistics, parents diagnosed with dermatitis of any form give birth to children with the same disease in 96% of cases, but if only one parent has this skin disease, then this probability is only 58% |
Related causes of dermatitis (they are also classified as provoked):
- the entry into the blood of irritants that can cause dermatitis - chemicals, pollen, food, medications, etc.
- stressful condition. Many are sure that stress is a simple ailment that quickly goes away after proper rest. In fact, a stressful state is a complex protective reaction of the body, which occurs under the influence of hormones.
Even if irritants enter the blood, this does not mean the immediate development of dermatitis - it is necessary that favorable factors be present:
- high air temperature;
- severely weakened immunity - for example, against the background of a long-term illness;
- receiving radiation - for example, from the sun or quartz lamps;
- prolonged exposure to cold on the skin - for example, dermatitis may appear after not wearing gloves during a cold winter.
Why does eczema occur on fingers?
The exact causes of eczema on the fingers are still unknown. Immunological disorders play a decisive role in its development. The onset of the disease is provoked by external or internal factors, and they may differ from person to person.
What causes eczema on the fingers:
- constant contact with aggressive chemical components or metals;
- dry air, severe frost and other types of thermal effects;
- insufficient hand hygiene;
- frequent mechanical damage, wounds and abrasions on the hands;
- allergic reaction to food;
- hereditary predisposition;
- disorders in the endocrine and digestive system.
Dyshidrotic eczema on the fingers is especially widespread. Its name is explained by the fact that previously the development of the disease was associated with blockage of the sweat glands. The pathology often affects the skin of the palms. Its development is promoted by hyperhidrosis - excessive sweating.
Classification
Depending on the cause of development, the following types of dermatitis are distinguished.
- Seborrheic dermatitis is a chronic pathology of the skin rich in sebaceous glands, resulting from the activation of the opportunistic lipophilic yeast fungus Malassezia furfur.
- Photodermatitis is a skin rash that occurs due to increased sensitivity to sunlight (visible light rays and UV radiation).
- Allergic contact dermatitis is a classic delayed-type reaction that develops due to the body's increased sensitivity to the allergen and the involvement of T-lymphocytes in the immune process.
- Simple contact dermatitis is an immediate skin reaction that occurs when directly exposed to an irritating agent.
- Toxic-allergic dermatitis (toxidermia) is an acute inflammation of the skin that occurs under the influence of a toxic allergenic agent that enters the body through the digestive, respiratory tract or by injection.
- Atopic dermatitis is a chronic polyetiological skin pathology that is inherited.
People who are in a constant state of stress are more susceptible to the disease. Those with dry skin are also at risk, especially in windy and cold weather.
Reasons for appearance
The main factors that can trigger the appearance of one or another form of dermatitis have already been listed. All inflammation and irritation of skin diseases are the result of remote or provoked causes.
- Remote ones include genetic predisposition or acquired individual predisposition. The latter occurs, for example, due to allergies or a previous infectious disease.
Related causes that trigger the development of dermatitis are various conditions to which the body reacts with skin irritation. These include stress, contact with chemicals, reaction to climate, and hormonal changes in the body.
Regardless of what resulted from the onset of the disease, remember: dermatitis must be treated immediately before it becomes protracted and chronic.
Symptoms of dermatitis
For each of the above types of dermatitis in adults, characteristic symptoms have been identified (see photo). But doctors also identify several common signs that will be characteristic of each of the existing types of disease:
- Redness (erythema). Erythema is increased blood filling of the dermal capillaries. In the acute form, redness with unclear edges and swelling is observed. For chronic dermatitis, erythema is not necessary. When pressed, the area of hyperemic skin turns pale for a while. Erythema should not be confused with hemorrhage (bleeding under the skin). Hemorrhage is considered as a separate manifestation of skin pathologies - hemorrhagic diathesis;
- Itching (prurigo). Its intensity depends on the strength of irritation of the skin nerve endings. The discrepancy between the strength of prurigo and skin manifestations (severe itching with minor rashes) is a sign of allergy in atopic dermatitis. With contact dermatitis, itching at the site of application of the pathogen is adequate to the damage;
- Exudation. In acute forms of dermatitis, exudative inflammation with copious discharge is possible. In chronic forms - lichenification (thickening of skin areas with a rough pattern), cracks in the skin and excoriation (self-scratching);
- Peeling of the skin (desquamation). Pathological desquamation is caused by increased dryness (xerosis) of the skin due to dehydration and insufficiency of the sebaceous glands. Desquamation and xerosis are observed in chronic dermatitis with allergic and inflammatory processes.
- Rash (eczema). The morphology of the rash and its localization are typical for specific dermatitis. The most common localization of rashes is moving parts of the body (skin over joints), face, scalp, sides of the body, groin area.
Additional symptoms are important in the differential diagnosis of specific dermatitis; they are identified during questioning, examination, laboratory tests and functional tests.
Symptoms of eczema on fingers
In the early stages of eczema, only increased dryness of the skin is observed. It is almost impossible to eliminate with conventional moisturizers. Due to severe dryness, cracks appear, and inflammation occurs at the site of their formation. They cause itching and burning.
The general list of symptoms of eczema on the fingers includes:
- increase in epithelial pattern on the skin;
- constant feeling of skin tightness;
- roughening of the skin;
- swelling and redness of the affected skin;
- red sprinkle elements.
The rash rapidly spreads across the skin, enlarges and merges into large plaques. All this causes severe itching in a person, which prevents normal sleep and causes nervous disorders. Very deep cracks form in the bends of the fingers, which hurt and do not heal for a long time. The skin in this area continues to peel off, and if a bacterial infection occurs, purulent discharge appears.
Atopic dermatitis
The pathogenesis of atopic dermatitis is based on genetically determined features of the immune response. Most often, the disease develops in children with a hereditary predisposition between the ages of 1 and 5 years.
The development of the pathological process is provoked by food products (proteins of animal and plant origin), stress and other unfavorable exogenous factors, UV radiation, as well as aggressive meteorological influences.
Atopic dermatitis occurs with periods of exacerbations and remissions and is characterized by the development of skin inflammatory reactions, increased reactivity to various irritants, itching and rashes. The disease begins in early childhood, but over time its clinical manifestations weaken, and by the age of 30-40 a spontaneous cure occurs, or symptoms regress.
Clinical researches
La-Cree shampoo for dry and sensitive scalp is intended for gentle cleansing of hair, normalization of the natural balance of the scalp of adults and children over 3 years old.
Clinical studies have proven the high effectiveness, safety and tolerability of products for daily skin care for children and adults with mild and moderate forms of atopic dermatitis and during remission, accompanied by a decrease in the quality of life of patients.
Sources:
- Andropova T.V., Gudina M.V., Odintsova I.N., Hygiene of children and adolescents, Siberian State Medical University Publishing House, 2022.
- Cohen Bernard A. Pediatric dermatology, MEDpress-inform, 2015.
- Sukolin Gennady Ivanovich, Illustrated clinical dermatology. Brief alphabetical reference book, Lux Print publishing house, 2010.
- Kildiyarova Rita Rafgatovna, Pediatrician for every day. Guide for doctors, GEOTAR-Media, 2022.
Photos of dermatitis
Photo album on the disease
Seborrheic dermatitis
Symptoms of seborrheic dermatitis, which can be seen in the photo on the Internet:
- red plaques with clear boundaries (with dry dermatitis);
- high blood supply to the dermal capillaries (erythema);
- weeping in the groin, behind the ears;
- the appearance of cracks, serous crusts;
- exudative inflammation;
- itchy dermatitis;
- uneven peeling on the head, dandruff, alopecia;
- damage to large areas of skin in severe cases;
- the occurrence of other types of eczema (ear dermatitis and others).
Inflammation of the skin as a result of high secretion of altered sebum or after exposure to microbes is called seborrheic or fungal dermatitis. It is not a contagious disease and therefore cannot be transmitted from person to person. The activity of opportunistic fungi manifests itself under stress, endocrine or immune disorders, and various forms of damage to the nervous system. They concentrate on areas of the skin inhabited by sebaceous glands: face, chest, back, ears, head.
Infectious dermatitis
The main causes of this disease are infections in non-healing wounds on the skin. The infectious type develops in patients with chickenpox, atopic dermatitis, or another disease if the infection gets into the rash that accompanies these diseases (often by scratching). Also, skin irritation may appear after operations and injuries due to infection with staphylococcus, streptococcus, etc.
The course of the disease is accompanied by the appearance of pustules without clear boundaries on the surface of the skin or purulent inflammation under the skin.
Allergic dermatitis
Inflammation occurs as a result of the body's reaction to a specific pathogen. The causative agents can be dust, plant pollen, animal hair, odors of perfumes or chemicals, medications, food, liquids, etc. It is often associated with seasonal manifestations of allergies. Intoxication can occur as a result of the production of certain substances in diseases of the kidneys, liver, thyroid gland, helminthic infestations, and the development of tumors.
How it manifests itself:
- the skin becomes covered with large red spots;
- small bubbles form on their surface;
- then they burst, forming weeping wounds;
- the rash is very itchy;
- accompanied by sneezing, coughing, lacrimation, and increased sensitivity to light.
An allergen can enter the bloodstream with food, through the mucous membrane of the respiratory tract, or through injections. Located on any area of the skin or mucous membrane.
Contact dermatitis
These are inflammatory processes on the skin caused by contact with a certain irritant. These are friction, pressure, exposure to temperature, radiation, burns and other strong irritants. With this type, direct damage to the skin occurs, symptoms appear immediately, and contact with the irritant must be eliminated as soon as possible.
Symptoms of contact dermatitis:
- swelling;
- hemorrhages, microhematomas;
- pronounced hyperemia;
- small papules, vesicles;
- weeping, scales, crusts;
- large bubbles;
- zones of necrosis.
Like food dermatitis, this is a type of allergic form of the disease. Occurs after contact with substances that cause an inflammatory response in the body. These may be chemical reagents, UV rays (photocontact or photodermatitis), x-rays, high/low temperature or mechanical factors. Stinging cells, pollen, plant sap, and caterpillar larvae can provoke a skin reaction. The main difference between this type of eczema is that it has no incubation period.
Diagnostics
Diagnosis of dermatitis consists of an initial blood test. To exclude the possibility of mycotic skin lesions joining the current processes, seeding and microscopic examination of scales from the area that has been affected is also carried out.
Allergic dermatitis requires various types of allergy tests, mainly skin tests are used for this. In frequent cases, the allergic nature of the factor acting as an irritant is determined through a blood test (increased lg E level). Based on the results of the studies, an appropriate assessment of the patient’s condition is made.
Diagnosis of dermatitis
The diagnosis is made based on the existing symptoms, the results of an external examination of the patient’s skin and mucous membranes, visual assessment and localization of pathological changes.
An anamnesis of the disease must be studied in order to establish the possible cause of dermatitis and its genetic cause. Laboratory diagnosis of dermatitis includes the following studies:
- General clinical blood test. During an allergic reaction, an increase in the number of eosinophils is observed, and an accelerated ESR indicates inflammation.
- Blood chemistry. Includes determination of the concentration of AST, ALT, total bilirubin, triglycerides, cholesterol, total protein.
- Determination of the level of immunoglobulins in blood serum, antibodies to food, household antigens, antigens of plant, animal and chemical origin.
If necessary, it is possible to conduct a histological examination of the biomaterial obtained through skin biopsy. Genetic blood testing helps determine hereditary predisposition to the development of atopic disease. In the presence of a purulent process or severe inflammation, a microscopic and bacteriological examination of the smear is prescribed in order to clarify the causative agent. Additionally, for dermatitis, tests are carried out for giardiasis and other forms of intestinal parasites, and the organs of the digestive tract are examined.
Treatment of dermatitis
In the case of dermatitis, the effectiveness of treatment depends on its form and is always selected individually.
Treatment of dermatitis in adults should begin by determining the cause. It is necessary to identify the irritant (allergen, toxic substance, microbial pathogen) and eliminate it. If the irritant is not identified, as is often the case with allergic and especially neuroallergic dermatitis, treatment will be only symptomatic, i.e. aimed at eliminating symptoms and maintaining remission.
Treatment of dermatitis is conservative, consisting of local and general therapy. Acute dermatitis and dermatitis in children, as a rule, are treated only with local remedies, while chronic forms require a combination of general and local therapy. Local therapy for dermatitis consists of treating the affected areas of the skin. Skin rashes are treated with anti-inflammatory and antibacterial drugs in the form of mash, powders, ointments, solutions - depending on the form of the inflammatory element and its stage. Dermatitis on the face (seborrheic) is treated with antifungal ointments. Chronic dermatitis is treated with corticosteroid anti-inflammatory drugs, acute dermatitis is treated with aniline dyes. Deep ulcerative lesions are treated in a hospital setting.
General treatment of dermatitis consists of taking immunomodulatory, antihistamine, and sedatives, depending on the cause of the disease. It is also necessary to eliminate all sources of chronic infection, such as teeth destroyed by caries, chronic sinusitis, tonsillitis, etc.
Treatment of skin infections in atopic dermatitis in children
In the international consensus document on atopic dermatitis (USA, 2002), experts note that atopic dermatitis is typically an inherited disease often associated with asthma, food allergies, allergic rhinitis and recurrent skin infections. Infection can significantly change the course of the disease. If a patient develops a bacterial, fungal or viral skin infection, it is necessary to quickly identify this infection and begin specific therapy to eliminate it [1].
This approach is due to the fact that viruses, bacteria and fungi can be triggers of atopic dermatitis and lead to exacerbation of the disease. On the other hand, ceramide deficiency as a result of a pronounced decrease in sphingomyelin levels contributes to dry skin and easier penetration of infectious agents and allergens into the damaged epidermis. In addition, the epidermal skin barrier is disrupted by proteases from house dust mites and Staphylococcus (S.) aureus, which, in combination with other factors, also increases the risk of allergen penetration and supports the inflammatory process in the skin. There are also observations indicating the role of bacterial and fungal colonization in the formation of therapy-resistant and more severe recurrent atopic dermatitis [2, 3]. Finally, secondary infection of the skin or deep scratching can lead to scarring, which is generally not typical for atopic dermatitis itself.
The microflora of healthy skin is usually not characterized by colonization by S. aureus, while the skin of more than 90% of patients with atopic dermatitis is contaminated with this type of bacteria, the number of which in weeping lesions can be over 14 million per square meter. see [2]. Moreover, a high degree of skin colonization with S. aureus is possible even in the absence of clinical manifestations of a bacterial skin infection. Toxins (so-called superantigens) produced by S. aureus on the skin surface stimulate the activation of T lymphocytes and macrophages and thereby enhance the allergic inflammatory immune response of the skin. Studies have shown that S. aureus exotoxins worsen the course of atopic dermatitis, and the level of specific immunoglobulin (Ig) E antibodies to staphylococcal superantigens correlates with the severity of the disease [3]. It is also assumed that superantigens are involved in the development of skin insensitivity to topical glucocorticosteroids and/or a decrease in the therapeutic effect of these drugs [3–5].
Another cause of severe atopic dermatitis, refractory to standard therapy, is considered by some authors to be fungal sensitization [5–7]. In Europe, 30–68% of patients with recurrent severe atopic dermatitis, as well as with a variant of the localization of the disease on the head and neck, have specific IgE antibodies in the blood or a positive reaction to prick or patch tests for the fungi Malassezia furfur (formerly called Pityrosporum ovale) [5].
In rare cases, the skin of patients with atopic dermatitis becomes infected with viruses, most often with herpes simplex virus types 1 and 2, as well as with molluscum contagiosum virus [1, 5, 7]. Herpetic skin infection can occur repeatedly in the same patients, while in others it almost never occurs. It is believed that patients with severe atopic dermatitis or those who have not received proper treatment are at greatest risk. Sometimes eczema herpeticum in patients with atopic dermatitis should be differentiated from a bacterial skin infection such as impetigo. Eczema molluscatum, unlike herpetic eczema, is a harmless complication that is rare.
Scientists believe that one of the important reasons for skin infection in patients with atopic dermatitis is the deficiency of antimicrobial peptides in the skin, which are necessary to protect the body against bacteria, viruses and fungi [5]. It is believed that infectious skin complications in atopic dermatitis are accompanied by certain immunological disorders: in bacterial infections - a deficiency of epidermal antimicrobial peptides and an imbalance of T-helper cells (Th1/Th2) - in the case of viral skin lesions [5]. According to recent data, in patients with atopic dermatitis with a complication such as herpetic eczema, significantly lower expression of antimicrobial peptides was found in skin keratinocytes [5].
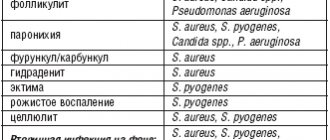
We list the skin infections that most often can complicate the course of atopic dermatitis and their causative agents:
- superinfection, folliculitis, furunculosis - Staphylococcus aureus; herpes simplex, herpetic eczema - herpes simplex virus type 1;
- genital warts, common warts, plantar warts - human papillomavirus;
- molluscum contagiosum - molluscum contagiosum virus;
- “head and neck dermatitis” - Malassezia furfur.
However, the possibility of developing such complications should be considered not only in the case of a clinically pronounced stage of exacerbation of atopic dermatitis, but also in the absence of a response to appropriate therapy. High colonization of the skin with S. aureus or a fungal infection can occur in the absence of a clear clinical picture of the disease.
According to M. Furue et al., who observed 1271 patients with atopic dermatitis for 6 months (including 210 young children, 546 children and 515 adults), the following complications were diagnosed: herpetic infections and/or Kaposi's dermatitis in 2.4% young children, 2.5% older children and 3.5% adults; association of atopic dermatitis with molluscum contagiosum in 7% of young children, 9% of children and 0.2% of adults [8].
Domestic experts point to the formation of complicated forms of atopic dermatitis in a much larger number of cases: in 25–34% of children suffering from atopic dermatitis [7].
The participation of microbes and viruses in the development of exacerbations and recurrent severe atopic dermatitis justifies the need for a differentiated approach to complex therapy for such patients. Let us dwell on the main stages of treatment of complicated forms of atopic dermatitis in children. We will talk about external, etiotropic and immunomodulatory therapy [7].
External therapy
Let us recall that the key point in the treatment of any forms and stages of atopic dermatitis is auxiliary basic therapy: regular use of cleansing and moisturizing products of the dermatocosmetic line [1]. The goal of this approach is to limit bacterial growth and restore skin barrier function.
When a child with atopic dermatitis is diagnosed with an active bacterial skin infection, treatment should include proper skin care (cleansing/hydration, antiseptics) and topical and/or oral antibiotics.
- For pustular rashes, it is better to use local baths with the addition of a solution of potassium permanganate until a light pink color is achieved (for infants - 10 ml of a 3% solution per 1 liter of water), lasting 15–20 minutes.
- Pustular rashes should be immediately extinguished with water (for children under 2 years of age) and alcohol solutions of aniline dyes: Castellani liquid, fucorcin, brilliant green solution or other antiseptics.
- Skin cleansing is carried out by taking a short bath or shower with a water temperature of 35–36 ° C and a soft washing base (pH = 5.5) that does not contain alkali (Bodygel, Mustela StelAtopia for bath, Atoderm mousse and etc.).
- After swimming or a bath, it is necessary to dry the skin with a towel without rubbing it, and apply a moisturizing cream (Topicrem, Exomega, Atoderm, etc.), and etiotropic drugs in combination with anti-inflammatory drugs to the areas of skin lesions.
Etiotropic therapy
For bacterial infections with exudation and oozing of the skin, topical antibiotics are used. It has been established that the growth of colonies of microorganisms, which are the most common causative agents of skin infections (including S. аureus, Streptococcus pyogenes, S. epidermidis, Corynebacterium spp.), is most effectively suppressed by fusidic acid [9]. In addition, the concentration of this antibiotic after a single application, in particular fucidin ointment, is 2.2% in the skin (in the epidermis - ~430 µg/ml, in the dermis - 286 µg/ml and subcutaneous fat - ~109 µg/ml) ; for comparison: the penetration ability of erythromycin is 0.3%, tetracycline - 0.28%, mupirocin (Bactroban) - 0.02%. In other words, fusidic acid penetrates the skin 100 times better than mupirocin, and 8 times better than tetracycline and erythromycin. It has been shown that fusidic acid penetrates even into devascularized areas and necrotic tissues, and its bioavailability is 90%.
Since in atopic dermatitis, eczematous skin lesions, in particular areas of exudation and excoriation, represent a favorable environment for the proliferation of S. аureus, it is believed that in the treatment of the disease it is preferable to use a combination of a topical glucocorticosteroid with an antibiotic. This will break the vicious circle: S. aureus reduces the effectiveness of corticosteroids through the production of staphylococcal toxin, while corticosteroids suppress inflammation.
Thus, the pathogenetic role of bacteria in the development and maintenance of allergic inflammation in atopic dermatitis has been proven, which justifies the need for the use of combination drugs containing topical corticosteroids and antibacterial agents. It has been shown that the use of such drugs can more effectively combat the clinical signs of atopic dermatitis than therapy with only one external corticosteroid. Thus, in two randomized clinical trials (from 34 to 207 patients), the effectiveness of topical application of various combination drugs containing antibacterial agents in combination with topical corticosteroids and monotherapy with topical corticosteroids was compared in patients with atopic dermatitis with skin manifestations of secondary infection [10, 11 ]. Clinical improvement was observed in 54–95% of participants, with no statistically significant differences in subjective and objective data depending on the use of various combination drugs. However, in the group using fusidic acid–hydrocortisone acetate (Fucidin G), clinical improvement occurred faster than in the group using miconazole–hydrocortisone [10], and the laboratory confirmed positive effect of treatment in the group using betamethasone valerate–fusidic acid (Fucicort) was higher than in the group where miconazole-hydrocortisone was used [11].
This approach—the topical use of an antibiotic and a cream—the mild corticosteroid hydrocortisone—led to a significantly earlier regression of the symptoms of skin inflammation in mild to moderate atopic dermatitis [12]. The administration of a cream containing an antibiotic and a corticosteroid seems absolutely necessary in the case of clinical manifestations of skin infection (wetting eczema). It is advisable to use such a drug in a short course (up to 1–2 weeks) in order to avoid the development of resistance to S. аureus [13]. In this case, for use on the face, skin folds, armpits, groin area, and open areas of the body, it is preferable to choose a combined drug in the form of a cream—a mild corticosteroid and an antibiotic (for example, fusidic acid + hydrocortisone acetate (fucidin G), 2–3 times per day in the form of light applications). In the case of acute and chronic forms of dermatitis, localized in areas with thick skin (palms and feet), resistant to weak topical corticosteroids, it is more advisable to prescribe an ointment form of a combination drug containing a corticosteroid of medium/high activity (for example, fusidic acid/betamethasone valerate (Fucicort) , celestoderm B with garamycin, etc.) 2–3 times a day.
However, studies have shown that skin colonization with S. aureus reoccurred 2–4 weeks after completion of treatment with a combination of topical corticosteroid and antibiotic. This is explained primarily by the fact that even when highly sensitive antibiotics are used, it is very difficult to achieve complete eradication of S. аureus. The maintenance of skin infection is facilitated by such factors as the possibility of transmission of S. aureus from parents who are in direct contact with a sick child, as well as the content of S. aureus in the nasal mucus of the patient himself.
If topical antibiotics are ineffective, as well as atopic dermatitis complicated by a bacterial infection (for example, impetigo), occurring with fever, intoxication, inflammatory changes in the blood, the administration of a broad-spectrum antibiotic orally (cephalosporins 1–3 generations, macrolides, aminoglycosides) is indicated for 7– 10 days. Taking fluoroquinolones and tetracyclines is not recommended [7].
However, despite the fact that as a result of taking systemic antibiotics, the level of microbiologically confirmed colonization of the skin with S. aureus was significantly reduced, this did not contribute to the clinical improvement of severe atopic dermatitis in children [14].
The ability to significantly reduce the colonization of S. aureus and the frequency of skin infections has also been described in relation to drugs of a new class of non-steroidal topical immunosuppressants - the calcineurin inhibitors tacrolimus and pimecrolimus (Elidel) [1, 4]. Thus, as a result of long-term use of pimecrolimus in children aged 3–23 months of life suffering from atopic dermatitis, significantly fewer cases of skin infections were noted [15]. This fact further confirms the important role of Th2-mediated skin inflammation and bacterial colonization, in which the relationship between cytokines, adhesion molecules and antimicrobial peptides plays a huge role [4, 16]. Another immunosuppressive drug, which also works by inhibiting calcineurin, is cyclosporine. This drug has the ability to reduce the number of S. aureus on the skin of patients with atopic dermatitis, which is most pronounced in patients who simultaneously have a high degree of colonization of the microbe and clinical manifestations of a bacterial skin infection [17]. However, the use of this drug is limited in pediatric practice.
For a fungal infection confirmed microbiologically, the following are prescribed: systemic antifungal agents (fluconazole (Diflucan) from the neonatal period, children over 2 years old can be prescribed terbinafine (Exifin), itraconazole (Orungal), ketoconazole - from 12 years old) for 7-14 days in combination with local therapy.
Exifin inhibits the biosynthesis of ergosterol in the fungal cell, thereby promoting the accumulation of squalene inside the cell and its death. The drug does not affect the metabolism of hormones or other drugs; in low concentrations it has a fungicidal effect on dermatophytes, molds and some dimorphic fungi. Depending on the type of yeast, its effect can be fungicidal or fungistatic.
Ketoconazole and itraconazole inhibit the production of interleukin-4 and interleukin-5 and the synthesis of ergosterol, which leads to a nonspecific anti-inflammatory effect and a decrease in the level of specific IgE to Malassezia furfur [5].
In case of combined skin lesions of patients with atopic dermatitis with a bacterial and/or fungal infection, the most optimal drugs of choice are combination agents: Triderm, Akriderm GK. Triderm in the form of an ointment is applied to the skin of the torso and limbs, and in the form of a cream - on delicate areas of the skin (in the area of folds, forearms). In pediatric practice, Triderm cream is mainly used. The drug is applied in a thin layer to the affected areas of the skin 2 times a day, the course of treatment averages 7–12 days.
As is known, topical corticosteroid therapy is the standard treatment for exacerbations of atopic dermatitis. However, the powerful anti-inflammatory effect inherent in these drugs may increase the skin's sensitivity to bacterial and fungal infections, which is an obstacle to long-term use of topical hormonal agents in the presence of these infections. In addition, children are more sensitive to topical corticosteroids due to their high cutaneous absorption; the latter is also caused by dry skin [1]. However, there are suggestions that the use of only monotherapy with topical antibiotics or fungicidal drugs contributes to skin sensitization and exacerbation of allergic inflammation with the development of candidiasis infection [18].
In all cases, the doctor should individually select medications for patients with atopic dermatitis, taking into account the course of the disease and the condition of the skin.
For herpes infection:
- it is necessary to control the factors that provoke the disease (colds, increased insolation, psychological stress, fatigue, etc.);
- in case of viral skin lesions, the use of topical corticosteroids is contraindicated;
- In pediatrics, only one antiherpetic drug is used - acyclovir (Zovirax). Parents of children with recurrent herpes infections are reminded of the need to use acyclovir immediately when the first symptoms of the disease appear (tingling of the skin);
- patients with atopic dermatitis, suffering from recurrent herpes simplex, herpetic gingivostomatitis, as well as in the case of diagnosing the most severe and life-threatening complication - Kaposi's eczema herpetiformis - are prescribed oral acyclovir. The duration of the course depends on the severity of the child’s condition and is 7–14 days [5, 7]. Patients with recurrent disease require prophylactic therapy with acyclovir. According to the latest data, after starting antiviral therapy, in order to quickly restore the skin barrier function, it is advisable to continue treatment with topical immunomodulators (tacrolimus, pimecrolimus) [5].
For molluscum contagiosum:
- the rashes are opened under aseptic conditions by piercing with a sterile needle (the needle is inserted from the side, parallel to the skin) and extinguished with a 5% alcohol solution of iodine. After the necessary training, the child's parents can perform this procedure at home on their own;
- practice cryodestruction;
- Isolation of a sick child is necessary.
Immunomodulatory therapy
In cases where patients with atopic dermatitis are diagnosed with a recurrent bacterial, fungal and/or viral infection, as well as if they have foci of chronic infection that are resistant to standard therapy, immunomodulatory therapy is indicated, which should be carried out under the control of immunological parameters. In pediatric practice, the most widely used is lycopid, an immunomodulator that has the ability to influence the main populations of cells of the immune system (macrophages, T- and B-lymphocytes), which is probably due to the presence of specific intracellular receptors for glucosaminylmuramyl dipeptide [7, 18]. . In its structure, lycopid is a synthetic analogue of the main fragment of peptidoglycan of the cell wall of all known bacteria (muramyl dipeptide). Activation of macrophages under the influence of lycopid leads to increased synthesis of pro-inflammatory cytokines (interleukin-1, tumor necrosis factor a, colony-stimulating factors), as a result of which phagocytosis, proliferation and differentiation of T- and B-lymphocytes are activated, the synthesis of immunoglobulins is enhanced, cytotoxicity increases, and leukopoiesis is stimulated .
A study by S. Yu. Rezaikina, conducted in patients with atopic dermatitis, revealed a predominant decrease in the functional activity of neutrophil phagocytosis (changes in the oxygen metabolism of neutrophils), which was restored when taking licopid [20]. As a result of the use of licopid in complex therapy of patients with moderate atopic dermatitis, the frequency of exacerbations of the disease significantly decreased and a pronounced correction of altered laboratory parameters was observed.
Likopid is prescribed to children aged 1 to 16 years orally in the form of 1 mg tablets. For the treatment of purulent-inflammatory skin diseases, the daily dose of the drug is 1 mg for 10 days. When treating herpes infection, the drug is prescribed orally at a dose of 1 mg 3 times a day for 10 days. Contraindications to the use of licopid: pregnancy, individual intolerance to the drug. In some cases, side effects may occur such as an increase in body temperature to 37.9°C (this is short-term, goes away on its own and does not require discontinuation of the drug). For adults, Lykopid is prescribed orally 30 minutes before meals (10 mg tablets) and sublingually (1 mg tablets) depending on the severity of the disease.
Isoprinosine (inosine pranobex) is characterized by a dual effect - antiviral (due to suppression of the replication of DNA and RNA viruses) and immunomodulatory (due to the inosine complex, the production of interleukins, the chemotactic and phagocytic activity of monocytes and macrophages is enhanced, the synthesis of antibodies increases and the proliferation of T-lymphocytes increases, T helper cells, natural killer cells). Indications for the use of isoprinosine are all viral skin infections in children over 1 year of age suffering from atopic dermatitis (molluscum contagiosum, herpes infection, vulgar warts, human papillomavirus infection). Isoprinosine is prescribed 1 tablet per 10 kg/body weight per day, in 3-4 doses over 10-14 days - depending on the severity of infectious diseases; If necessary, the course of treatment is repeated.
According to L.V. Luss, the inclusion of another immunomodulator, polyoxidonium, in the complex therapy of patients with atopic dermatitis and bronchial asthma, occurring in combination with signs of secondary immune deficiency and resistant to therapy, allows achieving a high clinical effect [21].
Among children suffering from atopic dermatitis, cases of scabies are common. In such cases, the course of atopic dermatitis is accompanied by severe persistent itching of the skin, and often by infection.
When scabies occurs, treatment includes:
- treatment of persons in contact with the patient with anti-scabies drugs;
- disinfection of things and bedding. The premises are wet cleaned or disinfected by employees of the sanitary and epidemiological station on the day of diagnosis and after completion of treatment. Medical control is carried out for 1.5 months;
- applying an aerosol preparation a-steam to the surface of clothing, furniture, bedding that cannot be boiled or otherwise treated;
- prescribing to the patient one of the following anti-scabies drugs:
– spregal – used in all age groups and has no contraindications; sprayed in the evening onto the patient’s skin from the neck to the soles; The drug is left for 12 hours, after which the child is thoroughly washed. If necessary, it is possible to reuse the drug 4–10 days after the initial treatment;– benzyl benzoate - 20% ointment is applied to the skin on the first, second, fourth day, also with a change of linen, clothes, and cleaning of the room;
– to treat the skin you can also use 33% sulfur ointment, Medifox;
- for atopic dermatitis complicated by scabies, it is necessary to use antihistamines, topical corticosteroids, including those combined with antibacterial drugs.
Thus, microbial colonization and superinfection of the skin (for example, S. aureus, Malassezia furfur) may play a role in exacerbations of atopic dermatitis, which justifies the need for additional prescription of antimicrobial agents to patients. Infectious agents are also involved in the development and maintenance of chronic allergic skin inflammation in atopic dermatitis. As a rule, this course of the disease is characterized by frequent relapses and a severe course. Timely diagnosis of skin infections and prescription of optimal etiotropic therapy are extremely important for achieving clinical improvement in the condition of patients with atopic dermatitis.
Experts on atopic dermatitis emphasize that etiotropic therapy can be stopped only after stopping the infectious process and cleansing the skin [1]. At the same time, treatment with anti-inflammatory drugs should be continued (according to indications, short-course topical corticosteroids, long-term calcineurin inhibitors) along with the continuous use of moisturizers to hydrate the skin [2, 5].
Literature
- Ellis C., Luger T., Abeck D. et al. New clinical data and modern strategies for the treatment of atopic dermatitis // Allergology. 2003. No. 4: 50–58.
- Leung D. Infection in atopic dermatitis // Curr Opin Pediatr 2003; 15: 399–404.
- Leung D. Presence of IgE antibodies to staphylococcal exotoxins on the skin of patients with atopic dermatitis. Evidence for a new group of allergens // J Clin Invest. 1993; 92:1374–80.
- Hank P., Leung D. Tacrolimus (FK506): new treatment approach in superantigen-associated diseases like atopic dermatitis? // J Allergy Clin Immunol. 2001; 107:391–2.
- Boguniewicz M., Schmid-Grendelmeier P., Leung D. Atopic dermatitis // J Allergy Clin Immunol. 2006; 118:40–43.
- Malanicheva T. G., Salomykov D. V., Glushko N. I. Diagnosis and treatment of atopic dermatitis in children complicated by mycotic infection // Russian Allergological Journal 2004. No. 2. P. 90-3.
- Atopic dermatitis and skin infections in children: diagnosis, treatment and prevention: a manual for doctors. M., 2004. 104 p.
- Furue M., Terao H., Rikihisa H. et al. Therapeutics clinical dose and adverse effects of topical steroids in daily management of atopic dermatitis // Br J Dermatol. 2003; 148: 128–32.
- Carr W. Fusidic acid in patients with skin and soft tissue infections// Eur J Clin Res. 1994; 5:87–95.
- Poyner T., Dass B. Comparative efficacy and tolerability of fusidic acid/hydrocortisone cream (Fucidin H cream) and miconazole/hydrocortisone cream (Dactacort cream) in infected eczema // J Eur Acad Dermatol Venereol. 1996; 7 (suppl. 1): 23–30.
- Wilkinson J., Leigb D. Comparative efficacy of betamethasone and either fusidic acid or neomycin in infected or potentially infected eczema // Curr Ther Res. 1985; 38: 177–82.
- Ramsay C., Savoie J., Gilbert M. et al. The treatment of atopic dermatitis with topical fusidic acid and hydrocortisone acetate // J Eur Acad Dermatol Venereol. 1996; 7 (suppl 1): 15–22.
- Menday A., Noble W. Topical betamethasone/fusidic acid in eczema: efficacy against and emergence of resistance in Staphylococcus aureus // J Dermatol Treat. 2000; 11: 143–149.
- Boguniewicz M., Sampson H., Bina P. et al. Effects of antibiotic treatment on S. aureus colonization in atopic dermatitis // J Allergy Clin Immunol. 1999; 103:179.
- Paul C., Cork N., Rossi A. et al. Safety and tolerability of 1% pimecrolimus cream among infants : experience with 1133 patients treated for up to 2 years // Pediatrics. 2006; 117: 118–28.
- Ong P., Ohtake T., Brandt C. et al. Endogenous antimicrobial peptides and skin infections in atopic dermatitis // N Eng J Med. 2002; 347:1151–60.
- Bunikowski R., Mielke M., Brautigam M. et al. Effect of oral cyclosporin A in children with Staphylococcus aureus-colonized vs S aureus-infected severe atopic dermatitis // Pediatr Allergy Immunol. 2003; 14(1): 55–9.
- Wong V., Croce C., Schonfeld S. et al. Use and abuse of topical corticosteroids in infections of the skin and related structures // J Drugs Dermatol. 2003; 2: 268–76.
- Smirnova G.I. Modern approaches to the treatment and rehabilitation of atopic dermatitis complicated by secondary infection // Allergology and immunology in pediatrics. 2004: 1: 34–39.
- Rezaikina S. Yu. Likopid (glucosaminylmuramyl dipeptide) in complex therapy of patients with atopic dermatitis based on a study of opsonophagocytic reactions of neutrophils: abstract. dis. ...cand. honey. Sci. M., 1999. 17 p.
- Luss L.V. Principles of using immunomodulatory therapy in patients with atopic diseases occurring in combination with secondary immune deficiency syndrome // Allergology and Immunology. 2002. No. 3: 159–63.
D. Sh. Macharadze , Doctor of Medical Sciences, Professor of RUDN University, Moscow
Diet for dermatitis
For allergic dermatitis, a special diet and balanced nutrition are included in the patient’s health system. Properly organized nutrition and hypoallergenic foods in the patient’s diet are the key to preventing new doses of allergens from entering the body. Before visiting a doctor, you must independently determine the minimum list of products that can be consumed without the risk of exacerbating allergic reactions.
Products that often cause allergies:
- Protein - pork, fatty beef, milk, chicken egg, fish, seafood, caviar, smoked meats, delicacies, stewed meat;
- Vegetable - legumes, sauerkraut, pickled vegetables, all red berries, all tropical fruits, mushrooms, dried fruits (dried apricots, raisins, dates, figs);
- Drinks – sweet carbonated water, filled yoghurts, cocoa, coffee;
- Desserts – caramel, marmalade, chocolate, honey;
- Seasonings, sauces (ketchup, mayonnaise, soy sauce), canned soups, and any finished products containing dyes, emulsifiers, preservatives and other food additives
Moderately allergenic products:
- Drinks – black tea, green apple juices, herbal infusions;
- Protein – lamb, horse meat, rabbit;
- Vegetables - rye, buckwheat, corn, green fruits, potatoes;
- Desserts - yoghurts, mousses, curds.
Low allergenic products:
- Protein - some types of fish (cod and sea bass), lean veal, offal (liver, tongue), low-fat cottage cheese, butter;
- Vegetable - cereals (rice, pearl barley), green salad, cucumbers, zucchini, rutabaga, fresh cabbage, spinach, vegetable oil, pears, gooseberries, white cherries and white currants;
- Desserts – dried fruits from dried pears and apples, prunes.
- Drinks – fermented milk without added dyes, pear and apple compotes, rhubarb decoctions, low concentration green tea, still mineral water;
For dermatitis without an allergic load, proper nutrition is more important. The main principle is to include low-calorie, easily digestible foods in the diet. There are no universal recommendations. You can learn more about the products recommended for you personally from your doctor or nutritionist.