Urticaria is a group of diseases (mainly of an allergic nature), the characteristic symptom of which is a rash on the skin in the form of red blisters.
In Russia, urticaria is very common - from 10 to 20% of the population have experienced its manifestations at least once in their lives. Moreover, in the majority it occurs in an acute form (70-75%), in the rest it takes a chronic course. WHO (World Health Organization) predicts that the 21st century will be the century of allergies. Every year the number of patients with one form of allergy or another increases by 5%.
Causes of the disease
The causes of urticaria in children are:
- sensitivity to allergens;
- consumption of allergens in food, their inhalation;
- taking certain medications;
- bites of some insects;
- tactile contact with the allergen (urticaria in a child may appear after sleep due to a reaction to the dye in the bedding fabric or washing powder). Source: L.V. Luss Causes and treatment of urticaria in children, swelling in children // Medical Council, 2015, No. 14
Upon contact with an allergen, inflammation occurs, fluid accumulates in the body tissues, and a rash and swelling appear. This reaction of the body is an attempt to reduce the amount of harmful substances.
Chronic urticaria, which can appear as early as one year of age, occurs due to:
- chronic or long-term gastrointestinal diseases;
- chronic inflammation;
- viral infections;
- parasite infestation;
- fungal diseases;
- disturbances in the functioning of the nervous system;
- hereditary predisposition.
The disease can be provoked by overheating or hypothermia of the skin, exposure to UV or water, when combing or injury by elements of clothing, due to severe stress. With such urticaria (it is called “cholinergic”), children do not have an elevated body temperature, and external manifestations quickly disappear (in a few minutes, maximum half an hour). Source: I.I. Balabolkin. Urticaria in children: clinical and pathogenetic variants, diagnosis and treatment // Russian Pediatric Journal, 2022, 20(2)
The mechanism of occurrence of urticaria (pathogenesis)
The human body contains mast cells or mast cells, which are specific elements of connective tissue. They are the central element in the development of urticaria, activators of inflammation. When an allergen enters the body for the first time and in small doses, the child does not experience any external manifestations or reactions, but sensitization occurs, which can be represented as the first acquaintance with the allergen, resulting in the production of histamine. It is this substance that causes redness, swelling and other inflammatory factors. It gradually accumulates in mast cells, and when its amount reaches a critical threshold, the cell membrane is destroyed with the release of histamine into the bloodstream and a subsequent cascade of pathological changes in the body.
Diagnostic methods
When this disease develops, the patient or his parents are interviewed and the symptoms are analyzed.
The doctor can make a preliminary diagnosis after examining the child’s skin. A rash with urticaria is difficult to confuse with another. However, to exclude errors and establish the cause, tests are prescribed:
- stool analysis, which will help identify parasites - they can be pathogens;
- general blood test - identifies or excludes inflammatory and immune processes;
- allergy tests - skin tests to identify the pathogen;
- liver tests - to determine liver function and exclude its pathologies.
Thyroid function may be tested because the disease can be caused by hypo- or hyperthyroidism.
Features of the diet for urticaria
Nutrition is a very important part of successfully recovering from the disease. Regardless of the cause of the rash, it is recommended to adhere to a hypoallergenic diet during an exacerbation. Diet principles:
- Complete exclusion of the product that caused the allergic reaction and any food similar in nature.
- Refusal of products containing chemical additives and preservatives, which can aggravate the course of the disease.
- Refusal of products with dyes, even if they are natural.
- Exclusion of generally recognized allergenic products (nuts, seafood, chocolate, honey).
- Food must be balanced and contain the necessary complexes of macro and microelements.
- Avoid alcohol, as it aggravates the symptoms of the disease.
Types of disease
In medicine, there are five main forms of this disease:
- chronic with periodic exacerbations;
- acute, arising and spreading rapidly;
- allergic (affects 70% of children);
- pseudo-allergic (provoked by disturbances in the functioning of the liver and digestive organs);
- hereditary non-allergic (accompanied by Quincke's edema, similar to allergic). Source: L.P. Sizyakina, A.A. Lebedenko, C.B. Maltsev, A.N. Posevina, L.A. Averkina Urticaria in children: a modern view of the problem // Medical Bulletin of the South of Russia, Reviews, 2015
Let's take a closer look at the types of urticaria, depending on the triggering factor:
- Medicinal. A type of drug allergy is a reaction to certain drugs. The most common provocateurs are iodides, streptomycin, sedatives, NSAIDs, and drugs containing gold. The rash may be accompanied by a runny nose, conjunctivitis and bronchial asthma. To cure this form of urticaria, you need to eliminate the allergen, adjust the diet, removing the brightest allergens from it - citrus fruits, red vegetables and fruits, nuts, cow's milk, fish.
- Mechanical – appears when pressure is applied to the skin. Its causes have not been reliably studied, but the disease is associated with skin sensitivity, heredity and the condition of the blood vessels. Divided into several subspecies:
- dermographic – develops quickly due to friction or pressure, often caused by wearing tight clothing;
- cold - a reaction to contact with something cold, drinks or foods;
- heat – the rash appears when the environment is hot;
- solar - occurs during prolonged exposure to the sun, manifested by swelling and red spots on the skin;
- aquagenic - rare, but very dangerous, appears upon any contact with water;
- papular - the result of an insect bite;
- cholinergic - a rash appears when the child is nervous and sweats a lot.
- Generalized. It differs in that the rash spreads throughout the body, including the mucous membrane of the oropharynx, which makes breathing difficult. Quincke's edema may develop. Such urticaria appears in children with atopic diseases and can be caused by antibiotics and NSAIDs. Rarely are food products allergens.
- Idiopathic. The cause is unknown, but itchy blisters appear regularly over a period of 6 weeks at varying intervals. The process is considered chronic. Spontaneous occurrence and the lack of diagnostic methods make it difficult to control the course of the disease, treatment and prevention.
Types of urticaria
There are several classifications of urticaria.
1. By time:
- acute – lasts up to 6 weeks;
- chronic – more than 6 weeks.
2. By nature:
- allergic (immune) - realized through the development of an immune reaction, often combined with other allergic diseases (bronchial asthma, rhinitis, conjunctivitis, dermatitis, etc.);
- non-allergic - through the direct release of histamine.
3. Due to:
— allergic urticaria
may cause:
- Food;
- taking medications;
- insect allergens (insect allergy);
- pollen allergens.
— non-allergic
form of the disease occurs due to a direct effect on the mast cell:
- physical factors - such as cold, heat, ultraviolet radiation, radiation, vibration, compression;
- chemical (provoking factors are solvents, acids, alkalis and other chemicals);
- certain medicines, such as aspirin;
- infectious agents - viruses (adenoviruses, Epstein-Bar virus, enteroviruses), streptococci, helminths, Helicobacter pylori;
- for systemic and other chronic diseases (rheumatoid arthritis, systemic lupus erythematosus);
- with a sharp increase in the level of histamine and other active substances in the blood due to the large consumption of foods high in them: eggplants, canned food, nuts, bananas, chocolate and others.
Hereditary, psychogenic, and idiopathic urticaria (this is the name for a disease whose cause has not been established) is also possible.
The wide variety of factors and similar developmental mechanisms of individual species make it difficult to find the cause. Most often, this requires the help of a specialist.
Treatment methods for urticaria in children
This disease should be treated depending on its form. The pseudoallergic variety requires examination for the underlying disease. Allergic – allergen exclusion and immunotherapy.
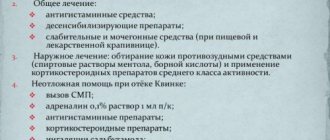
In the acute period:
- eliminate contact with the allergen;
- the child is prescribed a hypoallergenic diet for several days;
- remove the allergen from the body, prescribe plenty of fluids;
- use sorbents and antihistamines (types and dosage regimen are determined only with a doctor);
- for severe swelling, a specialist may prescribe a diuretic;
- Prescribe antipruritic ointments for the arms, legs, or other areas of the child’s body that are prone to hives.
Parents should carefully monitor the cleanliness of the house and promptly wash clothes and bedding with hypoallergenic products.
How to recognize the disease and identify its causes?
Urticaria on the body of an adult has characteristic signs:
- The rash appears immediately after exposure to the allergen, within a few minutes, and goes away just as quickly, often within a day.
- The rashes are most often localized on the arms, legs, and body, but can occur on any part of the body.
- The rash is characterized by the appearance of blisters that rise above the surface of the skin, pale pink or reddish in color, with clear contours. Blisters can merge into large spots.
- The rash is accompanied by severe itching3.
You can identify the cause of the rash yourself if you track the factor that causes specific symptoms to appear. However, the connection is not always obvious, so laboratory tests have to be carried out to accurately determine the allergen. They are called provocative tests. Investigations should not be performed during an exacerbation4.
Are there any complications?
Acute urticaria in children can have a dangerous complication - Quincke's edema (giant urticaria, angioedema). It consists of swelling of the mucous membrane of the respiratory tract. The child has coughing attacks and has difficulty breathing. Very young children may experience swelling of the gastrointestinal mucosa (the reaction to this is vomiting). In severe cases, the membranes of the brain and nervous system are affected. Any of these conditions is very dangerous and can be fatal. Therefore, it is very important not to delay visiting a doctor if there are signs of illness.
Important! Many parents do not know what to do with Quincke's edema. You should immediately give your child an antihistamine (any one from your home medicine cabinet) and call emergency medical help.
Chronic urticaria: drug of choice
XP
onic idiopathic urticaria (IU) is a skin disorder that affects 0.1–3% of the population. CHI usually affects people of working age, since the onset of the disease often occurs in the second and fourth decades of life, with at least one episode of urticaria occurring throughout life in 15–20% of both children and adults. Chronic urticaria is diagnosed twice as often in middle-aged women, which is due to the presence of dishormonal and neuroendocrine disorders [1, 2]. In approximately 50% of patients, chronic urticaria is combined with Quincke's edema [3]. In patients with CIC, the quality of life is significantly impaired, which is expressed in sleep disturbances, changes in the emotional background, and the occurrence of certain problems in everyday life [4, 5]. Urticaria can be either an independent disease or a symptom of a number of diseases. Clinical manifestations of urticaria are the result of the release and synthesis of mediators, mainly by mast cells located in the skin, which is caused by immune, non-immune, and idiopathic factors. The primary element in urticaria is a blister - urtica. When pressed, the urticarial element turns pale, which indicates the presence of dilated blood vessels and edema in the skin lesions. Urticarial rash is accompanied by itching, which intensifies at night and lasts from a few minutes to 48 hours [6]. After a specified period, the elements of the rash disappear without a trace, however, new rashes may appear at different times in other parts of the body (Fig. 1) [7]. At the histological level, it is swelling and perivascular infiltration of lymphocytes, mast cells, eosinophils and neutrophils of the epidermis and upper layer of the dermis with compression of veins and lymphatic vessels. Urticaria and Quincke's edema can develop together or separately. If the swelling involves the skin and subcutaneous tissue, the condition is called angioedema, or angioedema. With urticaria, only the superficial layers of the skin are involved in the process. With Quincke's edema, the itching is less pronounced, but the pain and burning sensation are similar. Urticaria can occur on any part of the body, while angioedema occurs most often in areas rich in connective tissue, such as the face, limbs and genitals. Unlike other forms of edema, there is no symmetry in its location (Fig. 2) [8].
There are acute (up to 6 weeks) and chronic (more than 6 weeks) urticaria. When rashes appear repeatedly, recurrent urticaria is diagnosed. Urticaria is most often associated with food and drug allergies, and can also be mediated by helminthic infestation or viral infection. Moreover, in half of the patients the cause of the urticarial rash cannot be identified - such urticaria is designated as idiopathic. It was previously believed that urticaria was mostly idiopathic, accounting for 80–95% of all urticaria cases. In the literature of recent years, the name “idiopathic urticaria” has become less and less common; the term “chronic urticaria” has become more common, since during many years of observation of patients with a previously established diagnosis of “idiopathic urticaria”, many researchers identified an autoimmune genesis in 35-55% of cases [7, 8]. Chronic urticaria can also be mediated by parasites, which is explained by their stimulating role in the development of the IgE immune response, however, clinical resolution of urticaria by eliminating parasites is achieved only in 8–16% of cases [9]. One of the reasons for increased activation of mast cells in patients with chronic urticaria is often identified infectious and inflammatory pathology of the digestive tract. Helicobacter pylori infection has also been implicated in chronic urticaria. It has been established that the frequency of its detection among patients with urticaria and in the population is the same. However, the immune response to H. pylori may differ in patients with urticaria. Moreover, an analysis of existing studies revealed that remission of urticaria is more likely in cases where antibacterial therapy leads to eradication of H. pylori [10]. In some patients, a combination of chronic urticaria with autoimmune pathology of the thyroid gland was found, accompanied by the detection of antithyroid antibodies in the serum, which may be a marker of an autoimmune nature, however, the mechanisms of the connection of antithyroid autoantibodies with mast cell activation remain unclear [11]. With CIC, urticarial elements persist longer than with various types of physical urticaria - usually up to 8-12 hours and are accompanied by more severe itching, especially in the evening and at night. With CIC, 25–45% of patients show signs of an autoimmune disease. In such patients, the level of serum immunoglobulin E (IgE) is significantly lower, and severe itching is added to the abundant and widespread urticarial rash [12]. When examining skin biopsies in patients with CIC and the presence of FcεRI/IgE antibodies, perivascular infiltrates are often detected, mainly consisting of neutrophils, eosinophils and mononuclear cells [13, 14]. Almost a third of patients with CIC have autoimmune reactions to thyroid tissue. However, most of them do not have any clinical symptoms of damage to the thyroid gland and changes in hormone levels; there is a decrease or disappearance of urticaria symptoms after the administration of L-thyroxine [11, 14–16]. In addition to assessing the history, clinical symptoms of the disease and its course, laboratory tests help in the differential diagnosis of chronic urticaria: • skin tests or determination of specific IgE antibodies in the blood can reveal the connection of the rash with food, medications, insect bites, plant pollen, animals; • sowing in the presence of a chronic focus of inflammation to isolate a culture of bacteria and determine their sensitivity; • study of thyroid function; • stool analysis for helminth eggs; • tests for the presence of autoantibodies; • complete blood count, ESR, determination of C-reactive protein; • detection of H. pylori [17] . The main drugs in the treatment of chronic urticaria are antihistamines. Despite the fact that first generation antihistamines (diphenhydramine, hydroxyzine, etc.) effectively eliminate the symptoms of urticaria, their use is associated with a large number of side effects. These include drowsiness, anticholinergic effect (dry mucous membranes, dizziness, constipation, urinary retention, etc.), impaired memory and attention, which can persist for 24 hours after taking the drug. According to the International Guideline for the Treatment of Urticaria (EAACI/GA2LEN/EDF/WAO management guideline), first generation antihistamines (sedatives) should not be used as first-line treatment for patients with urticaria. The only exceptions can be those situations when it is impossible to use second generation antihistamines. Currently, the priority is to prescribe non-sedating antihistamines of the second generation. These drugs, devoid of the side effects inherent in first-generation antihistamines, are no less effective at blocking H1 receptors for histamine and suppressing the symptoms of urticaria, significantly improving the quality of life of patients [18, 19]. Among the “non-sedating” antihistamines, desloratadine (Elysea), which is the primary pharmacologically active metabolite of the well-known loratadine, deserves special attention. Desloratadine is a drug that enters the body in the form of an active substance, which ensures its higher safety profile. It was synthesized in 1998 and registered in Russia in 2001. Desloratadine has the ability to suppress the acute phase of the allergic response by blocking H1 receptors. In experimental studies, it was shown that desloratadine has the greatest affinity for H1-histamine receptors and slow dissociation from connection with them. Desloratadine binds noncompetitively to H1 receptors and, according to clinical studies, has 52, 57, 194 and 153 times higher activity than cetirizine, ebastine, fexofenadine and loratadine, respectively. The drug is rapidly absorbed after oral administration and is characterized by a high rate of achievement of maximum plasma concentration and a rapid onset of action (after 1.25–3.00 hours). The pharmacokinetics of desloratadine are linear and dose proportional. The half-life of the drug is 21–24 hours, which allows it to be administered once a day. Eating does not affect the rate and degree of absorption of the drug. It was found that the pharmacokinetics and bioavailability of desloratadine are the same when taking the drug on an empty stomach and after a standardized meal in healthy people (the maximum concentration on an empty stomach and after a meal was 3.30 and 3.53 ng/ml, respectively, p = 0.17). Consequently, the drug can be taken regardless of meals, which indicates the convenience of its use. Metabolism and excretion of the drug do not depend on the age and gender of the patient [20–24]. Animal studies in vitro and in vivo have demonstrated that desloratadine, by inhibiting a number of inflammatory mediators, has additional antiallergic and anti-inflammatory effects not associated with blockade of H1-histamine receptors. At physiological concentrations, the drug effectively inhibits the production of histamine-dependent proinflammatory cytokines - IL-6 and IL-8, which are known to be released from endothelial cells, basophils and mast cells, and stimulate the secretion of proinflammatory mediators, such as tumor necrosis factor α. Desloratadine affects the activation and survival of eosinophils. Eosinophils, being the key effector cells in the allergic reaction, produce cytokines, chemokines, leukotrienes and neuromodulators. In addition, desloratadine, through inverse agonism, reduces the expression of nuclear factor κB (NF-κB), known as an inducer of RANTES, a major attractant for eosinophils, monocytes and T lymphocytes, promoting eosinophil activation and histamine release from basophils. Desloratadine is more potent than other antihistamines in inhibiting the activity of NF-κB, which stimulates the release of proinflammatory mediators from basophils and mast cells. In this effect, the drug is superior to cetirizine, loratadine and fexofenadine. Recent studies have shown that desloratadine may also inhibit mast cell degranulation and subsequent histamine release. In addition, desloratadine inhibits histamine-induced P-selectin expression [25–27]. Desloratadine is characterized by a high level of safety when used. It does not cause negative changes in the cardiovascular system and other organs, does not have a hypnotic effect and does not affect cognitive functions. The drug can be used by patients with pathologies of the hepatobiliary system and kidney diseases, and is approved for use in children from 1 year of age [23, 24]. Among the second generation antihistamines, desloratadine stands out for its more than 15 years of successful experience in widespread medical use and a large evidence base. The effectiveness and safety of desloratadine in the treatment of patients with CIC has been proven by numerous randomized, placebo-controlled clinical studies. J. Ring, R. Hein, A. Gauger conducted a multicenter, double-blind, placebo-controlled study that included 190 patients with moderate to severe CIC. During exacerbation of the disease, the 1st group of patients was prescribed desloratadine 5 mg/day, the 2nd group - placebo (control). The duration of treatment reached 6 weeks. The primary efficacy criterion was the average change in the itching index during the first 7 days of treatment compared to baseline. It was found that during the 1st week in patients receiving desloratadine, the itching index decreased by 56%, and in the control group - by 22%; a more rapid regression of skin rashes was also noted than in the control group. It was found that in patients from group 1 at the end of the 1st week of treatment, the degree of sleep disturbance when using the drug decreased by 53%, and in patients from group 2 - only by 18%. After 6 weeks During treatment with the drug, the itching index decreased by 74%, and during treatment with placebo – by 48.7%. By the end of the study, patients taking desloratadine experienced an almost 80% reduction in sleep disturbance. Both patients and doctors highly appreciated the overall positive dynamics of CIC symptoms and the response to treatment with desloratadine. The frequency of adverse events was comparable in the 2 groups; no serious adverse reactions were recorded [28]. In a more recent study, 137 patients with moderate to severe CIC were randomized into 2 groups. Patients from group 1 were prescribed desloratadine 5 mg/day, and patients from group 2 were prescribed placebo for 6 weeks. By the end of the study, the itching index in the desloratadine group decreased by 1.43, and in the placebo group by 0.86 (p = 0.004). After 6 weeks the number of patients with a complete, significant or moderate response to treatment was higher in the group of patients receiving desloratadine compared to patients receiving placebo (68.8 and 36.8%, respectively). No serious adverse events were reported, and the incidence of any adverse reactions was 11.1% in the placebo group and 6.2% in the desloratadine group [29]. Another study showed that desloratadine reduced the severity of the main clinical symptoms of CIC, primarily pruritus, by 50–70%. The effect of the drug lasted up to 24 hours. A decrease in symptoms of itching at the end of the desloratadine dosing interval was observed in 45% of patients (versus 4% of those taking placebo) and after 6 weeks. admission - 69%. There was also a significant decrease in the size and number of blisters during long-term use of desloratadine. Patients noted an 80% improvement in sleep. Assessment of the quality of life in patients with CIC while taking the drug for 7 days showed a decrease in scores on the Dermatology Life Quality Index (DLQI) questionnaire from 13.4 to 9.1. In 60% of patients during the specified period, the DLQI index decreased by an average of 2 points. By the end of the study, the proportion of such patients reached 77% (p<0.0001) [30]. In Germany in 2001–2002. 77,800 patients over 12 years of age were examined. Symptoms of allergic diseases were assessed before and after treatment. As a result of treatment with desloratadine, the vast majority of patients experienced relief of symptoms, which indicated a pronounced clinical effect [31]. A clinical study involving 12,050 patients confirmed the high therapeutic efficacy of desloratadine in CIC. At the same time, the absence of sedative influence and preservation of psychomotor functions were noted [32]. A number of studies were also carried out in Russia under the leadership of Yu.V. Sergeeva, N.V. Kungurova, I.M. Korsunskaya et al., aimed at assessing the effectiveness of desloratadine in the treatment of various dermatoses accompanied by itching. Therapy with desloratadine gave a positive effect in the form of a reduction in itching or its complete regression in 90% of patients. No side effects were observed during treatment with desloratadine [33–35]. Desloratadine meets all ARIA/EAACI criteria and is recommended as the first line of treatment for allergic dermatoses [36, 37]. It has special pharmacokinetic properties: it is quickly absorbed, its bioavailability is not affected by food or juice intake. The half-life of desloratadine is 21–27 hours, which allows its therapeutic activity to remain unchanged when taken once a day (unlike other second-generation antihistamines). Moreover, a study of the compatibility of desloratadine with other drugs did not reveal any significant interactions. A distinctive feature of desloratadine from other second-generation antiallergic drugs is its triple mechanism of action: it not only blocks H1-histamine receptors, but also has pronounced antiallergic and anti-inflammatory activity by inhibiting the synthesis of many other mediators by mast cells, basophils and other cells involved in the development of inflammation [ 38]. Desloratadine inhibits the development of not only the early, but also the late phase of the allergic reaction, which is associated with the accumulation of “inflammatory cells” in the lesion. This unique pharmacological effect of desloratadine suppresses the formation of chronic inflammation, which, in the absence of adequate therapy, can lead to a protracted course of the disease. Additional confirmation of the anti-inflammatory activity of desloratadine, associated with the suppression of not only allergic inflammation, is its ability to inhibit the development of erythema when exposed to ultraviolet B-range radiation [39]. The clinical efficacy and safety of desloratadine for chronic urticaria has been proven in multicenter, randomized, placebo-controlled, double-blind studies. Efficacy in suppressing itching was observed from the first day of use of the drug and persisted over the next 6 weeks. In addition, treatment with desloratadine led to the elimination or significant reduction in the severity of symptoms of CIC such as sleep disturbances, decreased activity and performance of patients. There were no side effects [40]. One of the drugs widely used in clinical practice is Elisea (desloratadine 5 mg). Since chronic urticaria is a long-term and recurrent disease, the drug is beneficial from a pharmacoeconomic position. It has antiallergic, antipruritic and antiexudative effects. Effective relief of urticaria symptoms when prescribing Elisea at a dosage of 5 mg occurs already on the first day of treatment, continues throughout the entire period of use of the drug and consists of a rapid and persistent reduction of rash, itching, improved sleep and activity of patients during the daytime, i.e. the use of Elisea for chronic urticaria is accompanied by a significant improvement in the quality of life of patients. Elisea has virtually no sedative effect, the drug does not affect cognitive functions (reading, driving). Elisey is prescribed from the age of 12, at a dosage of 5 mg (1 tablet), once a day, regardless of meals. The duration of treatment depends on the severity and form of urticaria. The high degree of safety and good tolerability give reason to recommend Elisey for the treatment of patients suffering from chronic urticaria.
Disease prevention methods
There are no special preventive measures. However, you can minimize the risk of developing the disease by following these recommendations:
- control the child’s diet;
- exclude contacts with potential allergens - food, volatile, contact;
- have an antihistamine in your home medicine cabinet;
- buy your child loose clothes made from natural fabrics;
- do not provoke stress in the child;
- do not trigger chronic diseases.
Sources:
L.V. Luss. Causes and treatment of urticaria in children // Medical Council, 2015, No. 14
I.I. Balabolkin. Urticaria in children: clinical and pathogenetic variants, diagnosis and treatment // Russian Pediatric Journal, 2022, 20(2)
L.P. Sizyakina, A.A. Lebedenko, C.B. Maltsev, A.N. Posevina, L.A. Averkin. Urticaria in children: a modern view of the problem // Medical Bulletin of the South of Russia, Reviews, 2015
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
What else should you know about hives?
- If you've experienced a rash like this, know that you're not alone. About one in four people in the world have experienced something like this at least once.
- Women and children are most susceptible to such allergic reactions.
- 50% of cases of urticaria are accompanied by swelling of the face and larynx (Quincke's edema).
Non-food allergens that most often cause allergic rashes:
- insect bites;
- latex;
- mold;
- helminths and parasites;
- pollen of various plants;
- chemicals (detergents, pesticides);
- Sun rays;
- vibration;
- pet epithelium;
- dust;
- dust mite;
- feathers.
First, for diagnosis, an elimination diet is prescribed - a diet from which certain foods are alternately excluded. The person suffering from skin rashes is then sent for a blood test. If a lot of IgE to specific allergens is detected in it, this confirms the body’s increased reaction to them. But in a third of patients it is still not possible to determine the allergen even after several laboratory tests.
Treatment of urticaria with an unknown allergen is mainly symptomatic. Consultations with other specialized specialists are scheduled.
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with an allergist-immunologist, primary, therapeutic and diagnostic, outpatient | 1950 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
| Allergen-specific immunotherapy (ASIT) - maintenance course (excluding the cost of the drug) | 8100 rub. |
How to treat urticaria using traditional methods
The question that concerns all patients who develop urticaria is what to do and how to treat it? Whatever the cause of urticaria, treatment must begin with eliminating the cause of its occurrence. A mild form of the disease can be cured using traditional methods.
Advantages of traditional methods:
- Treatment is carried out at home;
- Natural ingredients are used;
- There is no need for large financial expenses.
Disadvantages of traditional methods of treating urticaria :
- A lot of time is spent on preparing products;
- It is dangerous to treat a severe disease with such drugs.
Polina Vasilyeva
dermatologist
| If you or your baby are experiencing urticaria in one form or another, it is important to know a few first aid rules. They consist of applying a cold compress in combination with taking 2nd generation antihistamines. If urticaria is accompanied by suffocation, hoarseness, difficulty swallowing and breathing, blueness of the face, as well as symptoms of anaphylaxis (drop in blood pressure, dizziness, loss of consciousness), you must immediately call an ambulance! The doctor will give an injection of adrenaline, which acts on anaphylaxis with lightning speed (unlike antihistamines and hormonal drugs). Also, if possible, it is necessary to eliminate the allergen as quickly as possible and provide the patient with plenty of fluids. |
Polina Vasilyeva
dermatologist
| Separately, I would like to talk about the manifestations of urticaria in pregnant and nursing mothers and figure out whether it is dangerous. The first appearance of urticaria during pregnancy is a fairly common occurrence, and the reason for this is excessive sensitivity to placental proteins, as well as concomitant pathologies during pregnancy (gestational diabetes, for example). If a woman was already “familiar” with urticaria before pregnancy, then in some cases her condition may worsen during pregnancy due to hormonal changes. It is important to remember that most often urticaria does not have any negative effect on the fetus (during pregnancy) and the newborn (during breastfeeding), but you need to be careful with taking medications (antihistamines and hormonals) during these periods. Be sure to consult with your healthcare provider. |
Children under two years of age usually suffer only from the acute form. Between the ages of 2 and 12 years, urticaria sometimes becomes chronic, but more often it still occurs in an acute form. In adolescence, the chronic form takes precedence over the acute form.