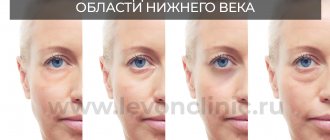
Darkening of the eye area is often a consequence of lack of sleep. But what is the reason if the darkening does not disappear even after a long sleep? The fact is that good sleep is only one of the factors that influence the darkening of the eyelids and skin around the eyes. And although dark eyelids are not dangerous, they can negatively affect the mood and self-esteem of their owner.
In order to choose the most appropriate care, it is necessary to know more about each individual case, as there are a number of possible causes. We will consider the most common cases of darkening of the eyelids in this article.
Pregnancy
During pregnancy, some women begin to experience skin changes. Melasma[1] is one of the most common effects of pregnancy on the skin. It appears as brown or gray-brown pigmentation on the face, which may appear on the eyelids.
The appearance of these spots is associated with increased levels of melanin, the pigment responsible for skin color. In those places where cells begin to produce excess amounts of melanin, pigment spots form.
Some doctors believe that the appearance of melasma during pregnancy is due to changes in hormonal levels, but the exact cause remains unknown today.
Causes of the defect
All known factors that can provoke the formation of dark circles around the eyes are divided into 3 groups:
Lifestyle
Quite often, circles under the eyes appear due to an unhealthy lifestyle:
- poor nutrition leading to vitamin deficiency;
- insufficient water consumption;
- strong insolation;
- constant lack of sleep;
- frequent stressful situations;
- sitting for many hours in front of a computer monitor.
Therefore, most people are at risk. But it is the factors of this group that are easiest to eliminate, since they are reversible and easily corrected.
Diseases of internal organs
Dark circles under the eyes can occur in people with impaired venous or lymphatic drainage. The cause of such conditions is insufficient blood supply (ischemia) and oxygen deficiency (hypoxia). As a result, metabolism is disrupted, causing insufficient nutrients to reach the cells. Therefore, dark circles are often noticeable in people with diagnosed diseases of the cardiovascular (coronary heart disease, vascular insufficiency) and bronchopulmonary (chronic bronchitis, tuberculosis, sarcoidosis, fibrosing alveolitis) systems.
In patients suffering from anemia, the number of red blood cells decreases and the concentration of hemoglobin decreases, which is why the tissues do not receive enough oxygen. At the same time, the reduced hemoglobin accumulates and gives the blood a dark color, which explains the change in color of the skin around the eyes.
Pathologies of the hepatobiliary system (cholecystitis, cholelithiasis) increase the level of bile pigment (bilirubin) in the blood. As a result, the skin in the periorbital area becomes pigmented and turns yellow-brown.
Damage to the thyroid gland (including hypothyroidism) causes a lack of oxygen in the body, which causes bruises to appear under the eyes. In this case, other signs are observed: hair loss, unbearable heat and cold, weakening of attention and memory, drowsiness, lethargy, rapid fatigue.
Diseases of the nasopharynx (sinusitis, sinusitis, chronic tonsillitis, adenoiditis) dilate the blood vessels, which leads to their excessive filling with blood and blueness of the skin under the eyes.
In acute infectious diseases accompanied by an increase in body temperature, intoxication occurs with the metabolic products of microbes. As a result, the acidity of the blood increases and acidosis develops, in which the vessels dilate and their permeability increases. Intoxication syndrome causes dehydration. On dry and thin dehydrated skin, dilated capillaries become especially noticeable, which creates the effect of dark circles.
Diseases of the adrenal glands and kidneys increase pigmentation of the skin surrounding the eyes. With chronic adrenal insufficiency (Addison's disease), the skin also darkens in natural folds (groin, palms) and in areas exposed to friction by clothing (lower back, neck). With kidney pathologies (pyelonephritis, glomerulonephritis), blue circles under the eyes become noticeable when the disease relapses due to a malfunction of the organ.
Women often suffer from hyperpigmentation during hormonal changes (during pregnancy, menopause) due to an imbalance of female sex hormones (estrogen, progesterone).
In case of inflammatory eye diseases (conjunctivitis, iridocyclitis), swelling appears under the eyes, the permeability of capillaries increases, which is why they become more noticeable and begin to “see through” the skin.
With vegetative-vascular dystonia (the so-called polyetiological syndrome, which is not a disease), bruises under the eyes also often form. At the same time, other signs appear: migraine, dizziness, asthenia, cardialgia, changes in heart rate and breathing, swelling of tissues, tremors of the hands, coldness of the extremities, feeling of heat in the face, sleep disturbance, fainting, neurotic disorders.
The maximum number of mast cells accumulates in the periorbital region, which causes the reactivity of the skin surrounding the eyes and frequent allergies. In diseases of an allergic nature (allergic rhinitis, hay fever), blood vessels dilate and their permeability increases, as a result of which the skin under the eyes darkens.
Hereditary predisposition
This group includes people who lead a healthy lifestyle and do not have health problems. For them, dark circles under the eyes are the norm. This problem is more common in women with very dry and dark skin.
It should be noted that the risk of hyperpigmentation of the skin in the periorbital zone increases with the use of tetracyclines, sulfonamides and oral contraceptives.
All of the above factors are enhanced by excessive exposure to ultraviolet radiation. In this case, the defect becomes stable and difficult to treat.
Dermal melanocytosis
Melanocytes are skin cells that produce melanin. In healthy skin, only melanocytes of the epidermis and hair follicles are able to synthesize melanin. However, with dermal melanocytosis, immature melanocytes (lingering in the dermis during embryogenesis) already begin to actively synthesize melanin, which leads to the formation of spots. If the dark eyelids have a similar origin, this can be easily determined by the gray or bluish-gray tint around the eyes[3].
Dermal melanocytosis can be either acquired or hereditary. The reasons for its occurrence may be:
- influence of the sun
- hormonal changes during pregnancy
- chronic eczema
Treatment methods
If the diagnosis does not reveal internal diseases, then circles under the eyes are a cosmetic defect that appears as a result of an incorrect lifestyle or hereditary predisposition.
In such cases, the most popular and effective treatment methods are:
- Mesotherapy. Typically, meso-cocktails are used, which contain arbutin, ascorbic, kojic and phytic acids. The therapeutic course includes 6-10 procedures, between which there is a one-week break.
- Bioreparation with ascorbic acid (vitamin C). Thanks to the combination of ascorbic and hyaluronic acid, the skin around the eyes is well moisturized and noticeably brightened. The course of treatment consists of 2-4 sessions, with a 2-week break between them.
- Plasmolifting. The procedure restores metabolism, normalizes tissue respiration, activates blood microcirculation, thereby increasing local immunity. A similar effect will appear after 4-6 sessions at weekly intervals.
- Biorevitalization. The skin around the eyes shows a pronounced reaction to dehydration and, due to dryness, often takes on an unaesthetic appearance, creating the effect of “tired eyes”. A course of birevitalization, consisting of 2-4 procedures with a 2-week interval, will help solve the problem.
- Contour plastic. If the blood vessels are located close to the skin and “see through” through it, then the filler forms an additional layer, making the vessels almost invisible. In addition, the drugs smooth out the nasolacrimal groove.
- Laser peeling. Using a laser, the top layer of skin is removed, which stimulates the regeneration process and promotes rejuvenation. The treatment course involves 2-5 procedures with a one-month break.
Diagnosis of eye melanoma
The diagnosis of ocular melanoma is made on the basis of complaints, information about the development of the disease, examination data and the results of additional studies. At the initial stage, ophthalmologists perform direct and reverse ophthalmoscopy. When identifying space-occupying formations, diaphanoscopy and biomicroscopy of the eye are performed.
In order to exclude the presence of ocular melanoma metastases to internal organs, patients at the Yusupov Hospital undergo the following examination:
- X-ray of the chest, skeletal bones;
- Ultrasound examination of the abdominal organs, kidneys;
- Magnetic resonance imaging of the liver, brain;
- Computed tomography of the kidneys and brain.
A biopsy for suspected melanoma of the eye is not performed due to the risk of dissemination of atypical cells. Histological examination is carried out after surgical removal of the tumor.
Localization and forms of eye melanoma
Most often, ocular melanoma is located in the choroid area. This type of tumor is the most favorable. Actually, the choroid is affected in approximately 85% of cases, the ciliary body in 9%, and the iris in 6%. Malignant changes in the conjunctiva and eyelids are much less common, but are much more severe.
Depending on the morphological features of the structure of tumor cells, the following forms of melanomas are distinguished:
- Epithelioid;
- spindle cell;
- Fascicular;
- Mixed.
The most malignant is the epithelioid form, as it is characterized by faster growth and metastasis. The most favorable prognosis for spindle cell melanoma of the eye. The nodular form of a malignant neoplasm of the choroid is a node; in the diffuse form, the tumor grows “along a plane.”
Depending on the spread of the tumor process, there are 4 stages of ocular melanoma:
- T0 – tumor is not detected;
- T1 – the neoplasm is located within one quadrant of the conjunctiva of the eye;
- T2 – more than 1 quadrant of the conjunctiva of the eyeball is affected;
- T3 – tumor extends to the conjunctiva of the eyelid or to the fornix;
- T4 – the pathological process involves the eyelid, orbit or cornea.
In case of lesions of the choroid proper at stage T0, the neoplasm is not detected, T1a – the tumor has dimensions not exceeding 7×3 mm, T1b – neoplasm measuring 10×3 mm, T2 – melanoma dimensions up to 15×5 mm, T3 – tumor size up to 15 ×5 mm; T4 – the pathological process has spread beyond the eye.
At stage T0 of ciliary body melanoma, no space-occupying lesion is detected, at T1 the tumor does not extend beyond the ciliary body, T2 – eye melanoma affects the anterior chamber or iris, T3 – invasion into the choroid proper is determined, T4 – the tumor process spreads beyond the eye.
In the presence of T0 stage of iris melanoma, the neoplasm is not detected. Stage T1 is characterized by the presence of a tumor within the iris, T2 - damage to the anterior chamber angle and one quadrant, T3 - damage to several quadrants, the anterior chamber angle, the choroid itself or the ciliary body. At stage T4, metastases to internal organs are determined.
Symptoms of eye melanoma
The first sign of melanoma may be the appearance of a pigmented formation in the eye area. Some patients report vision errors - floaters, flashes or spots. There is a gradual deterioration in visual acuity and loss of peripheral vision. Subsequently, the space-occupying formation increases in size, grows into nearby organs and tissues, affects regional cervical, submandibular, periauricular lymph nodes, and metastasizes to the liver, kidneys, bones, bones. With the development of metastases, the function of the affected organs is disrupted.
Melanoma of the eyelid is a voluminous pigmented formation, which sometimes has a clearly defined stalk. The surface of eye melanoma may be covered with fissures or papillary growths. The neoplasm is characterized by rapid progression and early formation of distant metastases.
Conjunctival melanoma can occur at any age. It is located at the lacrimal caruncle, in the area of the limbus or semilunar fold. May be single or multiple. Resembles a pigmented nodule. It is characterized by exophytic growth and, when spreading, affects the cornea, sclera and orbit. It progresses quickly and metastasizes early.
Melanoma of the choroid itself occurs in stages:
- At the first stage, there are no clinical signs; examination reveals a grayish lesion with blurred boundaries with a diameter of no more than 10 mm;
- At the second stage, the tumor increases in size, and new vessels appear in its tissues. Hemorrhages may occur in the neoplasm, retina and vitreous body. Upon examination, ophthalmologists detect redness of the conjunctiva, iridocyclitis, swelling of the eyelid and other signs of local inflammation. Patients complain of pain in the eye area;
- At the third stage, the tumor grows outside the organ. Protrusion of the eyeball (exophthalmos) and orbital deformation are noted. Intraocular pressure decreases. The tumor grows into the brain and cerebral sinuses. When spreading into brain tissue, various neurological disorders can occur;
- The fourth stage is characterized by generalization of the tumor process. Patients with ocular melanoma exhibit common symptoms of cancer pathology: fatigue, weakness, loss of appetite and weight. Metastases are found in the liver, lungs, pleura, bones, and other organs.
Ciliary body melanoma is detected mainly in patients 40-60 years old. It is characterized by circular growth with simultaneous damage to the anterior chamber angle, iris root and ciliary body. In the early stages of the disease, intraocular pressure increases. Ocular melanoma quickly spreads beyond the sclera and early gives distant metastases.
Iris melanoma is a nodule that is located on the surface or in the thickness of the iris. Most often localized in the lower part of the iris. The rate of spread of the tumor process varies greatly. Rarely metastasizes. The course is more favorable than melanoma of the choroid and ciliary body.
How to recognize blepharitis?
There are common symptoms of blepharitis. These include:
- photophobia;
- rapid eye fatigue when reading;
- feeling of heavy eyelids;
- swelling, redness (especially in the morning after waking up);
- thickening and swelling of the ciliary edge of the eyelids;
- feeling of “sand in the eyes”;
- itching;
- eyelash loss;
- the appearance of discharge and gluing of the eyelids;
- the appearance of dry crusts on the ciliary edge of the eyelids.
If one or more of these signs appears, you should contact an ophthalmologist to make an accurate diagnosis and prescribe the most effective treatment.
Preventive actions
To prevent the formation of dark circles under the eyes, it is recommended:
- adhere to a regime of wakefulness and rest;
- eat a balanced diet;
- maintain water regime;
- take vitamin and mineral supplements;
- to refuse from bad habits;
- do eye exercises;
- avoid direct sunlight to reduce insolation;
- use high-quality perfumes and cosmetics;
- walk in the fresh air more often;
- avoid stressful situations.