Vulgar acne or acne is one of the most common skin diseases. Acne vulgaris most often occurs in adolescence and young adulthood, however, the disease is not limited to this age period. Vulgar acne can also be registered in mature people if there is a genetic predisposition to the disease, hormonal disorders, use of inappropriate cosmetics and other reasons for changes in the balance of sebum production.
Vulgar acne in ICD 10
Acne vulgaris is a generally recognized disease and, according to the international classification ICD 10, has code L70.0 - Acne vulgaris.
The pathogenesis of acne vulgaris includes four main mechanisms:
- Increased sebum production
- Impaired keratinization and desquamation of the epithelium
- Invasion and reproduction of a bacterial pathogen (most often propionobacterium acne)
- Development of the inflammatory process around the hair follicle
For those who have to deal with acne vulgaris, often the most severe is not the physiological, but the psychological, psychosocial impact of the disease, associated with quite severe worries about their appearance. It is well known that most often vulgar acne manifests itself in adolescence - precisely the period when active, often dramatic changes take place in the mental and social sphere of the individual.
The following types of acne vulgaris are distinguished:
- Papular acne
- Pustular acne
- Abscess acne
- Phlegmonous acne
- Indurative acne
- Drain blackheads
- Acne conglobata
- Acne inversus
Papular acne is an inflammatory nodule of pink or bluish-red color and elastic consistency. They have a conical or hemispherical shape, up to 2-4 mm in diameter and cause almost no subjective sensations. The full development cycle of papular acne lasts up to 10-12 days. In the absence of trauma, gradually disappearing pigment spots usually remain at the sites of resolved papular acne.
Pustular acne can appear primarily in the form of a nodule with a pustule in the center or transform from papular acne. In appearance, pustular acne is similar to ostiofolliculitis and folliculitis, but does not have such a bright inflammatory color and proceeds more sluggishly, for a long time. Scars do not form after resolution of pustular acne.
Acne abscesses: the full development cycle of pustular acne takes 2 weeks. They may resolve without leaving scars or abscess. After healing of abscessed acne, which occurs 2-3 weeks after their occurrence, superficial atrophic scars remain. Acne abscesses occur predominantly on the back of the neck, in the upper chest and back in weakened and anemic patients who have been suffering from dermatosis for a long time.
Phlegmonous acne: inflammatory formations of a flattened shape, large in size up to 1 cm in diameter, soft to the touch, surrounded by a zone of hyperemia and edema.
Indurative acne: large, dense and painful nodules of bluish-pink color, the full development cycle of which lasts 3-4 weeks. A feature of the course of indurative acne observed in some patients is its undulation with periodic subsidence and intensification of inflammatory phenomena.
Confluent acne: formed as a result of the confluence of abscess, phlegmonous and indurative acne.
Acne conglobata: it should be noted that some authors consider acne conglobata to be an independent disease, different from acne vulgaris, since it occurs at a later age and is chronic. At the same time, they emphasize that the pathogenesis of dermatosis is not clear, however, due to the frequent detection of coagulase-positive staphylococcus and beta-hemolytic streptococcus, the authors believe that acne conglobates represent true pyoderma.
Inverse acne: hidradenitis is an acute purulent inflammation of the apocrine sweat glands, usually localized in the axillary, inguinal and perianal areas, as well as under the mammary glands. Pathogen: coagulase-positive staphylococcus. Hidradenitis differs from a boil in its hemispherical shape and the absence of a necrotic core.
Psychological aspects of acne vulgaris
Vulgar acne can have such a noticeable impact on a person’s psychological state, since the main zone of localization of the inflammatory process - the face - is the central object in interpersonal communication, and it is on it that the attention of interlocutors and those around them is focused. That is why acne vulgaris can not only reduce self-esteem, but also contribute to the emergence and progression of various psychosomatic disorders, primarily depression. Vulgar acne, even in its mildest form, can cause quite severe stress.
This is most pronounced in young patients. Their value orientations have not yet been formed, they are very vulnerable, and self-esteem is one of the most painful areas. Appearance for boys and girls is not just a calling card, but one of the fundamental reasons for success in society, in life, in a career. In addition, ideal appearance and figure are a clear demonstration of good health. At the same time, momentary criteria of beauty are created and popularized by young people themselves, and usually defects like vulgar acne are perceived extremely negatively in the light of these frameworks. Many girls suffering from vulgar acne begin to actively use decorative cosmetics, which, with such extensive use, only aggravates the situation, contributing to the progression of acne.
Vulgar acne, masked in this way constantly (and not once, for example, for a photo), will progress; Ultimately, getting rid of acne will require more serious and complex treatment. Many teenagers with vulgar acne try to avoid playing sports, since this is where revealing clothing is often used. Problems with self-esteem progress, a feeling of rejection is formed, and traits such as unsociability, shyness, and isolation begin to predominate in behavior. In adults, the situation is not much better - the disease can have a very strong impact on the state of mind.
People with acne vulgaris are often haunted by a feeling of inferiority, inferiority, and problems establishing social contacts, especially when it comes to people of the opposite sex. Such psychological problems affect all areas of a person’s life - study, work, career, relationships, family life, etc. Studies have revealed a direct connection between the presence of vulgar acne and problems finding work - among those who suffer from acne, hardly any are unemployed not twice as much. In general, even mild acne can be identified as a cause of serious social discomfort.
The influence of emotional factors in acne vulgaris is almost as significant as in other socially significant diseases - epilepsy, bronchial asthma, rheumatoid arthritis, diabetes mellitus. At the same time, the degree of emotional discomfort often does not have a direct relationship with the severity of the disease - often the highest level of anxiety is observed just with a mild degree of acne vulgaris. Research by scientists shows that a pronounced manifestation of fear and depression is more often observed in young people with moderate forms of acne vulgaris than in those who are faced with severe acne. Such situations are usually interpreted as the result of the work of “psychological adaptation” - a mechanism of gradual adaptation, getting used to the disease in adolescence, perceiving it as a negative, but inevitable and habitual phenomenon. From a physiological point of view, adaptation is expressed in a decrease in sensitivity to itching and pain; In the psychological aspect, we can talk about the formation of a “partnership” relationship with the disease.
The optimal approach for a person suffering from acne vulgaris is to follow all medical recommendations, implement all preventive and therapeutic measures, and at the same time maintain an emphasis on an overcoming style of behavior - a life credo “in spite of the disease”, aimed at achieving and maintaining a high level of social interaction. R. Berger offers a conditional classification by personality type of patients with acne vulgaris in accordance with his own observations:
- The “indifferent” group is approximately 20% of the total number of those experiencing vulgar acne; These people believe that acne is a temporary phenomenon that you just need to wait it out without making any special efforts to treatment and prevention.
- The “active” group is about a third of the total number of patients; These people were able to avoid severe emotional damage and treat acne vulgaris as a more or less standard manifestation of the transition period, to combat which the simplest methods of self-medication are sufficient.
- The “depressed” group is almost half of all people with acne vulgaris; a high level of psychological sensitivity means a significant emotional burden, a strong blow to self-esteem, the formation of a stable social inferiority complex, a sharp decrease in the volume of interpersonal communication; In addition, this group of patients demonstrates low confidence in the effectiveness of treatment.
The psycho-emotional aspects of acne vulgaris are seriously influenced by several factors:
- the patient’s primary attitude to his own illness, as well as to the possible outcome of the situation;
- the degree of accompanying cosmetic defect in appearance;
- the presence and severity of scars on the face that form as a result of acne vulgaris and remain even after complete recovery;
- disorders of the psycho-emotional sphere that precede the appearance of acne vulgaris; the level of the patient’s general psychological state.
Very often, dermatologists have to deal with patients who are sure that their case of acne vulgaris is the result of a rare and difficult to diagnose problem of the sebaceous glands, and that is why they need a lot of examinations, procedures, and non-standard treatment methods. In this case, one should suspect a disguised, “erased” form of depression, in which the classic signs of the disorder are weakly expressed or completely absent. No less often, doctors are faced with another type of mental disorder in acne - social phobia, the fear of being in society.
Due to defects in appearance, a person with acne vulgaris is constantly in an anxious state, which can be mistaken for a feature of self-awareness, showing the level of isolation of the person. Visible skin defects caused by acne vulgaris can attract the attention of others, which is a strong negative factor for patients and forces them to seek social isolation. Subjective sensations, awareness of oneself as ugly, disfigured have a very strong impact on self-esteem. The real experience of someone else's negative reaction to manifestations of acne vulgaris (distancing, disgust, ridicule) is a powerful stimulus for “withdrawal.”
A complex of psychological difficulties (low self-esteem, obsessive negative thoughts, critical self-perception) often leads to the formation of a special form of acne, directly related to the manifestation of neurosis - squeezing out rashes. Excoriated acne is most often observed in teenage girls, often leading to the formation of multiple hypo- and hypertrophic scars; constant squeezing only provokes increased inflammation; The question is no longer about how to treat vulgar acne, but how to deal with a more severe form of acne.
Of course, today society's requirements for appearance are much more serious than a couple of decades ago. However, we often have to deal with an excessive, painful fixation of a patient with vulgar acne on the defects of his appearance with a frank thickening of dark colors when assessing the situation.
Etiology and pathogenesis of acne
The main sex hormones that regulate the activity of the sebaceous glands are androgens . They affect the development and increase in the size of the sebaceous glands in androgen-dependent areas of the skin, the hyperproduction of sebum and the proliferation of keratinocytes in the ducts of the sebaceous glands, the hair canal and the mouths of the pilosebaceous follicles.
According to the inflammatory concept of acne, the chain of pathogenetic events begins with androgen-induced inflammation of the sebaceous gland . This causes proliferation and active desquamation of keratinocytes in the upper part of the pilosebaceous follicles. Progressive hyperkeratosis and the associated difficulty in the outflow of sebum lead to the formation of comedones , which subsequently transform into papules and pustules or spontaneously regress.
Overproduction of sebum contributes to changes in its qualitative composition. In sebum, the concentration of linoleic acid decreases, which suppresses the expression of transglutaminase and is involved in the synthesis of the main components of the intercellular matrix. This leads to an increase in the pH of sebum and a change in the permeability of the walls of the follicles and the stratum corneum of the epidermis.
Sebum stagnation creates anaerobic conditions that are optimal for the proliferation of propionibacterium acnes in the pilosebaceous follicles. They secrete substances that damage the walls of ducts and glands, as well as factors that attract neutrophils.
The release of lysosomal enzymes by neutrophils further reduces the strength of the follicle wall, which ultimately leads to their rupture. The contents enter the dermis, where local inflammation develops according to the “foreign body reaction” type.
Exogenous factors contributing to the development of acne:
- taking sex hormones, anabolic steroids ( Fig. 1 );
- high glycemic index diet;
- smoking;
- whole milk;
- fast food;
- chocolate;
- various occupational hazards;
- hot and humid climate.
Rice. 1. Acne on the shoulder and back of an athlete due to the use of anabolic steroids (Danish national service on dermato-venereology)
https://www.danderm-pdv.is.kkh.dk/atlas/4-120-9.html
Treatment of acne vulgaris
Modern medicine offers people suffering from acne a huge range of treatments for acne vulgaris. These medications have different active ingredients and are available in various forms: ointments, gels, creams, tablets, etc. The use of a wide range of products allows you to influence several parts of the pathogenesis of acne vulgaris at once, which provides a faster and more pronounced effect.
For moderate to severe acne vulgaris, the basis of therapy is the prescription of systemic antibiotics. Drugs from the group of tetracycline antibiotics demonstrate high effectiveness in the treatment of acne vulgaris, which can help even with advanced, severe forms of acne, when other drugs are powerless. Tetracycline antibiotics act on one of the main links in the pathogenesis of acne vulgaris - they eliminate the bacterial causative agent of the disease. They are also distinguished by an extremely high degree of fat solubility, which facilitates its penetration into the secretions of the sebaceous glands and inside the bacterial cell. Tetracycline antibiotics have a powerful therapeutic effect, allowing you to eliminate papules, pustules and cysts, even in a very advanced state. After just 6 weeks of taking tetracycline antibiotics, the number of acne lesions is halved*. Treatment of acne vulgaris with antibiotics can be carried out at any time of the year, since the drug, unlike doxycycline, has a low level of photosensitivity and, accordingly, does not cause photosensitivity in patients with acne vulgaris.
In most cases, eliminating severe visual acne defects through treatment and therapy allows you to get rid of the stress factor and significantly improve the patient’s psychological state. The psychological state of the patient is one of the most important criteria for assessing the overall severity of acne vulgaris. Psychological discomfort, emotional distress and suffering can themselves serve as an indication for the use of drug treatments. It must be remembered that negative emotions are most often a response of the psyche to a cosmetic skin defect, that is, to a stress factor. At the same time, effective elimination of the disease is the most effective way to combat such stress, superior to any psychotherapeutic techniques. Successful treatment of acne vulgaris almost always means an improvement in the quality of all aspects of life (study, work, relationships, career, etc.).
*Antibiotics in the treatment of acne: the problem of rational choice Belousova T.A., Goryachkina M.V. PMGMU named after. THEM. Sechenov.
Principles of acne treatment
A carefully collected anamnesis will allow the specialist to understand what tactics should be used in the treatment of acne in a particular patient.
Among the general recommendations, it is worth mentioning the possibilities of diet . You should eat more vegetables, avoid fast food, whole milk and casein-containing products, chocolate, saturated fats, trans fats, easily digestible carbohydrates, foods with a high glycemic index, and also eat regularly and properly, and monitor your weight.
The basic strategy for combating acne on the face and body involves the following steps:
- Cleansing - you can use emulsions, solutions and foams that have a neutral pH (5.5–7.0). It is important that they do not contain anionic surfactants (surfactants) that increase alkalization of the stratum corneum of the epidermis. The fact is that this leads to its swelling, maceration and increased blockage of the mouths of the pilosebaceous follicles.
- Exfoliation - its purpose is to smooth the surface of the skin, free the mouths of the sebaceous hair follicles from accumulated secretions, exfoliate corneocytes and restore the normal outflow of sebum. This procedure should not be overused, since aggressive exfoliation leads to damage to the epidermal barrier, which is clinically expressed by redness, irritation, peeling and increased sensitivity of the skin.
- Skin nutrition - active ingredients may include: vitamin D, vitamin B2, vitamin C, genistein, daidzein, kigelia, tea tree oil, papaya, various prebiotics, formononetin, equol, apricot extract, basil extract, cornflower extract, chondrius algae extract Crispus, ginkgo biloba extract, etc.
- Sun protection is very important, since ultraviolet and infrared rays activate sebum production and reduce local immunity in the skin, which often leads to exacerbation of acne after sun exposure.
Avocutin (butyl avocadate) was biotechnologically isolated from avocado oil , a fatty acid ester that can suppress the synthesis of 5-alphareductase, an excess of which is present in the skin of people with acne. It has been established that as a result of using a product containing 3% avocutin, the oiliness of the skin of the face and scalp is reduced by a third in the first two weeks of use.
A fairly universal cosmetic ingredient that will also be useful for acne is bitter aloe extract (Aloe Ferox Extract). It destroys and blocks the activity of many pathological microorganisms - streptococci, staphylococci and propionibacteria.
To treat acne on the face and body, you can use chemical peels, creams and gels with tretinoin, 20% azelaic acid cream, 10% sulfacetamide lotion, 2.5–10% benzoyl peroxide gels, various antibiotics (erythromycin, clindamycin), and also injection procedures: PRP therapy (injection of platelet-rich plasma into the skin) or mesotherapy (for example, hyaluronic acid modified with vitamin C, cysteine and glutathione).
Western acne treatment consensus recommends a combination of topical retinoids with topical and systemic antimicrobial therapy. It has been proven that its effectiveness significantly exceeds monotherapy with these drugs, which is due to complementary mechanisms of action aimed at various pathogenetic factors of the disease:
- retinoids (tretinoin) reduce excessive desquamation of the epithelium, exhibit comedolytic and some anti-inflammatory effects;
- local antibiotics (benzoyl peroxide) reduce the number of propionibacteria in acne lesions and have some keratolytic effect;
- systemic antibiotics (doxycycline, minocycline) suppress inflammation and inhibit the proliferation of Propionibacterium acnes.
It is impossible not to mention systemic retinoids - isotretinoin preparations. They are typically used to treat severe and treatment-resistant forms of acne. For some patients, one course of oral isotretinoin is enough to achieve remission of the disease, while others require additional courses. One study found that 38% of patients treated with systemic retinoids had no signs of acne during a 3-year follow-up period, 17% had their disease controlled with topical therapy, 25% required topical and systemic antibiotics, and 20% received a repeat course. isotretinoin. Relapse was more common in young patients and girls. However, it should be remembered that for all its effectiveness, isotretinoin has serious side effects associated with the development of depression and possible suicide of patients.
Hardware treatment of acne can be used in cases where therapy with systemic retinoids is ineffective or contraindicated. There are at least 2 methods of effectively influencing the inflammatory elements of acne:
- Deep heating of the skin, which leads to normalization of sebum formation and improved cleansing of the mouths of hair follicles. Such heating can be carried out by an IPL system ( M22 ) or an RF device ( Thermage ).
- Exposure of the anaerobic bacteria Propionibacterium acnes to broadband pulsed light in the blue part of the spectrum in order to induce the formation of free radicals from the uroporphyrin metabolite in these bacteria and their subsequent death. This method is implemented in IPL systems equipped with a special filter ( M 22 IPL , Acne filter with passbands 400–600 nm and 800–1200 nm).
White and blackheads on the face -
There are two types of acne. The first option is the so-called whiteheads (they are also called closed comedones). They can range in size from 0.1 to 3.0 mm and appear as small white bumps on the surface of the skin. With whiteheads, the lumen of the hair follicles will be swollen and filled with dense fatty contents (sebaceous plug), and the outlet of the follicle on the surface of the skin will be almost invisible. Such acne can persist for a period of several weeks to several months, and can turn into either blackheads or inflamed pimples in a few days.
1) What do whiteheads (closed comedones) look like?
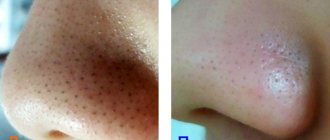
The second option is blackheads (also called open comedones), which appear as dark-colored dots in the pores of the skin. They can range in size from 0.1 to 3.0 mm, and in this case we directly see the upper part of the sebaceous plugs in the skin pores. What gives them their dark color is not dirt, as is commonly believed, but the skin pigment melanin. Most often, open comedones are the result of transformation of closed comedones (Fig. 4-6).
2) Blackheads (open comedones) –
Almost all people have acne on their nose. Acne is quite common on the forehead, chin, cheeks, as well as on the back and shoulders. This localization is explained primarily by the fact that it is in these areas in the skin that the largest number of sebaceous glands is observed, the number of which reaches from 400 to 800 per 1 cm2. According to statistics, whiteheads are 4 times more common (compared to blackheads).
Important: you should distinguish between common acne vulgaris and acne (despite the fact that both are classified as acne). We have already said above that acne is also called “comedonal acne,” and this form is always distinguished by the absence of inflammation in the area of the hair follicles. Pimples are usually called inflammatory formations that arise in the area of hair follicles, which can be in the form of papules and/or pustules (Fig. 7).
Pustule (traditional pimple with pus inside) –