Doctors Cost
Price list Doctors clinic
Radio wave removal of condylomas is an advanced method of removing these formations from the skin and mucous membranes. The procedure involves applying a radiosurgical instrument to the affected surface and has proven to be effective and relatively safe. The specialists of the Family Doctor clinic were among the first in the region to successfully use radio wave surgery, so our extensive practice allows us to achieve high efficiency of such manipulations.
Causes of condylomas and indications for removal
The reason for the formation of genital warts lies in infection with human papillomavirus. Formations that are located in areas of the skin subject to constant trauma must be removed first - constant mechanical stress can lead to infection (inflammation) and even malignancy. However, removal of condylomas with Solcoderm or radio waves is also preferred if they have formed on a “safe” area of the skin, which is dictated by aesthetic considerations.
Prevention of genital anal warts
Primary prevention of diseases associated with human papillomavirus infection is to reduce the likelihood or prevent infection. This is achieved through the implementation of a set of preventive and anti-epidemic measures. Doctors recommend not to have early sexual relations, try to have one sexual partner, and resort to barrier methods of contraception, which reduce the risk of developing anal warts, but do not provide reliable protection against infection with the human papillomavirus.
In order to prevent infection, doctors vaccinate persons of both sexes aged 9 to 17 years (women up to 26 years old) who are not infected with human papillomavirus types 6, 11, 16, 18. To achieve the greatest effect, the full course of vaccination is carried out before first sexual contact. Vaccinations are also given to persons infected with human papillomavirus of one, two or three genotypes included in the vaccine. Vaccination is carried out to prevent infection with other types of human papillomavirus and the development of diseases associated with them (anal warts). In order to undergo an effective course of treatment for anal warts or preventive vaccination, make an appointment with a proctologist at the Yusupov Hospital online or by calling the contact center specialists in advance.
Radio wave removal procedure
Radio wave removal of condylomas begins with preparatory measures. These include the following:
- Consultation and examination by a gynecologist;
- Determination of HPV type and concomitant infectious diseases;
- Blood test for HIV, syphilis, hepatitis;
- If necessary, colposcopy (examination of the affected area with a colposcope) and biopsy (histological examination of removed tissues is carried out after the procedure in order to clarify the diagnosis and exclude a malignant disease).
The removal operation itself is performed under local anesthesia: injections of anesthetics, a gel or a spray with an anesthetic effect can be used for these purposes. After performing anesthesia, the doctor proceeds directly to the removal - this is carried out with a radio knife, without contact with the patient’s skin. The method is based on the fact that high-frequency radio waves generate a large amount of thermal energy. The cellular fluid heats up, the structure is destroyed - the cells that are exposed immediately evaporate. Heat allows not only to “evaporate” the cells, but also to “seal” small vessels, which reduces the risk of bleeding and infection to zero and ensures rapid healing.
Skin lesions must be completely removed to prevent their reappearance. The area where the manipulation took place is treated with an antiseptic solution, and if necessary, an ointment application is carried out.
How is genital warts removed?
- surgically (excision);
- hardware ablation (diathermocoagulation, cryogenic destruction, laser coagulation, radio wave excision);
- contact chemical method.
Classical surgical excision of condyloma acuminata is applicable for single, fairly hard formations (10 mm in diameter or more) formed on the penis, in the vagina or around the anus, for large formations, as well as for relapses of condylomatosis after other treatment methods. Excision is performed under local anesthesia, sutures are placed on the wound at the site of the excised condyloma, and a scar is subsequently formed. Pain after surgery can last up to three weeks. Removal of genital warts with electric current - diathermocoagulation: this is burning out the formation with high temperature created by high-frequency current. The method is painful, so local anesthesia is needed. At the site of the burned genital wart, a scab forms, which falls off on its own after 7-8 days. After the scab falls off, a large scar remains. Currently, electrocoagulation is considered an outdated method; According to foreign experts, the probability of relapse after its use ranges from 30 to 70%.
Nitrogen removal
Cryotherapy or removal of genital warts with nitrogen is the destruction of genital warts by instantly (within 10-20 seconds) freezing tissue with liquid nitrogen (temperature below -195°C). Necrosis and rejection of the condyloma occurs. This method is most often used to remove several small condylomas, especially those located on the penis, vagina, rectum and urethra. Although there is an opinion that this method should not be used in hard-to-reach places. Local anesthesia is used if warts are present in several places or when the affected area is large. During the procedure, patients feel a burning sensation, and after its completion - moderate pain. Blisters and skin hyperemia may appear, but virtually no scars remain. Healing occurs on average within two weeks. The probability of relapse of the pathology (after several months) is 20-40%.
Laser removal
Laser therapy (using carbon dioxide or infrared lasers) completely removes viral tumors with an efficiency of up to 90%. But this method is very painful and is performed under local anesthesia or general anesthesia, depending on the number and size of the warts. As a rule, the wounds heal for at least a month, leaving scars at the site of removal. Laser removal of genital warts is recommended for the treatment of large genital warts that cannot be treated using other physical ablation methods due to access difficulties. This applies to condylomas located deep inside the anus or urethra. With this method, the risk of recurrence of condylomas is 25-50%.
Removal by radio wave method
With this method, condylomas are removed using a special radio wave surgical generator Surgitron Dual, which operates without contact with tissue - radio waves. According to doctors and patients, this procedure is quick, minimally injures the surface of the skin and mucous membranes and does not cause pain. Radio wave excision - removal of genital warts using the radio wave method - is a bloodless, high-precision method of hardware surgery, since the dissected tissue is simultaneously coagulated, preventing bleeding. After it is carried out, there is no need for stitches and no scars are formed. In general, experts consider physical ablation to be more effective for keratinized condylomas, and for soft condylomas in the genital area, a contact chemical method of removal is more suitable.
Removal with Solcoderm
A chemical method to solve the problem is to remove genital warts with Solcoderm. This solution (in ampoules of 0.2 ml) is intended for external use only. It contains nitric, acetic and lactic acid, oxalic acid dihydrate and copper nitrate trihydrate. The action of a concentrated acid compound leads to chemical denaturation of the proteins of condyloma tissue, its drying out and falling off in the form of a scab. If the drug gets on healthy skin or mucous membranes, burns and necrosis also occur. Therefore, according to the instructions, Solcoderm should be applied only in a medical institution, and the patient himself is not recommended to do this, although the ampoules are supplied with an applicator and a glass tube for manipulation.
It should be borne in mind that removing genital warts at home is very problematic in the absence of an overview of the genital formation, and is also very unsafe if there are several of them and they are located on the mucous membranes. And doctors warn that attempts to get rid of condylomas on your own can lead to their quantitative growth. If condylomatosis is multiple, then Solcoderm is not applied to all formations at once, but in stages: on 4-5 condylomas in one procedure, after 24-25 days - on the next . In addition, after contact with water, it is necessary to treat the skin in the area where the drug is applied with 70% medical alcohol. And in no case should you tear off the resulting scab: it must fall off on its own. Preparations for the chemical removal of genital warts also include solutions of Feresol (phenol with tricresol) and Verrucacid (phenol with metacresol), which should be applied only to externally located condylomas - several times , after the already applied solution has dried.
Advantages of the method
Removing condylomas using the radio wave method has many advantages:
- Low-traumatic - ease of tissue dissection without the usual scalpel, no impact on the upper layers of the skin, no mechanical damage to capillaries and tissues;
- The ability to control the depth of exposure of the radioknife, as well as the area of impact on tissue - allows you not to affect surrounding healthy tissue;
- No rough scars after the procedure, which is especially important for patients planning pregnancy;
- Timely coagulation of blood vessels, which reduces the risk of bleeding and swelling;
- Speed (no more than 30 minutes) and high efficiency of the procedure, quick rehabilitation period;
- Antiseptic effect of radio waves - reduced risk of infection, inflammation;
- Painless due to the lack of impact on sensitive receptors;
- Complete removal of affected tissue; minimal possibility of their reoccurrence
- Possibility of removing condyloma of any location;
- Preservation of high quality material for further laboratory research.
However, despite the advantages, radio waves may be contraindicated in some cases.
Condylomas acuminata - symptoms and treatment
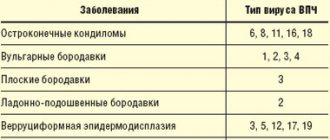
The key point in the pathogenesis of the disease is the penetration of HPV into the host body. With a single sexual contact, the probability of infection is 80%, then, with a good state of the immune system, infectious agents are eliminated (destroyed).
Viruses of various types are adapted to a specific host. There are hundreds of types of viruses, many of them are not dangerous to humans, since they are tropic to the tissues of mammals, reptiles and birds and cause benign tumors in them (formation of papillomas).[3]
When studying HPV, three types of viruses were identified - alpha, beta, gamma. Of these, anogenital lesions are caused by papillomaviruses of the first group (α). Infectious agents belonging to the Beta and Gamma genera are more often found with papillomas of the keratinizing epithelium [3] - plantar and palmar warts appear.
In genera, when classifying viruses, types (genotypes) were identified. They are indicated by Arabic numerals. Of the hundreds of virion genotypes, particles with a high carcinogenic risk are isolated - these are α 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59. They are detected in 90-95% of cases with malignant processes of the cervix , vagina and vulva. Types 16 and 18 are especially significant. Such oncogenic types of HPV, containing E6 and E7 proteins in their DNA, are able to suppress the activity of the tumor suppressor proteins p53 and pRb, leading to the rapid malignant transformation of papillomas into carcinomas.
About 90% of cases of anogenital warts are caused by HPV α 6 and 11. These are pathogens of low carcinogenic risk.[5] This same low-risk group includes HPV 40, 42, 43, 44, 54, 61, 72, 81.
Penetration
Virions penetrate the basal layer of the epithelium through microscopic damage and then attach to cell membrane proteins. Next, they engage the mechanism of receptor endocytosis (with the participation of integrin and L1 protein from the viral capsid) and enter the cytoplasm. The L2 protein from the viral capsid promotes the release of viral DNA and its entry into the nucleus.[5]
Reproduction
Proteins E1 and E2 from the DNA of the virus are involved in the replication of the foreign genome in the nucleus of the affected cell. At the same time, the cell retains the ability to divide and reproduce its own DNA. By multiplying its DNA, the virus ensures its presence in the form of episomes in the cytoplasm (about 100 per cell). This joint “work” of the virus and the host cell leads to a failure in the processes of proliferation (cell reproduction) and differentiation in the basal layer, leading to visual manifestations.
Manifestations
Abnormal endophytic or exophytic growths of the epithelium appear - papillomas, spots or condylomas. Loose mucous membrane or atypical epithelium of outgrowths are prone to rapid traumatization and maceration (softening). Against this background, a secondary infection quickly develops, pain, discomfort, copious discharge, inflammation, swelling, unpleasant odor, and ulceration of condylomas appear.[2][3]
In the cells of the basal layer, active replication of the virus occurs; as condyloma cells differentiate, their blood supply is sharply depleted, and the central vessels are reduced. But, remaining in the upper layers of the epithelium in an inactive form, this is where the virus is dangerous in terms of contact infection.
During histoanalysis of biopsy materials, the epithelium is thickened, areas of acanthosis and papillomatosis are revealed. Koilocytes are detected (changed in size cells with light cytoplasm, many vacuoles, and a perinuclear light rim). Their nuclei are hyperchromatic. Cells with two or more nuclei are often found.[8]
From the above we can conclude: viruses that cause the formation of anogenital warts, in 90% of cases, belong to types α 6 and 11 HPV.[6][7] They have a low probability of causing malignancy (cancerous degeneration). However, there are frequent cases of joint persistence (residence) of viruses of different types in one carrier. This obliges the patient and doctor to be especially attentive to preventive examinations, their quality and regularity to prevent anorectal cancer .
Recovery after deletion
After the doctor removes the condylomas, he will definitely explain the features of the recovery period. In the vast majority of cases, no complications are observed if you follow the specialist’s recommendations for 4-6 weeks:
- Avoid visiting baths, saunas, swimming pools, beaches, solariums;
- Prefer a warm shower to a hot bath;
- Limit physical activity, eliminate heavy lifting;
- Maintain sexual rest
- Use pads and avoid tampons;
- Don't drink alcohol.