Mycosis or skin fungus on the hands develops mainly due to non-compliance with basic rules of personal hygiene.
You can become infected with the fungus through direct contact with a patient, with common household items, the patient’s clothing, as well as when visiting public places - a gym, swimming pool, bathhouse, etc.
The pathogenic organism penetrates damaged skin - microcracks between the fingers, abrasions or cracks. Often cracks between the fingers form due to increased sweating (hyperhidrosis), diaper rash, and professional activity.
Since the nutrient medium for the fungus is keratin, it primarily affects areas of the body with a large amount of protein - skin, nails and hair. The presence of concomitant diseases, decreased immunity, or the use of certain medications can contribute to the widespread spread of the fungus.
Symptoms, signs and diagnosis
It is very important not to miss the first signs of fungus on the hands, which are expressed:
- Peeling of the skin and persistent itching;
- Peeling of the skin, especially between the fingers;
- The appearance of bubbles and swellings in areas affected by mycosis;
- Increased sweating of the palms;
- Changes in skin structure, deformation of nails;
- Various spots on the nails and their peeling;
- Since the fungus can penetrate the human body, pain in different organs is possible.
Diagnosing fingernail fungus is the task of a dermatologist. You should not diagnose yourself and try to solve the problem alone, as this requires taking a scraping for laboratory testing.
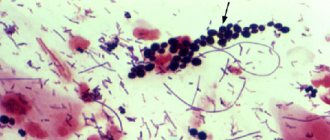
Causes of candida infection
In the external environment, fungi of the genus Candida are found:
- in soil and water contaminated with human and animal excrement;
- on food products - raw meat, fruits, juices, cottage cheese, milk;
- on household items.
This is an opportunistic fungus: in people with a healthy immune system, it is found in the mouth and nose, in the vagina in women, and on the mucous membrane of the digestive tract. There is no fungus in sterile body fluids (blood, cerebrospinal fluid, bile).
Primary colonization of the child’s body by fungi occurs in the mother’s birth canal, and after birth, infection occurs through contact: infection from other people, through household items. In adults, infection can occur through sexual contact. The internal cause of the development of candidiasis infection is severe immunodeficiency conditions, diabetes mellitus, endocrine pathologies.
The main cause of candidal fungus of the skin and nails is a violation of the barrier function of the skin. This can occur with chronic skin diseases: eczema, atopic dermatitis, seborrheic dermatitis, psoriasis. There is an opinion that the prevalence of yeast-like fungi is increased in people with allergic dermatoses. Fungi of the genus Candida are more often isolated in individuals with severe atopic dermatitis. Increased levels of Candida fungus are found in patients with psoriasis.
Photo: Iris_AN / Shutterstock.com
Clinical cases of candidiasis among patients with chronic skin diseases can be explained by the result of the development of immunodeficiency states against the background of chronic diseases, the use of antibiotics, immunosuppressive and hormonal drugs in the treatment of these diseases.
Fungus between the fingers is an occupational disease for those people who have contact with water and food products: confectioners, dishwashers, cleaners.
Photo: sukiyaki / Shutterstock.com
Treatment of fungus on hands
It is necessary to begin treatment with laboratory tests to determine the type of fungal disease. The study will allow us to determine the necessary and effective drug that will successfully combat the detected type of pathogen. In the early stages, mycosis can be successfully treated with antifungal medications - sprays, lotions, creams and ointments. All of these medications have contraindications, so before starting treatment, you need to consult your doctor and follow his instructions.
Fungus on hands photo
Classification
Fungal pathogenic organisms are divided into several groups:
- Anthropophilic - they only affect people.
- Zoophilic - affects exclusively animals.
- Zooanthropphilic - affects all representatives of the fauna.
In medicine, fungal diseases are divided into five groups:
- Keratomycosis (trichosporia nodosum, lichen versicolor ).
- Dermatomycosis (athlete's foot, athlete's foot, rubromycosis, trichophytosis , microsporia).
- Candidiasis (superficial candidiasis, chronic generalized candidiasis, visceral candidiasis)
- Deep mycoses (blastomycosis, histoplasmosis, sporotrichosis, coccidioidosis, etc.).
- Pseudomycosis (superficial and deep pseudomycosis).
Pharmacy remedies for fungus on hands
help well in treating fungus on the hands . To be effective, they need to remain on the affected area for as long as possible. For this purpose, medicinal varnish is also used. Loceryl and Batrafen are considered the most effective: before using them, you need to remove the infected piece of nail with a file or nail clippers.
In the early stages of the disease, it is good to use patches with a peeling effect. When used, the affected area of the nail softens and can then be easily removed. It contains salicylic acid, urea, an antiseptic and an antifungal agent. This patch is wrapped in a simple plaster, left for a couple of days, after which the procedure is repeated. Such treatment will require at least six months.
Fungus on the fingers or between the fingers is treated with medical formulations according to prescriptions, which you can make yourself, knowing the exact composition of the medications. They usually contain vinegar essence, sulfur, iodine, salicylic and lactic acid, brilliant green and blue. Treatment with such drugs is quite long-term and can last more than a year.
New drugs are now available that actively destroy the fungus. The duration of treatment with these drugs is from 2 to 4 months. The most effective is pulse therapy, which lasts only a few weeks. Common medications for oral administration are tablets and capsules. But all drugs can be used only as prescribed by a doctor.
Medicines for mycosis:
- Diflucan
- Mycohepitn
- Clotrimazole
- Fluzol
- Fluconazole
Ointments and solutions:
- Levorin ointment
- Griseofulvin
- Triderm
- Nystatin ointment
- Mycozolon
Diet
Antifungal Diet
- Efficacy: no data
- Terms: 3-6 months
- Cost of products: 1500-1600 rubles. in Week
In the process of treating a fungal disease, doctors recommend following some recommendations. Proper nutrition promotes a speedy recovery and helps fight fungal infections. The antifungal diet requires the following rules:
- Do not consume foods that contain yeast.
- Minimize, or better yet completely eliminate, the consumption of sweets, since carbohydrates are a breeding ground for fungus.
- The use of dishes made by fermentation (kvass, etc.) is contraindicated.
- It is recommended to eat freshly prepared food and consume as many raw vegetables and fruits as possible. It is important to introduce more greens, carrot and orange juice into your diet.
- It is prohibited to consume alcohol.
- During the treatment process, it is important to consume as much fermented milk products as possible in order to normalize intestinal functions.
- It is recommended to drink rosehip decoction, green tea, herbal teas, and mineral water. You need to drink as much fluid as possible.
Traditional medicine against fungus on hands
such remedies for fungus on the hands , the most effective ones are listed below.
Coffee:
- Brew strong coffee without throwing away the sediment.
- Several times during one procedure, lower and hold your hands in warm coffee.
Hot pepper:
- Cut off the bottom of the hot pepper, remove the seeds.
- Pour strong vodka into it.
- Dip the affected finger into the vodka, being careful not to let the vodka spill out.
- Leave for 10-20 minutes, remove the finger and bandage it.
- The bandage must be left overnight.
The process is very painful, but recovery occurs quickly.
Sea salt baths:
- Add 2 tbsp to 2 liters of warm water. l. salt. Mix.
- Systematically hold your hands in a warm solution for 20 minutes a day.
hand fungus
How to eat healthy
Nutrition is of particular importance as it affects metabolism, the disturbances of which underlie the disease. It is useless to treat psoriasis without following a diet. Important: in the patient’s diet, 70% should be products of plant origin and only 30% should be animal products. Recommended to use:
- any fruits and vegetables (fresh, boiled, stewed) except those prohibited;
- fresh juices; Citrus juices are especially useful; lemon juice can be used as a salad dressing;
- more clean water.
Limit consumption (no more than a few times a week):
- lean meat and fish;
- low-fat cottage cheese and fermented milk products;
- cereals;
- some fruits and berries: plums, currants, cranberries, blueberries.
Exclude from the diet:
- fat meat;
- fatty dairy products;
- sweets, baked goods;
- vegetables from the nightshade family: tomatoes, eggplants, hot and bell peppers;
- all spicy, sour, smoked, fried, canned foods;
- drinks: sweet soda, cocoa, strong coffee, tea, alcohol.
Prevention
We should never forget that mycosis is a contagious disease, and if one family member is infected, then, as a rule, everyone else becomes infected. Therefore, you must always strictly follow the rules of hygiene:
- Do not use someone else’s shoes and do not give yours to anyone;
- The infected family member should have separate manicure supplies;
- If you are infected, do not walk around your apartment barefoot.
- Perform daily disinfection of everything the patient has touched;
- Try not to wear socks and tights for a long time.
In order not to become infected with such an unpleasant disease, you should try to avoid visiting public health centers - baths, showers and swimming pools. Carefully monitor personal hygiene and prevent fungal diseases, and immediately consult a doctor at the first symptoms.
In children
In children, such a disease is not uncommon due to non-compliance with hygiene rules, active contacts with peers, pets, etc. But since children may develop other skin lesions associated with allergic reactions, infectious diseases, etc., parents should definitely contact see a dermatologist so that the doctor can determine the diagnosis. In no case should you practice self-medication, since you must initially establish an accurate diagnosis. In addition, many antifungal agents cannot be used to treat children. Parents must not only ensure proper treatment of the disease, but also teach their children the basic rules of personal hygiene.
What can streptoderma be confused with?
Pyoderma
With pyoderma, the sebaceous and sweat glands are damaged. The rash appears in certain areas of the skin - parts of the body, scalp.
Herpetic rash
Herpes is characterized by the presence of blisters with constant inflammatory processes. They burst and provoke development.
Thrush or candidiasis
Candidiasis is characterized by erythematous papules or reddened, wet plaques. In the pathology under consideration, the lesion, as a rule, occurs in the mucous membranes or fold areas.
Manifestations of allergies
An allergic rash continues to occur as long as the influence is the causative agent of the allergy.
Symptoms
If streptoderma occurs, what is the treatment? Before we know the treatment options, let's find out the symptoms. The disease in children occurs in extremely severe forms:
- temperature up to 39C,
- poisoning,
- large lymph nodes.
The texture of the skin may vary depending on the form of the pathology:
- Superficial. Initially, red spots form on the skin. After a couple of days they turn into blisters with a certain liquid inside. The blisters grow up to two cm in diameter, after which they rupture. Yellow crusts form in this area. After this, the skin in this area heals, and the pathology develops further.
- Dry streptoderma . This form usually occurs in boys. Light and pink spots up to 5 cm in diameter form on the skin. They are found everywhere on the body. After they disappear, scars may remain.
- Streptococcal infection. The pathology extends specifically to the corners of the lips; it is encountered when there is a deficiency of vitamin B. Small cracks form on the skin, causing discomfort. After some time, they form into pustules that become crusty. The child has difficulty consuming food, as it causes pain.
- Felon. In a situation where streptococcus spreads to the area around the nails, panaritium develops. Oddly enough, this disease is more often encountered by children at an early age who bite their nails.
- Streptococcal diaper rash. This form of pathology is typical for breastfed children. Blisters form in the folds of the skin.
Understanding how streptoderma begins to develop in children, treatment which requires timely contact with a dermatologist and the implementation of therapeutic actions, not a minute can be lost. If you constantly put off going to the doctor, the pathology can develop into a chronic form, and it will be almost impossible to achieve a final cure.
streptoderma, treatment
Types of disease
- Streptococcal impetigo. The most common standard form of the disease. A characteristic rash forms on the face, arms and legs. This form is also the most limited, since the pathogen does not move beyond the upper layer of the skin, which has certain protective mechanisms. The appearance of the integument does not change, only individual blisters with liquid appear on the reddened areas. Initially, the patient will experience itching, after which the blisters become darker, which helps the blister to crust over. The duration of this process reaches one week. However, it is worth remembering that if the rash resolves, bacteria are further transferred to healthy areas of the integument, which has its negative consequences for the sick person.
- Bullous impetigo. The rashes are located on the arms and legs and had a fairly impressive diameter. Once the blisters open, these areas of skin develop ulcers that can spread quickly.
- Streptococcal diaper rash. Most of the patients are young children and overweight people. The location of the rash is under the mammary glands, in the axillary folds, intergluteal or inguinal-femoral folds. If you are overweight, the abdominal area is affected.
- Ringworm common. Appears in the form of bright pink rashes. The place of appearance is the face. The rash may become smaller due to exposure to direct sunlight. Those areas of the skin that are affected will not take on a tan like before.
- Streptococcal infection is characterized by the formation of blisters in the corners of the mouth. After the blisters disappear, a crack appears in their place, which in a matter of minutes becomes covered with a yellow crust. It also happens that children tear off the crust, but it forms again.
- Streptococcal ecthyma is the most complex form of the disease. The disease is accompanied by the appearance of characteristic lesions and scars on the arms and legs. In case of development of ecthyma, as a rule, there is a deterioration in health.
Therapy
Streptoderma has occurred ? Even in cases where the initial examination was carried out by a pediatrician, only a dermatologist can select therapy. Doctors in this field have an understanding of drugs with a narrow scope of action.
The first step is to limit the child’s diet. The course of treatment also involves avoiding water procedures, which can cause the spread of the disease. Healthy areas of the skin should be washed with a solution of chamomile, and damaged areas should not be touched at all.
The sick person needs to choose the right wardrobe, from which items of clothing made from synthetics and wool must be removed.
Doctors advise popping blisters that form on the skin with a disinfected needle, after which the abscess should be drained twice a day. Healthy areas of the skin are washed with a boron solution.
If crusts appear on the skin, they should be treated with antibacterial gels or ointments.
In more complex situations, many other medications may be prescribed:
- antibiotics for streptoderma of the tetracycline or chloramphenicol series,
- means that prevent the occurrence of an allergic reaction,
- means aimed at improving the body's immune system,
- vitamin preparations,
- antipyretic.
The set of medications must be discussed with the doctor. With the right treatment, the symptoms disappear within a week, but after the severe form is eliminated, scars may remain. This is what streptoderma looks like .
what does streptoderma look like?