- Symptoms
- The initial stage of toenail fungus (photo)
- The initial stage of fingernail fungus (photo)
- Treatment of the initial stage of onychomycosis
- Prevention
The initial stage of nail fungus on the toes and fingers has the same symptoms. Unfortunately, not everyone pays attention to them, which leads to aggravation of the pathological process.
Unpleasant cosmetic defects in the future threaten complete loss of nails and blood poisoning. To prevent these complications, it is important to diagnose and begin treatment of onychomycosis at the very beginning of the disease.
Causes of fingernail fungus
Fungi are ubiquitous in the external environment. They love moisture and warmth. Almost all organs and systems of the human body are affected, including fingernails. Human hands are a unique tool created by nature itself. They are constantly in contact with many objects, and therefore are significantly exposed to environmental factors, including microbial ones. Fingernail fungus does not always develop upon contact with a pathogen. Good immunity and personal hygiene protect a person from this disease.
Rice. 1. In the photo, fingernail fungus (onychomycosis) is one of the most common diseases throughout the world.
The main part of onychomycosis is caused by a fungus of the species Trichophyton rubrum (red trichophyton). Much less frequently, the source of the disease is fungi of the species Trichophyton interdigitale, Epidermophyton floccosum, Microsporum, Aspergillus and Candida albicans.
Red trichophyton spreads throughout the body through the blood and lymphatic tract. This is evidenced by damage to the nail from the posterior area (proximally) and the detection of the pathogen in the lymph nodes of the groin area and the secretion of the prostate gland. This form of onychomycosis is rare. The disease is often registered in HIV-infected people.
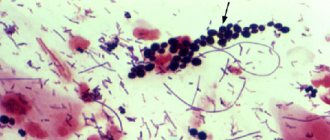
Rice. 2. In the photo, the fungus Trichophyton rubrum (red trichophyton) is the main culprit of onychomycosis.
Prevention
Compliance with preventive measures will minimize contact with pathogens of onychomycosis, and, therefore, prevent infection with nail fungus.
Recommendations for preventing infection:
- You cannot walk barefoot in a public place (swimming pool, sauna, etc.). When going to such establishments, take individual rubber slippers with you.
- Shoes should be purchased from natural materials. It should be comfortable and not injure the skin.
- It is forbidden to wear someone else's shoes. If we are talking about trying on in a store, you should definitely put new models on the sock.
- For salon manicure and pedicure, it is advisable to purchase your own tool and disinfect it yourself. Only in this case can you remain confident that no pathogenic microflora from a stranger will be transferred to the nails during caring procedures.
- After hygienic procedures - shower or bath, you should wipe your feet and hands dry.
- A strong immune system can prevent most pathologies. Multivitamin and mineral complexes sold in pharmacies will cope with this task perfectly.
- If the nail is damaged or scratches or cracks appear on the skin of the hands and feet, you need to treat them immediately, as this is the entry point for infection.
No one is protected from mycoses. Even with careful adherence to hygiene rules, it is quite difficult to exclude the possibility of fungal infection. If the first signs of onychomycosis occur, you should consult a doctor as soon as possible. The sooner treatment begins, the less harm the pathology will cause to the body.
What is the source of infection
- Diseases in your family and friends can become a source of pathogens for you too. The fungus is transmitted within a family through the use of shared towels, bed linen, etc.
- Fungus on the skin and nails of the feet can become a source of onychomycosis of the hands.
- The fungus lives in large quantities in bathhouses, showers and swimming pools.
- The source of fungi can be the patient’s clothes and shoes, manicure sets, carpets and floors.
Rice. 3. The photo shows fingernail fungus.
Epidemiology and risk factors for onychomycosis on the hands
Dermatophyte fungi
The reservoir and source of dermatophyte fungi is a sick person, from whom pathogens are transmitted through his personal belongings or through direct contact. The risk of infection increases if one of the family members has mycosis. In the chronic course of rubromycosis, the infection from the feet often spreads to the working hand and nails.
The infection is transmitted through the patient's personal belongings, including a towel, washcloth, shoes, manicure accessories, etc. Infection of the feet often occurs in swimming pools, saunas, showers, beaches and gyms. Red trichophyton lives for a long time on wooden floors and decking.
Risk factors:
- Diabetes mellitus and vascular diseases.
- The presence of diseases that weaken the immune system.
- Hereditary predisposition.
- Visiting beauty salons where infected instruments are used for manicure procedures.
- Nail injuries.
Rice. 4. About 80 - 90% of all cases of the disease are caused by dermatophyte fungi, of which 70 to 90% are caused by Trichophyton rubrum.
Yeast-like fungi of the genus Candida
Yeast-like fungi of the genus Candida are saprophytic flora. They constantly live in the body of a healthy person. Their development is inhibited by the normal functioning of the immune system. Active growth of fungi is promoted by long-term use of antibiotics, use of contraceptives, glucocorticoids and cytostatics, endocrine pathology (often diabetes mellitus) and other diseases. Pathogens enter the nails from the skin or lymphogenously. The disease often begins with inflammation of the periungual fold. Warmth and moisture are optimal living conditions for fungi of the genus Candida.
Risk factors:
- Humidity and elevated ambient temperature.
- Constant contact with water.
- Wearing false nails.
- Immunodeficiency states.
- Diabetes mellitus and vascular diseases.
- Failure to comply with personal hygiene rules.
Rice. 5. According to European researchers, onychomycosis on the hands caused by Candida fungi ranges from 40 to 60%.
Molds
Molds live in the soil. Their spores end up on food, things and environmental items. Mold onychomycosis does not spread among people. Fungi penetrate damaged nail plates from outside.
Risk factors include severe immunodeficiency and nail injuries.
Rice. 6. A risk factor for mold onychomycosis is wearing false nails and shellac (Shellac) - applying professional varnish and liquid gel.
Rice. 7. Lesions of nails by yeast-like fungi, mold fungi and Pseudomonas aeruginosa are similar to each other. To diagnose the disease, microscopic and microbiological examination is carried out.
What provokes the development of onychomycosis
- Warm and humid environment, climate.
- Constant stress.
- Unhealthy diet, which is replete with sweets.
- Insufficient hand hygiene.
- Artificial nails, under which fungi live and develop in damp places. It is especially dangerous to wear artificial nails for more than 3 months.
- Reduced immunity and susceptibility to disease.
- Long-term use of antibiotics and oral contraceptives.
- Disease diabetes mellitus.
Mold on the nail under the gel? What is this? Photo
Masters in beauty salons can save on materials. This will lead to problems with the health of the nails - detachment of the artificial nail plate from the natural nail.
Moisture accumulates in the resulting pocket, and mold appears on the nail under the gel. What is this and how to fix it? Photos allow you to clearly see what this defect of an incorrectly performed procedure looks like.
The natural nail plate may become deformed. A woman should monitor the condition of her new nails.
IMPORTANT: If mold appears under the extended nails, then you need to go to the salon and have them removed.
If this is not done in a timely manner, the disease onycholysis may develop. The nail will change its color, and then recovery and treatment will take at least six months. In addition to mold, stains from ingrained materials may appear. Only a qualified technician will be able to determine the cause and origin of green spots on the nail plate.
How the disease develops
More often, fungi enter the nail through the nail bed, where they penetrate through small cuts and cracks in the skin. With good health and strong immunity, the fungus does not develop.
Nail fungus progresses slowly. If left untreated, the infection spreads to other areas, eventually completely destroying the nail plate.
Onychomycosis often recurs. Up to 20% of people become ill again after successful treatment. Affected nails can become infected with bacterial flora and then acute paronychia occurs (inflammation of the tissues located around the nail plate).
Rice. 4. The photo shows fingernail fungus.
Why is onychomycosis dangerous?
When the nail plates are affected by pathogenic fungi, this poses a serious danger to the body. This is not a cold that can be cured quickly and with the help of available drugs.
During their development, fungi synthesize toxins. Accordingly, they provoke the development of dangerous somatic processes, such as:
- Inflammation and soreness of the dermis.
- The presence of blisters and toxicodermic skin lesions.
- Generalized necrosis.
- Spread of the fungus through the bloodstream to other organs and systems of the body.
- Complete destruction of the nail plate in the absence of proper treatment.
- Toxins can trigger the development of cancer.
Signs and symptoms of fingernail fungus
The following clinical types of onychomycosis are distinguished:
Onychomycosis. Normotrophic type.
The configuration of the nail plate and its thickness do not change for a long time. But in its depths and along the edges you can see spots and stripes ranging from white to dark yellow. Over time, the painted areas merge, occupying the entire plate. The back of the nail (near the lunula) remains unaffected by the lesion.
Rice. 5. The photo shows the first signs of fingernail fungus. The appearance of the lesion resembles a splinter (or a yellowish spot).
Rice. 6. The photo shows fingernail fungus. Normotrophic type of onychomycosis.
Onychomycosis. Hypertrophic type.
Rice. 7. The photo shows fingernail fungus. Hypertrophic type of onychomycosis.
With this type of onychomycosis, a fungal infection causes hyperkeratosis of the skin of the nail bed. The nail above it thickens, and white spots and yellow stripes appear in its thickness. The nail plate begins to lose its substance, as a result of which its appearance has a peculiar “corroded” appearance, sometimes covering the entire area of the plate. If hyperkeratosis is highly developed, then the nail acquires a lumpy appearance and a change in the direction of growth (onychogryphosis). Onychogryphosis can be seen more often on the legs
Onychomycosis. Onycholytic type.
Rice. 8. The photo shows fingernail fungus. Onycholytic type of onychomycosis.
There is a rapid separation of the nail plate from the nail bed from the side of the free edge. Its color is whitish or whitish yellow and its surface remains smooth. Often, several clinical forms of the disease can be seen in one patient.
Rice. 9. Separation of the nail plate from the nail bed from the free edge is a sign of onycholytic type of nail fungus.
Rice. 10. The photo shows the consequences of fungus on the hands - destroyed nails.
Symptoms
The incubation period after the introduction of pathogens of mycotic infection into microcracks in the nails and skin, until the first signs of pathology appear, lasts several weeks. During this time, fungal spores try to penetrate the nail plate as deeply as possible, beginning active growth and development.
The initial symptoms of mycosis become noticeable by the end of the first month after the infection occurs.
Many people become ill as a result of visiting a public bath, swimming pool, sauna or beach. They notice that their nail color has become duller and their skin is itchy and slightly irritated. But at this stage, not every person suspects a fungal infection.
By the way, healthy nails are practically not susceptible to infection by this disease. Damaged nail plates and people with low immunity are not protected from onychomycosis pathogens.
Diseases with similar symptoms
Of all infectious diseases, onychomycosis occurs in 50% of cases. Similar symptoms occur in the following diseases:
- Eczema.
- Psoriasis.
- Reiter's syndrome.
- Darier's disease.
- Lichen planus.
- Pachyonychia.
- Lichen planus.
- Norwegian scabies.
Rice. 12. Nail damage due to psoriatic arthritis.
Rice. 13. The photo shows green nails. Onychia pseudomonas. The disease is caused by the colonization of Pseudomonas aeruginosa in the cavities under the nails.
Rice. 14. The photo shows nails after chemotherapy.
Rice. 15. The photo shows the appearance of nails after injury.
Symptoms and possible complications
Poor quality manicure is the cause of the development of Pseudomonas aeruginosa. Most manicurists believe that the cause of green nails is a common fungus.
On the one hand, it is easy to confuse due to the presence of a blue-green coating, but only pseudomonia is pathogenic for the body, unlike fungus. Such a mistake by a manicurist can be costly. While the client tries to cure an ordinary fungus, spending money on medicine, Pseudomonas aeruginosa will continue to develop. The consequences of such negligence can be dangerous for the entire body.
The entire nail platinum is affected by pseudomonia within two weeks after extension. Fingers become red, swollen and painful. It is possible that the infection may spread to soft tissues and infect the entire body. Such cases, fortunately, are the exception rather than the rule.
When the first signs of changes in the nail appear, consult a doctor immediately. At the initial stage, eliminating Pseudomonas aeruginosa is not difficult.
Diagnosis of fingernail fungus
To obtain information about what causes nail damage, you need to consult a dermatologist who will organize a procedure for diagnosing the disease. A scraping from the affected part will be sent to the laboratory to determine the causes of the disease.
Microscopy will reveal the presence of the pathogen, and culture will determine the type of fungus and its sensitivity to antifungal drugs.
Rice. 16. Photo shows Trichophyton rubrum under a microscope and growth on a nutrient medium.
How to treat an advanced condition?
If the patient ignored the initial stages of the disease and also did not follow the rules, then the disease becomes advanced. The nails become thick, lumpy and gray-yellow in color. Caring for them becomes impossible.
Important . If the matrix is damaged, the nail peels off from the skin and falls off.
The infection also spreads to the hands. Excessive dryness, peeling and cracks occur. The activity of the sweat glands increases and the patient’s hands constantly hurt and smell bad. In case of a complicated clinical picture, it makes sense to use local, folk and medicinal treatment with tablets.
Previously, in such cases, surgical methods were used to remove the nail plate affected by the fungus. But this method is painful and healing of damaged areas takes a very long time. In such cases, an excellent solution is the avulsion method. It involves the chemical “dissolution” of diseased nails with the help of special medications.
The best external remedies - ointments and varnishes
Most often, doctors prescribe the following drugs to treat mycosis:
- Lamisil ointment has a wide spectrum of action. The duration of treatment is 3 weeks.
- "Exoderil" in the form of a cream is effective in the treatment of mold and yeast fungi, as well as dermatophytes.
- "Mikonorm" in the form of a cream is a very effective remedy that promotes rapid recovery.
- "Fundosil" is a cream based on zinc and salicylic acid. Suitable for treating all types and forms of fungus.
- Nizoral must be applied several times a day. This is one of the few drugs that has no side effects.
Sometimes, in the fight against the disease, special medicinal varnishes are used, which are used in parallel with ointments and creams.
- "Batrafen" is a varnish based on ciclopirox. Treats 57 types of fungus.
- "Loceril" is an antifungal varnish against many types of fungus.
- "Fukortsin" is an antiseptic and disinfectant solution of bright pink color. Effective against all types of fungus. It is necessary to apply the drug twice a day for two weeks.
- “Demikten” is a varnish based on formic acid. You need to apply it daily until a healthy nail grows out.
All drugs with a local spectrum of action must be used according to the same scheme:
- Wash and clean the surface of the nail plate.
- Trim and file the free edge as far as possible.
- Disinfect tools after treating each nail.
- The prescribed product must be used regularly and in full accordance with the instructions or doctor's prescriptions.
Pills and medicines
Oral medications do not treat fungus alone. Therefore, their use is advisable only in combination with local remedies. The most common and effective are:
- "Ketoconazole" - the drug inhibits the development of fungi, but causes side effects: nausea, weakness.
- "Futsis" is used at any time of the day. The dosage is prescribed by the doctor and changes it throughout the course of treatment.
- Fluconazole can only be used as prescribed by a doctor. The course of treatment lasts until the healthy nail grows completely, and the dosage is prescribed by the doctor.
- Terbinafine is prescribed only to adults and children over 12 years of age.
Important . If after treatment there is no result, then it is necessary to re-take tests and undergo an examination.
Effective folk recipes
Home remedies will not work without the use of medications, but they will provide relief if necessary.
- Hydrogen peroxide is an excellent antiseptic, but the drug does not kill fungus. Good for disinfection only. Peroxide lotions should be done in addition to the main treatment.
- Propolis is suitable for preparing baths. Add 1 teaspoon of propolis tincture to warm water and hold your hand and fingers in the container for 10 minutes. Then apply propolis to your nails and put on gloves on top. The compress is left overnight.
- Tar soap gives good results in the treatment of mycosis. The affected areas must be soaped, sprinkled with salt and secured with a sterile bandage.
- the garlic in half and apply a clove to each nail. To improve treatment results, it makes sense to take garlic tincture daily before meals.
- Tea tree oil has antiseptic, antifungal and antibacterial effects. It should be applied to the nails twice a day and rubbed in a little.
- Vinegar is mixed with glycerin in equal proportions. The solution must be lubricated on the nail plates several times a day for a month.
- A 5% iodine solution works well against fungus, as it has antiseptic properties. Infected areas should be treated twice daily. During treatment, a burning sensation will occur - this is the effect of the drug. After seven days, complete regeneration of the nail plate will begin.
Each of the folk remedies helps to alleviate the condition, remove discomfort and speed up recovery.
The video presents several folk recipes for treating fungus on the hands:
Hardware treatment methods
A medical manicure using a device is carried out only if the fungus has not managed to penetrate deeply into the nail plate. The specialist removes the top layer of the affected parts of the nails with a milling cutter along with mycosis.
Should I take pills?
Fungus tablets are the most effective way to treat all types of mycosis .
However, treatment must be comprehensive and according to a specific system prescribed by the doctor. Before starting treatment, the doctor must check the condition of the patient’s kidneys and liver using tests and ultrasound diagnostics. In the initial stages of the fungus, you should not take such serious medications.
Treatment of fingernail fungus
Onychomycosis is difficult to cure. The disease is difficult to treat and can accompany the patient throughout his life.
What is the basis of treatment?
- The use of general and local antifungal drugs.
- The use of drugs that improve blood circulation in the small vessels of the extremities.
- Antifungal treatment of personal belongings and household items.
- To prevent relapse of onychomycosis, antifungal varnishes are used.
Treatment methods for fingernail fungus
A dermatologist has a whole series of medications and techniques at his disposal.
- For mild to moderate fungal infections, ointments, creams, lotions, drops, sprays, gels and varnishes are used, which are applied to the damaged nail and surrounding tissues. They are sold in pharmacies without a doctor's prescription and are standard drugs for the treatment of onychomycosis. They have no side effects and provide long-term therapy. Modern antifungal drugs include intraconazole, terbinafine and fluconazole. They linger for a long time in the affected areas and do not penetrate the blood. They work well for mild and moderate forms of the disease.
- For moderate and severe onychoses, tablets are used. Taking them increases the chances of cure and requires constant medical supervision due to a number of side effects.
- In some cases, laser therapy is effective.
- For severe and recurrent fungal infections, the nail can be removed surgically or non-surgically.
- When a bacterial infection occurs, antibiotics are prescribed.
- With superficial onychomycosis, some patients are helped by tea tree oil and cream.
Before starting treatment for fingernail fungus, it is necessary to identify the type of infection. Do not self-medicate. Only a doctor will select adequate treatment and be able to help you.
Treatment of nail fungus with systemic antifungal drugs
Treatment of onychomycosis with tablets is used for moderate and severe onychoses. Taking them increases the chances of curing the fungus, but requires constant medical supervision due to a number of side effects.
For the treatment of onychomycosis, 2 groups of antifungal tablet drugs are used:
- Group 1 of drugs (azoles) is represented by intraconazole, fluconazole, ketoconazole;
- Group 2 drugs (allylaminamines) are represented by terbinafine, naftifine.
The selection of single, daily and course doses of antifungal drugs is carried out only by a doctor.
Rice. 17. The photo shows remedies for nail fungus - medications of 2 main groups in tablets and capsules.
Before treating fingernail fungus, you must carefully read the instructions for the drug and the description of the treatment method.
Local treatment of nail fungus
With local treatment, high concentrations of antifungal drugs are created on the surface of the nail plate. But where the fungus develops (in the nail bed), the concentration of medicinal drugs is insufficient.
Topical remedies for nail fungus are:
- varnishes: Loceryl, Batrafen, Cycloperox. Demicten, Neil expert;
- creams: Lotseril, Nizoral, Microspor, Exoderil, etc.;
- sprays: Daktarin, Lamisil, etc.
- solutions: Lotseril, Exoderil, Clotrimazole, Terbinafine, Bifonazole, Cycloperox.
Rice. 18. An effective remedy for fungus is Lamisil cream, ointment, spray and solution.
Antifungal drugs in the form of solutions, varnishes and ointments, as a single-component treatment, are used in case of damage to the nail plate of no more than 2/3 of its area.
Creams and ointments
Creams, ointments and sprays are more often used in the treatment of fungal skin infections. Creams, ointments and sprays are more often used in the treatment of fungal skin infections. They create a high concentration of antifungal drug in the area of application, but also help soften the skin by moisturizing it.
Rice. 19. Antifungal creams are more often used for skin lesions.
Rice. 20. In the photo there are remedies for fungus - antifungal creams Lamisil, Clotrimazole and Terbinafine.
Solutions
Antifungal drugs in the form of solutions are widely used to treat onychomycosis. The liquid form promotes deep penetration and the creation of a high concentration of the drug.
Antifungal drugs in the form of solutions are used in case of damage to the nail plate of no more than 2/3 of its area. It is also recommended to use these drugs to prevent the disease.
Rice. 21. Remedies for nail fungus in liquid form Exoderil and Thermikon.
Rice. 22. An effective remedy for nail fungus is Loceryl and antifungal serum Mikozan.
Rice. 23. Local use of the antifungal drug Irunin.
Lucky
Antifungal drugs in this form are used only in the initial stages of the disease. Therapeutic varnishes soften the nail plate and significantly increase the concentration of the antifungal drug in it. Used several times a day (Neil Expert) or once or twice a week (Loceryl). The varnish treatment procedure is described in detail in the instructions.
Before applying medicinal antifungal varnish, the nail plate must be thoroughly cleaned. The polish must be applied daily until a healthy nail grows. The effectiveness of this method ranges from 10 to 50%.
Rice. 24. Effective means for the treatment of nail fungus in the initial stage and for prevention - varnishes Batrafen Neil expert.
Rice. 25. The photo shows the application of keratolytic colloidal varnish.
Additional treatment
For mild fungal infections of the nails, some patients benefit from tea tree oil and cream.
Treatment of fingernail fungus will be successful if you are patient and do not interrupt the treatment. Nail plates on the hands grow faster than on the feet, which is why treatment results can be seen in the shortest possible time.
Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Principles of treatment
Onychomycosis (fingernail fungus, toenail fungus) is a fungal infection of the toenails or fingernails that affects any component of the nail complex, including the base, bed or plate. The disease can be accompanied by pain, discomfort, and changes in the appearance of the nails, which in some cases leads to serious physical and professional limitations, anxiety for patients and a decrease in their quality of life.
In our company you can purchase the following equipment for the treatment of onychomycosis:
- AcuPulse (Lumenis)
In the USA, onychomycosis of the nails occurs in approximately 2–13% of the population, in Canada - in 6.5%, in England, Spain and Finland - in 3-8%. According to a systematic review of 1914 articles, the prevalence of onychomycosis is as follows:
- general population - 3.22%;
- children - 0.14%;
- elderly people - 10.28%;
- patients with diabetes mellitus - 8.75%;
- patients with psoriasis - 10.22%;
- HIV-positive patients - 10.40%;
- patients on dialysis - 11.93%;
- after kidney transplant - 5.17%.
Onychomycosis accounts for about half of all nail pathologies and is the most common nail disease in adults. As for the affected areas, statistically, the legs are affected much more often than the arms.
The main forms of onychomycosis are:
- Distal lateral subungual onychomycosis
- Proximal subungual onychomycosis
- White superficial onychomycosis
- Endonyx-onychomycosis
- Candidal onychomycosis
Often patients have a combination of these subtypes, or total dystrophic onychomycosis - damage to the entire nail complex.
Removing a damaged nail using non-surgical techniques
Methods for removing damaged areas of the nail mechanically
You need to take care of your nails constantly. Special care is required if the nails are affected by fungus. Horny masses are constantly growing, which prevents the penetration of drugs. They can be removed with a medical pedicure, using mechanical means (nippers, scrapers and files) and with the help of medications.
Rice. 26. Using wire cutters to remove damaged edge areas.
Nail plates can be treated using a special device (medical pedicure). The procedure is carried out in a beauty salon. The affected part of the nail is easily removed using a special milling cutter.
Rice. 27. Cleaning the nail using a machine using a special milling cutter.
Using medications to soften nails
The technique is used for severe recurrent fungal infections. When using Onychoplast, urea ointment is applied to the damaged nail and dissolves it. Before applying the keratolytic patch Onychoplast, the nail plate is cleaned.
Rice. 28. Iodinol softens the nail and facilitates its painless removal. Used as a compress. Onychoplast is a thick mass. After application to the nail, it is sealed with adhesive tape.
Using nail softening kits
Microspor and Kanespor contain bifonazole, a powerful antifungal agent. The cream is applied to the damaged nail and sealed with a band-aid. The procedure is repeated daily. The entire procedure is described in detail in the instructions.
Using medications to soften nails is a good alternative to surgical treatment. With the help of such patches, damaged nails can be removed painlessly and relatively quickly.
Why do you need to get tested at the first suspicion of onychomycosis?
Many people believe that onychomycosis is an aesthetic problem. Women cope with the fungus especially quickly in the initial stages of the disease. They cover the affected areas of the nail plate with varnish and think that the problem is solved, and if the varnish ceases to serve as a camouflage, they resort to nail extensions.
As a result, the fungus not only moves further along the diseased nail, but also spreads to healthy nail plates. When the woman finally comes to the doctor, it turns out that there is no way to do without taking antifungal tablets that are harmful to the body. It turns out that trying to forget about the fungus leads to even bigger problems.
But these are not all possible complications. The fungus releases harmful toxins into the human body, which affect the decrease in immunity, provoke diseases of internal organs, and contribute to the development of allergic reactions and dermatitis. It practically poisons the patient’s body, so nail fungus must be dealt with at the initial stage, without delaying or hiding the problem under a beautiful coating.
Nail removal
Currently, surgical removal of nails affected by fungus is almost never practiced. The main indication for this is the addition of a bacterial infection or a complete lack of effect from drug treatment (resistant forms of fungi). The addition of a secondary infection occurs quite often with advanced onychomycosis, severe destruction of the nail plate and poor personal hygiene.
If a fungal infection is usually limited to the nails and the surface of the skin, then the bacteria can also infect neighboring tissues. This leads to the formation of pus, its accumulation and the development of a serious inflammatory process. In such cases, it is recommended to remove the nail to more thoroughly treat the bacterial infection. It should be understood that even removing a nail is not a radical solution to the problem of onychomycosis. Regardless of this, antifungal medications must be continued, since the infection is still present in the body and there is a risk of affecting other nails.
An alternative to surgery is to artificially “dissolve” the affected nail (avulsion). There are a number of drugs (nogtivit and its analogues) that promote rapid keratinization of nails and their layer-by-layer death. This method is now widely practiced because it is painless and can be performed at home. However, you should resort to it only after consulting a dermatologist.
Where can you get infected with onychomycosis?
As noted above, this pathology relates to an infectious disease. The fungus penetrates the nail structure from the external environment. Where can you catch onychomycosis?
The sources of infection are considered to be:
- Infected person. Some types of fungal microflora can parasitize not only the human body, but also exist on personal hygiene items and shoes. As a result, short-term contact can introduce a negative microorganism;
- Pets. In nature, there are more than a hundred species of fungi that can be transmitted from animals to humans;
- Public baths, saunas and swimming pools. Some types of fungal infection are able to reproduce without using living organisms. To become infected with pathogenic microorganisms, it is enough to visit public places with high humidity.
What it is?
Onychomycosis is a nail disease caused by a fungal infection. This pathology is very common; in total, 10-20% of the world's population suffers from onychomycosis. The causative agents of infection are most often dermatophytes, somewhat less often - trichophytosis, microsporia and epidermophytosis.
Very often, the activity of dermatophytes is complicated by the concomitant development of yeast-like or moldy fungi, which enhance the negative manifestations of the disease and cause resistance to therapy.
Symptoms of onychomycosis and photos
Each of the three types of onychomycosis has its own individual symptoms (see photo), which also depend on the severity of the disease. The main symptoms that are characteristic of each of the three types of onychomycosis include:
- the presence of an inflammatory process in the area of the periungual fold.
- the presence of dystrophic changes in the nail plate.
- formation of white, yellow spots, stripes inside the nail.
- atrophy of the nail with its separation from the bed.
The disease most often begins with infection of the nail on the big toe. Then the infection spreads to the remaining toes, and then to the hands.
Features of onychomycosis on the hands caused by dermatophyte fungi
Fingernails are affected by dermatophytes in 40 - 60%. The most common are Trichophyton rubrum (70 - 90%) and Trichophyton mentagrophytes v.interdigitale (10 - 20%). The remaining dermatophytes account for about 3% of all cases of onychomycosis. The reservoir and source of pathogens is a sick person. Dermatophytes survive in the environment for more than 2 years. They live in sand, pebbles, stones, on old and diseased trees, wooden flooring, seats and trestle beds.
With rubrophytosis, a hypertrophic type of lesion, distal and distal-lateral form, is more often noted. In 25% of people suffering from mycosis of the feet for a long time, the infectious process spreads to the skin and nails of the working hand first, and then to the second hand.
For epidermophytosis, caused by the fungi Trichophyton mentagrophytes var. interdigitale, fingernails are extremely rarely affected. Pathogens have a pronounced keratolytic ability and quickly destroy the surface of the nail plate (white superficial onychomycosis). Its surface becomes loose and rough, opal-white in color. Mycosis occurs without hyperkeratosis and involvement of the matrix in the pathological process.
With trichophytosis, fingernails are rarely affected. The cause of mycosis is often the anthropophilic fungi Trichophyton tonsurans and Trichophyton violaceum, much less often - Trichophyton mentagrophytes v.gypseum and Trichophyton verrucosum.
When infected with anthropophilic trichophytons, the nail plates on the hands are affected long after the damage to the scalp. At the site of pathogen penetration, a rounded gray-white spot appears in the thickness of the nail plate - the only sign of the disease that exists for a long time. The nail remains shiny and smooth for a long time, but later becomes dull, dirty gray, lumpy, and crumbles easily. In some cases, the posterior cushion becomes inflamed, it becomes swollen and reddish-bluish. The disease lasts for many years.
When infected with zoophilous trichophytons, the nail plates are affected only on the hands, mainly their superficial layers. Inflammation of the nail folds is noted, blisters and peeling appear on them.
Rice. 26. The initial stage of fingernail fungus.