In recent years, the world has seen an increase in the incidence of psoriasis, including among young people.[1] In Russia, according to research, there are about 3 million people suffering from this disease. [2] Psoriasis is a chronic inflammation of the skin that affects joints and even nails. The development of the disease is associated with the immune response and pathological activity of the cells of the upper layer of the skin. [3] A characteristic manifestation of psoriasis is a rash, most often occurring on the extensor surfaces of the arms and legs. Also, rashes can spread to the scalp and various parts of the body.
Advanced and progressive disease significantly affects the quality of life. Patients experience not only physiological, but also emotional discomfort - many patients with psoriasis become fixated on this problem, which leads to depression, rejection of close relationships and isolation.
Choosing the appropriate treatment for psoriasis is a rather difficult task, since there are many theories about the development of the disease, as well as factors that can cause exacerbation. Treatment must be comprehensive; choosing one or another therapeutic measure must take into account the form of the disease, stage, symptoms and individual characteristics of patients with psoriasis. To understand the principles of treatment, it is necessary to establish which factors cause the disease and provoke an exacerbation. The clinical picture of the disease and the severity of the course are also of great importance.
Reasons for the development of psoriasis
One of the most common causes of psoriasis is considered to be a genetic factor associated with sensitization of the immune system and pathologies of keratinocytes (cells of the stratum corneum of the epidermis). Researchers have proven the multifactorial nature of the disease with predominantly genetic determination, with the share of the genetic component being 60-70%, and the environmental component – 30-40%. [4] Unfortunately, scientists have not yet established which genes control the immune system failures that occur in psoriasis. The mechanism of the pathological process is as follows: the immune system gives the wrong signals, so the body, instead of getting rid of the affected skin cells, begins to accumulate them on the surface, forming plaques characteristic of psoriatic lesions.
Also common theories as to what causes psoriasis and exacerbations (more often in the cold season) are:
- viral;
- neurogenic;
- exchange;
- theory of congenital defects of skin capillaries.
Some scientists believe that, in addition to keratinocytes, T-lymphocytes and blood vessels are involved in the pathological process. This leads to the formation of inflammatory foci in the form of various rashes. [3]
Among the reasons for the development of total skin lesions in psoriasis, as well as their exacerbations, the following are considered:
- concomitant viral or bacterial infections;
- alcohol abuse;
- active smoking;
- mechanical damage;
- use of certain medications;
- emotional stress. [5, 6]
Complex therapy of palmoplantar psoriasis using Losterin cream
Dermatologists often prescribe classic cream or foot cream “Losterin” in complex therapy of the active stage of palmoplantar psoriasis, as well as to maintain the disease in remission. However, it can be freely purchased at a pharmacy or online. This is a local non-hormonal remedy. It does not contain aggressive and harmful components, as well as dyes and flavors. Therefore, “Losterin” is absolutely safe.
All products from the Losterin line have been tested in laboratories and confirmed their effectiveness. Doctors often recommend them due to the following advantages:
- ease of use (the drug can be used at home and while traveling without any problems).
- lack of addictive effect (the product can be used every day and for several courses);
- no side effects - the cream is well tolerated and does not cause allergic reactions
- complex effect on the symptoms of the disease - the drug reduces peeling on the surface of rashes, effectively copes with skin redness
- harmless composition;
Losterin gently fights inflammation and eliminates external symptoms.
Symptoms of psoriasis
The clinical picture of psoriasis largely depends on the type and stage of the disease. This or that type of disease is determined by the location of the lesion and the type of rash. Currently, the following types of psoriasis are distinguished: [1]
- Ordinary or vulgar. It appears as dense, flat, pinkish rashes that rise above the skin level and are covered with loose scales. The scales fall off easily, and if they are removed, you can see a reddish surface with small pinpoint bruises. The rashes gradually merge into plaques of various shapes and sizes.
- Exudative. It is characterized by rashes covered with yellow lamellar crusts, which also contain scales. When the scales are removed, the surface of the lesion begins to get wet and bleed.
- Seborrheic. It appears mainly on the scalp, as well as on the nasolabial and behind-the-ear folds, between the shoulder blades, and on the chest. The rash is often accompanied by dandruff, in some cases spreading to the forehead.
- Palmoplantar. It is a rash with very dense scales. It is most often diagnosed in people whose profession involves heavy physical labor.
- Pustular. One of the severe forms of psoriasis, which is accompanied by an increase in body temperature. The rash appears as small, red, scaly blisters that most often appear on the palms of the hands and soles of the feet. Patients also complain of pain and burning in the affected areas.
- Arthropathic. In addition to skin rashes, the disease also manifests itself as joint pain, stiffness and swelling. With multiple episodes of exacerbations, the disease can deform the joints, and with further progression, even lead to disability.
- Psoriatic erythroderma. A disease with very rapid development and acute manifestation. Symptoms include severe redness and swelling, many scales merging into plaques. Patients may develop a fever and possibly experience joint pain. [1]
Sometimes psoriasis can affect the nails, deform them and change color. The affected nails may develop grooves and thickenings, they become brittle, and in some cases there is even discharge from under the nails.
There are three stages of psoriasis:
- Progressive - the appearance of new elements of the rash, an increase in vesicles and nodules, their fusion into plaques.
- Stationary – manifestations stabilize and stop.
- Regressive - gradual disappearance of the rash, delayed peeling, appearance of colorless spots at the site of the rash. [1, 7]
Types of palmoplantar psoriasis
There are two main types of palmoplantar psoriasis: ordinary and pustular (Barber type).
Ordinary psoriasis manifests itself as follows:
- In the area of the palms (often closer to the big toe and little finger) or soles (heel, lateral surface of the foot and area of the metatarsophalangeal joints), clearly defined, inflamed areas of reddish-yellow skin form. With severe exacerbation of the disease, the rash may occupy the entire palm or sole.
- in some cases, a large number of rough scales accumulate on the surface of the rash, forming deep and painful cracks
Pustular palmoplantar psoriasis (Barber psoriasis) is additionally characterized by the presence of pustules - intradermal accumulations of whitish-yellow pus. Purulent rashes can form both on top of plaques and on clean skin.
The pustular subtype develops quickly, is characterized by frequent relapses and is difficult to treat. Treatment for Barber psoriasis differs significantly from treatment for other subtypes.
Features of treatment
Taking into account the large number of provoking factors, as well as the various manifestations of psoriasis, many treatment approaches have been developed. The most effective is considered to be a combination of drug therapy and non-drug measures. Also, many doctors emphasize the importance of diet and skin care. Patients are advised to reduce their consumption of fatty foods, give up alcohol, as well as confectionery and flour products. The diet should be dominated by proteins, which can be obtained from lean meat and fish, vegetables and dairy products. [7]
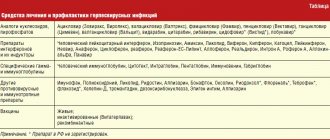
In the drug treatment of psoriasis, topical agents are used. They are aimed at reducing inflammation and peeling. The most effective are creams and ointments containing salicylic acid, as well as external glucocorticosteroids. [8]
Palmoplantar psoriasis in the photo with description
Photo 1. Provoking factors for psoriasis: obesity.
Photo 2. Provoking factors for psoriasis: smoking and alcohol.
Photo 3. Psoriasis on the palms.
Photo 4. Psoriasis on the soles of the feet.
Photo 5. Symptoms of palmar psoriasis: peeling and the appearance of a red crust.
Photo 6. Symptoms of palmar psoriasis: peeling of the nail plates.
Drug therapy with Akriderm drugs
Of all the Akriderm preparations presented, it is more advisable to use Akriderm SK ointment to combat psoriasis. This is a combination ointment containing both glucocorticosteroid and salicylic acid. Thus, it affects the source of inflammation in several ways:
- has an anti-inflammatory effect;
- provides antiseptic effect;
- has antiallergic properties;
- eliminates horny layers.
Salicylic acid promotes deeper penetration into the site of inflammation through skin thickened by psoriasis, where the glucocorticosteroid delivers a powerful therapeutic blow. Thanks to this thoughtful composition, Akriderm SK ointment acts quickly and has a favorable safety profile. It can also be used on the scalp. [9]
links to sources
- D.K. Nazhmutdinova. Clinical manifestations and treatment of psoriasis. Medical Council, No. 4, 2007, pp. 15-20.
- World Health Organization. (2016). Global report on psoriasis. World Health Organization.
- Berdnikova E. R. On the issue of the immunopathogenesis of psoriasis / Berdnikova E. R., Filimonkova N. N., Tuzankina I. A. Immunology. Allergology. Infectology. 2004; 5:27–30.
- Kungurov N.V. Peculiarities of inheritance of psoriatic disease based on pedigree analysis / Kungurov N.V., Filimonkova N.N. et al. Modern. problem dermatovenerol. im-munol. and medical cosmetologist. 2009; 3:44–48.
- Gudjonsson JE, Elder JT Psoriasis: epidemiology // Clin. Dermatol. 2007; 25 (6): 535–546.
- Elder L. et al. The association between smoking and the development of psoriatic arthritis among psoriasis patients // Ann. Rheum. Dis. 2012; 71(2):219–224.
- V. A. Molochkov. Psoriasis and psoriatic arthritis. Clinic, diagnosis, treatment. A manual for doctors. Moscow, 2015.
- Batyrshina S.V. Glucocorticosteroids for local use in the modern strategy for the treatment of inflammatory dermatoses in pediatric practice // Practical Medicine, 2014. No. 9 (85). pp. 94–102.
- Instructions for medical use Akriderm® SK.
Current trends in the treatment of palmoplantar psoriasis and acquired limited forms of keratoderma
S.V.
KLYUCHAREVA1, K.S. GUZEV2, V.I. NOZDRIN2 1 – Federal State Budgetary Educational Institution of Higher Education “North-Western State Medical University named after. I.I. Mechnikov", St. Petersburg, Russia, 195256; 2 – JSC “Retinoids”, Moscow, Russia, 111123.
Summary
Keratoderma is a group of diseases united by a common feature - increased keratinization due to an increase in the number of keratinocytes with a decrease in their normal desquamation. Excessive keratinization of the skin of the palms interferes with tactile sensitivity, which becomes a source of discomfort, and cracks lead to loss of performance.
Purpose of the study
— to study the possibilities of using the drug Uroderm for the treatment of patients with acquired limited forms of keratoderma.
Material and methods.
Two groups, equal in terms of the main characteristics, were formed: the 1st group included 37 patients (10 men and 27 women) with a diagnosis of palmoplantar psoriasis, the 2nd group included 39 women with a diagnosis of climacteric keratoderma. Participants in both groups used Uroderm ointment 2 times a day for 30 days.
Results.
A significant reduction in the area of lesions from the initial level was established in both groups (up to 44% in group 1 and up to 19% in group 2). There was a significant decrease in the values of the dermatological index of the symptom scale and the Visual Analogue Scale in group 1 - from 9.64±3.71 and 3.39±1.08 to 2.13±1.04 and 1.19±0, 83 points, respectively, in the 2nd group - from 10.31±3.45 and 3.67±0.97 to 1.01±0.62 and 0.57±0.57 points, respectively. The use of Uroderm ointment allowed, within a relatively short period, to achieve clinical recovery in participants of group 1 - 16 (43.2%) out of 37, or a significant improvement in the condition of representatives of group 2 - 31 (79.5%) out of 39.
Conclusion.
Uroderm ointment has a significant positive effect on the severity of the main objective clinical manifestations of limited forms of keratoderma. The drug has high safety and tolerability rates: representatives of both groups have no cases of complications; None of the study participants had any episodes of allergies or individual intolerances.
Keywords:
keratoderma, psoriasis, urea, Uroderm.
Keratoderma is a heterogeneous group of diseases characterized by diffuse or focal thickening of the stratum corneum of the epidermis of the palms and soles, in some patients in combination with keratoses of other localization, ectodermal dysplasia and inflammation [1–3]. Hereditary palmoplantar keratodermas have common histological features: acanthosis, hyperkeratosis, and sometimes focal parakeratosis. There are small perivascular infiltrates in the upper dermis. Hyperkeratosis and granulosis are observed in the vast majority of diffuse and limited forms of palmoplantar keratoderma [4].
For symptomatic purposes, keratolytics are used to treat keratoderma, one of which is urea. Urea in high concentration denatures and dissolves proteins, thereby providing a keratolytic effect, improves skin hydration and increases desquamation, and reduces skin itching. The advantage of urea is the absence of toxic and allergenic effects on the body. F. Julia et al obtained positive results when treating patients with dry flaky skin with urea preparations against the background of ongoing or previous dermatitis and patients with hand eczema. [5]. P. Oztas et al. [6]. It was found that in psoriasis, external treatment with urea reduces hyperproliferation of the epidermis and induces differentiation of keratinocytes.
Successful examples of the use of drugs with urea for the treatment of keratoderma have been noted, but since they are not yet numerous enough and are not widely used in practice, the search for optimal ways to solve this problem remains relevant. In this sense, the use of a domestic drug, which in its characteristics, content and properties is close to the idea of an ideal remedy for the successful treatment, control and prevention of acquired limited keratoderma (ALK), is promising.
Uroderm drug
- ointment for external use on an emulsion basis, which has a keratolytic effect, softens and moisturizes the skin, increasing its elasticity. The emulsion base of the ointment is easily absorbed by the stratum corneum of the skin, helping to soften the keratin. The concentration of urea in Uroderm ointment is 30% - this is higher than in any other product containing urea. Unlike various cosmetics with urea, Uroderm ointment is a medicinal product with a proven pharmacological effect, produced from pharmacopoeial quality components.
Purpose of this work
— substantiation of the feasibility of using the drug Uroderm as a pathogenetically justified, non-invasive drug for the treatment of patients with POC.
To achieve the goal of the study, standard criteria for assessing the effectiveness of therapy were used: the influence of the therapeutic agent used on the severity of the main clinical signs of the pathological process (criterion 1), the therapeutic effect (criterion 2), the incidence of side effects of therapy (criterion 3), the quality of life of patients in the comparison groups (criterion 4) and consumer properties of the drug (criterion 5).
The grounds for including patients in the clinical trial program were voluntary informed consent to participate in the study, confirmation of the diagnosis of palmoplantar psoriasis (PLP), climacteric keratoderma (KC), age from 21 to 69 years inclusive, the presence of indications and the absence of absolute contraindications to the use of the included into the external therapy program, the possibility of treating the patient on an outpatient basis and compliance with the agreed conditions of the trial, which imply strict adherence to medical recommendations and continued participation in the study until its completion.
Material and methods
The objects of observation were 76 outpatient patients (10 men and 66 women) aged from 21 to 69 years (average age 44.5±9.4 years), suffering from the most common nosological forms of non-hereditary POC, with no signs of a systemic process, with a duration diseases from 3 months to 20 years. The diagnosis of POC was initially made clinically. In order to verify it, the set of preliminary diagnostic measures, along with the collection of anamnesis and physical examination, included mandatory laboratory tests performed in accordance with the recommendations for the diagnosis of keratoderma [5].
Two groups of patients were formed: the 1st group included 37 patients (10 men and 27 women) with a diagnosis of palmoplantar psoriasis, the 2nd group included 39 women with a diagnosis of menopausal keratoderma. The criteria for analyzing the therapeutic effectiveness of the treatment method used in the groups were the following specific and nonspecific indicators.
Criterion 1.
Sign 1 - the dynamics of regression of objective symptoms of the disease, assessed by comparing the areas of affected areas before and after treatment. The current assessment of results is the registration and comparison of the areas of affected areas before and after treatment in absolute values. Presentation of results is a relative change in the areas of affected areas (decrease, increase), observed during treatment and expressed as a percentage of the initial level. Sign 2 is the dynamics of regression of objective symptoms of the disease, assessed by the results of changes in the dermatological index of the symptom scale at each control point of observation. Sign 3 - dynamics of the subjective indicator (index) of the severity of itching, calculated on a 10-point Visual Analogue Scale (VAS) - the most constant sign characteristic of both diseases under consideration on the 10th, 20th and 30th days of observation.
Criterion 2.
Global assessment of the therapeutic effect (adaptation option in relation to the conditions of this study). Comparative analysis of the effectiveness of treatment of POC using the drug Uroderm. Evaluation of results in groups according to the number of patients who achieved clinical recovery (excellent treatment result - a decrease in the severity of a clinical sign as a percentage of 75% or higher from the initial level), significant improvement (a good treatment result - a decrease in the severity of a clinical sign as a percentage of 50 to 75% of the initial level), moderate improvement (satisfactory treatment result - reduction in the severity of the clinical sign as a percentage from 25 to 50% of the initial level), no effect (unsatisfactory treatment result - reduction in the severity of the clinical sign as a percentage of less than 25% of the initial level) level). Presentation of results - assessment of the severity of the studied phenomena before and after treatment (in points). To ensure the reliability of the results obtained during statistical processing of the data, a ranking method was used: an excellent result corresponded to 3 points, a good result corresponded to 2 points, a satisfactory result corresponded to 1 point, and an unsatisfactory result corresponded to 0 points. The assessment control point is the 30th day of observation.
Criterion 3.
Frequency of development of undesirable effects of treatment, comparative assessment of the safety and tolerability of the drug Uroderm in the treatment of POC. Methods for obtaining information: clinical observation data (objective method), questionnaires (subjective method).
Criterion 4.
Changes in the assessment of quality of life based on the dynamics of the Dermatology Life Quality Index. Assessment of psychosomatic status in patients with POC before and after treatment. Analysis of the strength of influence of the only external therapy used in the experiment on the level and quality of physical, mental, social and role-related or functionally associated lifestyle on patients with diseases of various natures. Method: survey. The method is to independently fill out a universal form of a standard questionnaire, which is a Russified version of the Dermatology Life Quality Index or the dermatological quality of life index (DIQL). Control points: 1st and 30th day of observation.
Criterion 5.
Assessing the results and quality of treatment, analyzing consumer properties, studying the reaction and attitude of patients to the use of a new external therapy. Method: survey. The method is to independently fill out a simple questionnaire that allows you to assess patient compliance and further prospects for using the drug in patients with various nosological forms of POC.
Statistical processing was carried out using generally accepted methods of parametric and nonparametric statistics (Excel and Statistica 6.0 programs). To compare qualitative, quantitative and semi-quantitative characteristics, χ2 and Wilcoxon-Mann-Whitney tests were used. Data were presented in the form of absolute or relative (%) values, quantitative - in the form of X±x, where X is the arithmetic mean, x is the error of the average value. The difference in values was considered significant at p
Results and discussion
There were no significant differences in the severity of the assessed clinical manifestations of the disease, as well as significant differences in the assessment of the quality of life at the pre-treatment stage in representatives of both groups: the initial indicators in the comparison groups were statistically indistinguishable (p
Criterion 1.
The strength of the influence of the therapy used on the severity of the main clinical signs of the pathological process (Table 2).
Despite the fact that as a result of treatment, patients in both groups showed positive dynamics, the strength of the effect of therapy on the assessed clinical sign of the pathological process turned out to be different.
Thus, in patients of group 1, the use of the declared drug led to a reduction in the lesion area by 56%, which by the end of the study amounted to 44% of the initial level, which can only be interpreted as a clinically significant positive result (p>0.05). At the same time, patients in group 2 showed a more pronounced reduction in the value of the studied parameter - up to 19% of the initial level (p Table 1.
Distribution of patients by group
| Index | Group | |||||
| 1st (n=37) | 2nd (n=39) | Total | ||||
| abs. | % | abs. | % | abs. | % | |
| Number of participants | 37 | 39 | 76 | 100 | ||
| men | 10 | 27,0 | — | — | 10 | 13,2 |
| women | 27 | 73,0 | 39 | 100 | 66 | 86,8 |
| Area of lesions, cm2 | 32,5±15,7 | 38,9±17,4 | ||||
| DISHS | 9,64±3,71 | 10,31±3,5 | ||||
| VAS | 3,39±1,08 | 3,67±0,97 | ||||
| Dermatology Life Quality Index | 12,2±1,3 | 12,0±1,0 | ||||
Table 2.
Change in the area of lesions during treatment
| Group | Change in horizontal area of lesions, cm2 | |||||||
| 1 | 2 | 4 | ||||||
| abs. | % | abs. | % | abs. | % | abs. | % | |
| 1st (n=37, N=107) | 32,5±15,7 | 100 | 27,6±12,3 | 85 | 19,6±7,8 | 60 | 14,3±6,5 | 44 |
| 2nd (n=39, N=120) | 38,9±17,4 | 100 | 26,4±13,9 | 68 | 10,7±5,8* | 28 | 7,4±3,4* | 19 |
Note.
Here and in Tables 3, 6: * - within the 95% CI, intragroup differences in indicators relative to the initial level are statistically significant (p
Table 3.
Dynamics of objective and subjective symptoms of disease severity during treatment
| Indicator/index | Group | |||||||
| 1st (n=37) | 2nd (n=39) | |||||||
| observation control points (points) | ||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| DISHS | 9,64±3,71 | 6,28±2,21 | 4,89±1,28*# | 2,13±1,04* | 10,31±3,45 | 4,10±1,02* | 2,53±0,96*# | 1,01±0,62* |
| VAS | 3,39±1,08 | 2,45±0,71 | 1,50±0,67* | 1,19±0,83* | 3,67±0,97 | 1,75±0,66* | 1,09±0,51* | 0,57±0,57* |
Note.
Here and in the table. 6. # - within the 95% CI, intergroup differences in indicators are statistically significant (p
In addition, in group 2, the intensity of the decrease in the value of the studied parameter was more pronounced than in group 1. Thus, a statistically significant reduction in the affected area was observed already by the 20th day of the study.
Preliminary conclusions about the effectiveness of the use of the drug Uroderm in the treatment of POC were also confirmed by analysis of changes in the severity of other clinical symptoms of the disease (Table 3).
During treatment, the average values of DISH and VAS in group 2 decreased statistically significantly from 10.31±3.45 and 3.67±0.97 to 1.01±0.62 and 0.57±0.57 points, respectively (p
Criterion 2.
Global assessment of therapeutic effect (Table 4).
Comparative analysis of the data given in table.
4 demonstrates the differences in treatment results in patients of the 1st (Fig. 1, a, b) and 2nd (Fig. 2, a, b) groups. The advantages of using the drug in group 2 are quite obvious. This is evidenced by the fact that the total proportion of representatives of the 2nd group who achieved clinical recovery - 8 (20.5%) out of 39 and significant improvement - 23 (59%) out of 39 was 79.5%, while as in group 1, the total proportion of study participants who achieved a similar result was almost 2 times less and amounted to only 43.2% (5.4 and 37.8%, respectively). Table 4.
Comparative analysis of the effectiveness of using Uroderm ointment as a monotherapy in patients with palmoplantar psoriasis and climacteric keratoderma
| Result | Group | |||
| 1st (n=37) | 2nd (n=39) | |||
| abs. | % | abs. | % | |
| Excellent (3 points) | 2 | 5,4 | 8 | 20,5 |
| Good (2 points) | 14 | 37,8 | 23 | 59,0 |
| Satisfactory (1 point) | 18 | 48,7 | 7 | 17,9 |
| Unsatisfactory (0 points) | 3 | 8,1 | 1 | 2,6 |
| Average treatment effectiveness score | 1,41 | 1,97 | ||
Criterion 3.
Frequency of development of unwanted side effects of therapy (Table 5).
The data given in table. 5 demonstrate differences in the incidence of undesirable treatment effects in groups when using the studied external therapy. Analysis of the presented results indicates both a greater number of possible complications that arose in representatives of the 1st group, and a higher frequency of cases of their registration than in the 2nd group.
Fig 1.
Patient S., 52 years old, with a limited form of climacteric keratoderma. a — clinical picture of severe hyperkeratosis of the right foot before treatment; b — significant reduction in hyperkeratosis in the area of the right foot after treatment with Uroderm ointment (after 2 weeks of daily application).
Fig 2.
Patient O., 48 years old, with palmoplantar psoriasis.
a - pronounced hyperkeratosis, cracks; b - clinical improvement: epithelization of cracks, reduction of hyperkeratosis, restoration of the structure of the epidermis. Table 5.
Comparative analysis of the safety and tolerability of using Uroderm ointment in patients with palmoplantar psoriasis and climacteric keratoderma
| Symptom | Group | |||
| 1st (n=37) | 2nd (n=39) | |||
| abs. | % | abs. | % | |
| Paresthesia (itching, pain, tingling, feeling of tightness) | 3 | 8,1 | 2 | 5,1 |
| Edema, hyperemia | 3 | 8,1 | 2 | 5,1 |
| Vesicular eruptions, oozing | 2 | 5,4 | — | — |
| Depigmentation, hyperpigmentation | 4 | 10,8 | — | — |
| Peeling | 1 | 2,7 | 1 | 2,6 |
| Telangiectasia | 1 | 2,7 | — | |
| Allergic reactions, individual intolerance | — | — | ||
| Total | 14 | 37,8 | 5 | 12,8 |
Table 6.
Analysis of the strength of influence of the used therapy method (drug) on the quality of life of patients by group
| Chapter | Questions | Group | |||
| 1st (n=37) | 2nd (n=39) | ||||
| before | after | before | after | ||
| 1. Symptoms and sensations | 1 and 2 | 2,1±1,8 | 1,1±0,7 | 1,9±1,2 | 0,6±0,2 |
| 2. Daily activities | 3 and 4 | 1,9±1,7 | 1,0±0,4 | 1,7±1,4 | 0,7±0,3 |
| 3. Rest (leisure) | 5 and 6 | 1,6±1,2 | 0,8±0,4 | 1,5±1,3 | 0,5±0,3 |
| 4. Work and study | 7 | 1,3±0,9 | 0.7±0,5 | 1,4±0,6 | 0,4±0,2* |
| 5. Interpersonal relationships | 8 and 9 | 3,2±1,4 | 1,2±0.7 | 3,2±1,1 | 0,8±0,3* |
| 6. Treatment | 10 | 2,1±0,8 | 2,1±1,1 | 2,3±0,7 | 1,2±0,5 |
| Sum of points | 12,2±1,3 | 6,9±0,6*# | 12,0±1,0 | 3,7±0,3*# | |
Table 7.
Differences in assessing the consumer qualities of Uroderm ointment by group, abs. (%)
| Subjective comments | Comparison group | |||
| 1st (n=37) | 2nd (n=39) | |||
| Yes | No | Yes | No | |
| Presence of side effects | 14 (37,8) | 23 (62,2) | 5 (12,8) | 34 (87,2) |
| Ease of use | 19 (51,4) | 18 (48,6) | 36 (92,3) | 3 (7,7) |
| Availability of additional wishes | 16 (43,2) | 21 (56,8) | 7 (17,9) | 32 (82,1) |
| Satisfaction with the results of therapy | 22 (59,5) | 15 (40,5) | 34 (87,2) | 5 (12,8) |
| Willingness to continue therapy | 26 (70,3) | 11 (29,7) | 36 (92,3) | 3 (7,7) |
Criterion 4.
DIQL assessment (Table 6).
A detailed analysis of the DIQL (see Table 6), carried out in the main sections, showed the presence of clinically significant differences in the assessment of the quality of life before and after treatment by the absolute majority of patients in both groups. The exception was the differences in assessing the degree of influence of the treatment method on this indicator. Thus, if the participants of the 1st group, taking into account previous experience of treatment, did not change their attitude towards it even after these clinical studies (the average score before and after treatment was 2.1 ± 0.8 and 2.1 ± 1.1, respectively), then in patients of group 2 we can state clear positive changes in assessing the effect of therapy on their quality of life (2.3±0.7 and 1.2±0.5 points before and after treatment, respectively). In patients of both groups, a statistically significant decrease in the total indicator (index) of quality of life was registered after therapy: in group 1 - from 12.2±1.3 to 6.9±0.6 points (p
Criterion 5.
Assessment of consumer properties of Uroderm ointment (Table 7).
In a comparative analysis of the consumer properties of Uroderm ointment, the following data were obtained: participants in group 2 were much less likely (in 12.8% of cases) than representatives of group 1 (37.8%) to focus on the presence of side effects of treatment. Significantly less frequently (7.7% versus 48.6%, respectively) made complaints about the ease of use of the drug. Objectively, they expressed additional wishes during treatment less often (17.9% versus 43.2%). Significantly more often (87.2 and 59.5%, respectively) positively assessed the results of therapy and expressed readiness to continue it to the same extent (92.3% versus 70.3%, respectively).
conclusions
The drug Uroderm has a positive effect on the severity of the main objective clinical manifestations of diseases. The drug Uroderm really has high levels of safety and tolerability. The drug Uroderm has a pronounced positive effect on the quality of life of patients with POC who use it as monotherapy for their disease. The drug Uroderm has high consumer characteristics.
The authors declare no conflict of interest.
Literature
- Mordovtsev V.N., Mordovtseva V.V., Mordovtseva V.V. Hereditary diseases and malformations of the skin. M. 2004.
- Isaeva D.R., Haldin A.A. On the issue of differential diagnosis of hyperkeratotic dermatoses of the palmoplantar localization. Clinical dermatology and venereology. 2016;6:120-126.
- Kruglova L.S., Zhukova O.V., Fineshina E.I. Pathogenetic aspects underlying palmoplantar keratoderma. Modern methods of therapy. Clinical dermatology and venereology. 2015;14(2):17-23.
- Paltsev M.A., Potekaev N.N. Clinical and morphological diagnosis. M. 2004.
- Julia F, Phan A, Balme B, Thomas L. Severe palmoplantar keratoderma. Arch Dermatol. 2010;146:667-672.
- Oztas P, Alli N, Polat M, et al. Punctate palmoplantar keratoderma (Brauer–Buschke–Fischer syndrome. Am J Clin Dermatol. 2007;8:113-116.
Psoriatic nail care
Nails and feet affected by psoriasis require regular pedicures. Usually carried out every 2-3 weeks, and if you follow the podiatrist’s recommendations, gentle self-care and the right shoes, a visit to the office is required once every 5-6 weeks.
The podiatrist carefully trims the nails without damaging the adjacent tissues, as a result they do not peel off or crack.
A medical pedicure removes keratinization - a protective barrier that interferes with the external effects of ointments and creams on psoriasis lesions; in fact, keratinization of the feet nullifies the effect of external medications. A mandatory procedure in the complex treatment of the disease.
How to distinguish psoriasis from mycosis?
Nail psoriasis without cutaneous or joint involvement is possible, but occurs only in 5% of cases. So psoriasis usually affects the nail plate and the entire foot.
On the toenails we most often observe changes in the form of dimples, spots similar to vitiligo and normal pigmentation.
Common symptoms of nail psoriasis:
- thimble syndrome - microscopic crop-shaped depressions in the nail plate;
- yellowish-brown color of the nail, similar to a drop of oil;
- longitudinal and transverse grooves - splitting of the nail plate;
- leukonychia - white spots on the nails;
- raised hyponychium – masses of keratinized epidermis accumulate under the nail, which raise the hyponychium, deform the nail, and make it brittle;
- skin edema - painful and swollen skin on the nail folds.
Prevention of palmoplantar psoriasis
Many of the signs of psoriasis on the palms are also common on the feet and soles. Therefore, therapy and prevention are similar.
Basic preventive measures:
- Take daily baths with the addition of natural esters, sea salt or mild baby soap without any additives. Instead of baths, you can do 20-minute baths for your feet and hands.
- Use of moisturizers. Especially after a shower or bath. The product is applied once a day. In advanced cases - twice a day.
- Use soft towels. In this case, the skin is not rubbed, but “blotted” by carefully applying a towel to it.
- Walks in the open air. It is important for people with psoriasis to get enough sunlight. However, moderation is important here. Too much sun will only make the situation worse. Therefore, it is worth consulting a doctor about this issue.
- Rejection of bad habits. Cigarettes, alcohol and lack of daily routine.
- Protection against infections. It is important to monitor your immunity and not have contact with sick people.
- No stress. Or working on changing the perception of negative situations.
These rules must be followed throughout your life. Then the manifestations of the disease will be minimal, and the periods of remission will be longer.
Psoriasis of the skin of the feet - what is it?
Psoriasis often occurs on the foot and spreads to the nail plate. The most difficult case of foot psoriasis is the vesicular form, also known as pustular psoriasis (palmoplantare pustuloese psoriasis). Unfortunately, it is very often confused with mycosis of the skin, sweat eczema, hyperkeratosis of the epidermis caused by excessive sweating, keratosis due to papillary infection, lichen planus or atopic dermatitis.
Nail psoriasis is difficult to hide. Whether we are among colleagues or among friends, affected nails are always visible. They are thickened and yellowish in color.