Among sexually transmitted diseases, fungal infections are becoming increasingly common. Currently, Candida albicans and other species of the genus Candida are considered the main etiological factor of such pathologies; mold fungi and Geotrichum are less common.
Environmental factors play an important role in the spread of genital mycosis:
- industrialization;
- urbanization;
- neglect of hygiene;
- synthetic underwear;
- close contacts in the pool, on beaches, etc.;
- sexual contacts with multiple partners.
Also influenced by various external factors - antibiotics, steroids, cytostatics and immunosuppressants, and internal - impaired immune mechanisms, genetic predisposition, malignant tumors, diabetes, atopic diathesis.
The development of sexual mycosis depends on the number of cells of the attacking fungus and its virulence, that is, the ability to multiply and adhere to the epithelium and the proteolytic enzymes, phospholipases and toxic metabolites produced. Also important is the ability to overcome saprophytic bacterial flora thanks to fungal β-lactam antibiotics, which are derivatives of fucidic acid and streptomycin.
Symptoms
Inguinal dermatophytosis is characterized by an acute onset of the disease. The lesions are pink-red in color and are sharply limited from healthy skin. The surface is peeling. The lesions reach 15 cm in diameter and can unite. Swelling occurs, papules, pustules, vesicles and scales appear.
Since fungi affect keratin-containing tissues (hair, skin, nails), one of the first signs may be the appearance of a hairless area with scales and a rash. There may be lesions with the formation of crusts. Pain and itching appear. Discomfort increases while moving.
Inflammation of the skin most often affects the inguinal folds, the surface of the thighs, and the scrotum, without affecting the genitals.
Publications in the media
Dermatomycosis is a large group of skin lesions caused by pathogenic fungi.
Classification • Keratomycosis (lichen versicolor) • Dermatophytosis: athlete's foot; mycosis caused by interdigital trichophyton (athlete's foot); mycosis caused by red trichophyton (rubrophytosis); trichophytosis; microsporia; favus • Candidiasis • Deep mycoses: blastomycosis, sporotrichosis, chromomycosis, etc.
Etiology. The main pathogens are various species of Trichophyton, Microsporum, as well as several species of the genus Epidermophyton, united under the general name dermatophytes. Morphological identification of pathogens in tissue samples is difficult and requires the isolation of a pure culture. In rare cases, lesions are caused by various species of Candida.
Epidemiology. Most pathogens are widespread in nature, and widespread infection is possible. Diseases are more often reported in countries with hot, humid climates. Among age groups, children are more susceptible to infection. Diseases occur after contact with an active lesion. The following epidemically significant groups of pathogens are distinguished: • Geophilic dermatophytes live in the soil. Infection is possible after contact of a sensitive organism with infected soil • Zoophilic dermatophytes are parasites of most domestic animals (cats, dogs, cattle), a source of infection for humans • Anthropophilic dermatophytes are parasites of humans, transmission of the infectious agent occurs as a result of contact with the patient.
Pathogenesis. In dermatomycosis, the infectious agents are represented by fragments of hyphae and conidia that have entered keratin-containing tissues (the stratum corneum of the skin, hair, nails). The virulence of dermatophytes is low, and damage to underlying tissues is not observed in healthy individuals. All pathogens are characterized by the ability to destroy and utilize keratin. According to the type of growth in the hair shaft, pathogens are divided into 2 groups: endothrix - grow from the skin into the follicles and hair, without going beyond the hair shaft; ectothrix - grow from the hair follicle into the hair.
Clinical picture. Pathogens multiply in the skin and its appendages; diseases are limited, do not pose a threat to life, are often spontaneously limited and cause mainly cosmetic problems. In rare cases, fulminant damage to adjacent tissues is noted, especially in people with immunodeficiencies. It is characterized by itchy round, bright red, clearly defined scaly plaques less than 5 cm in diameter, located singly or in groups.
• Dermatophytosis of the scalp, caused by fungi of the genus Microsporum and trichophytes from the endothrix group, is manifested by brittle hair caused by the growth of the pathogen in the hair shaft • Dermatophytosis of the scalp, caused by trichophytes from the ectothrix group, is often accompanied by purulent melting of the hair follicles and hair loss.
• Dermatomycosis of the beard and mustache. The course can be acute or, less commonly, chronic. Initial manifestations are papules and pustules; later, lesions of the hair follicles appear. As a result of their infection, granulomatous lesions develop, often secondarily infected with bacteria. Swelling of the affected areas is characteristic, the latter are covered with bloody crusts. The main pathogen is Trichophyton verrucosum.
• Body ringworm (tinea corporis). Localized foci of desquamation, pustular rashes, erythema and pyoderma appear on various parts of the body. The main pathogens are Trichophyton mentagrophytes, Trichophyton rubrum and Microsporum canis.
• Inguinal ringworm. It manifests itself as foci of peeling, pustular rashes, erythema and pyoderma in the legs (including the inner thighs), genitals, perineum and groin. The main pathogens are Trichophyton mentagrophytes, Trichophyton rubrum, Epidermophyton floccosum and Candida species.
• Dermatomycosis of the feet. The lesions are localized in the area of the soles, mainly on the skin between the toes; characterized by small bubbles, cracks, scales, areas of softening and erosion. The main pathogens are Trichophyton mentagrophytes, Trichophyton rubrum, Epidermophyton floccosum.
• Onychomycosis. It manifests itself as thickening, roughness and separation of the nails of the fingers and toes. The main pathogens are Trichophyton species; in rare cases, lesions are caused by Candida species. For more details, see Onychomycosis.
• Favus is a fungal infection of the skin, hair and nails with a long-term chronic course and cicatricial alopecia. Etiology: causative agent - Trichophyton schoenleinii; infection occurs through close and prolonged contact with a sick person. Clinical picture • Scutular form. 1 week after infection, erythema appears around the hair follicles, against which scales form, turning into pseudopustules, and then into small, up to several millimeters in diameter, yellowish oval or round crumbling saucer-shaped formations - scutules (scutules are a pure culture of the pathogen). When the scutula is removed or resolved, an erosive or ulcerative surface remains, subsequently cicatricial atrophy of the skin occurs and final alopecia develops. The hair does not break off, but loses its shine, becomes dull, resembling tow • Pythyroid form. Erythematous areas of the skin are covered with tightly packed scales, cicatricial alopecia develops more slowly than with the scuticular form • Impetiginous form. Thick yellow-brown crusts, upon the removal of which cicatricial alopecia develops • With favus, nails can be affected, which become yellow, brittle, and under them, scutulae are visible on the nail bed. Damage to the mucous membranes and internal organs usually leads to death. Research methods, treatment, prevention, see below. Synonyms: scab, lichen favus. ICD-10. B35 Dermatophytosis.
Diagnosis of superficial mycoses is based on clinical manifestations, microscopy data of affected tissues and identification of cultures of microorganisms isolated from them. The causative agents of microsporia are quite easily identified by irradiating the scalp with a Wood's UV lamp (green glow).
Research methods
• Identification of the pathogen by microscopy. Materials for microscopy are fragments of skin and its appendages (nails, hair). The skin sample is placed on a glass slide and a drop of 10% KOH solution is applied. After 10–15 minutes, microscopy of the sample is performed for the presence of hyphae or conidia. Hair microscopy makes it easy to identify pathogens of the endothrix and ectothrix types. Lesions caused by pathogens of the endothrix type are characterized by pits and cavities in the hair shaft, while with pathogens of the ectothrix type, hyphae entwine the hair shaft from the outside. To enhance contrast, use a reduced condenser and matte light.
• Isolation of culture. Place individual hair or skin fragments on nutrient media. Skin samples are obtained by carefully scarifying the lesion with a sterile scalpel or glass slide. The pathogen is identified microscopically and by colony morphology •• Trichophyton species grow in 2–3 weeks; colorful colonies; conidia are large, smooth and septate (up to 10 septa), shaped like pencils (10–50 µm). Intraspecific identification is difficult and requires studying biochemical properties • Microsporum species also grow slowly; macroconidia are thick-walled, multicellular, fusiform (30–160 µm) and covered with spines •• Epidermophyton floccosum forms white, yellow or olive colonies; identified by the presence of many smooth, club-like conidia (7–20 µm long).
Differential diagnosis • Pityriasis rosea • Seborrheic eczema • Contact dermatitis • Syphilis • Psoriasis • SLE.
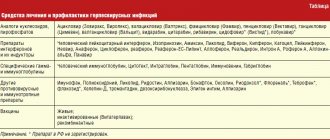
Treatment • Synthetic antifungal drugs topically in the form of ointment (cream) - miconazole or clotrimazole 2 times a day for 2 weeks, as well as ketoconazole 4 times a day for 2 weeks (within 1 week after recovery - to prevent relapse). Econazole and methylnaphthalene derivatives, for example naftifine, are also prescribed • For dermatophytosis of the scalp - griseofulvin 1 g/day (for children - 16 mg/kg, for microsporia - 22 mg/kg) orally daily until the first negative test for fungi, then the same dose for 2 weeks every other day and 2 weeks 2 times a week or ketoconazole. Terbinafine 125-250 mg/day for 4-6 weeks. Locally - 2-5% iodine solution, ointment with sulfur (10%) and salicylic acid (3-5%) • For onychomycosis - terbinafine 250 mg/day for 2-4 months, itraconazole 200 mg/day for within 3 months
Synonyms • Dermatophytosis • Athlete's foot • Ring ring
ICD-10 • B35 Dermatophytosis • B36 Other superficial mycoses
APPLICATIONS
Geotrichosis is a systemic mycosis caused by the yeast-like fungus Geotrichum candidum, affecting the oral cavity, bronchi, lungs or intestines. Symptoms: cough with mucopurulent viscous sputum (streaked with blood), aphthous stomatitis, fever. Secondary or mixed infection is possible. The prognosis is unfavorable. Treatment • gentian violet • oral potassium iodide for lung damage. ICD-10. B48.3 Geotrichosis.
Chromomycosis is a systemic fungal disease caused by certain dark hyphal fungi (Fonsecaea pedrosoi, Fonsecaea compacta or Phialophora verrucosa), with predominantly rough and deforming skin changes. Characterized by slow transformation into large and often ulcerating papillomatous growths (in the form of cauliflower). It usually occurs chronically. Observed everywhere; most often in tropical and subtropical countries (Brazil, Costa Rica). Treatment: the success of treatment is inversely related to the duration of the disease and the activity of the process; antifungals (amphotericin B, ketoconazole), antihelminthics (thiabendazole). Synonyms: verrucous dermatitis, Pedroso disease, chromophytosis, chromoblastomycosis. ICD-10. B43 Chromomycosis and pheomycotic abscess.
Erythrasma is a pseudomycosis caused by the bacterium Corynebacterium minutissimum, manifested by limited foci of yellowish-brown or pink color with clear contours and fine pityriasis-like peeling on the surface; localized almost exclusively on the areas of the inner thighs adjacent to the scrotum.
At-risk groups
Men are more susceptible to dermatophytosis inguinalis than women. The following also increase the risk of infection:
- history of fungal infections;
- weakened immunity;
- disruption of the endocrine and digestive systems;
- stressful conditions;
- climatic conditions (high humidity and air temperature);
- close-fitting clothing;
- presence of chronic diseases;
- increased sweating (hyperhidrosis);
- frequent visits to public baths and saunas;
- obesity;
- genetic predisposition.
Diagnostics
For diagnosis, the patient’s medical history and symptoms are studied, and a number of studies are carried out:
- CON test. Belongs to the group of microscopic studies. Before microscopy, the affected area is treated with a 10% potassium solution or 25% sodium hydroxide solution to clear the preparation. The test identifies the spores or mycelium of the fungus. The method accurately confirms the diagnosis, but has low sensitivity and may show a false negative result.
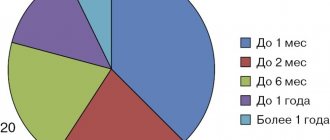
- Culture method. The material is planted on a nutrient medium. Based on the results of the analysis, the type of pathogen and its susceptibility to drugs are determined. Microscopy of the culture is performed. They make a diagnosis. The disadvantage of the method is the long duration of the study (up to 7 weeks).
- Direct DNA diagnosis of dermatophytosis. This is a new method using polymerase chain reaction. The analysis requires specialized laboratory equipment.
- Histological examination of the skin by taking a biopsy. Used in difficult to diagnose cases.
- Wood's lamp examination. Used when it is necessary to distinguish dermatophytosis from erythrasma. When examining erythrasma, the lesions have a pinkish glow.
List of sources
- Sergeev A. Yu., Sergeev Yu. V. Fungal infections (a guide for doctors). M., 2003. 185–193.
- Leshchenko V. M. Fungal skin diseases. In the book: Skin and venereal diseases (a guide for doctors). Ed. Yu. K. Skripkina, V. N. Mordovtseva. M., 1999. T. 1. P. 257–311.
- Sergeev V.Yu., Sergeev A.Yu. Dermatophytes: new in the diagnosis, therapy and prevention of the most common human mycoses. Consilium medicum. – Dermatology. – 2008. – No. 1. – P. 30–35.
- Haldin A.A., Sergeev V.Yu., Izyumova I.M. Modern ideas about inguinal dermatophytosis: etiology, epidemiology, clinical picture and effective therapy. Ross.zhur. leather and veins Bol. – 2005. – No. 5. – S. 43–48.
Treatment
The goal of treatment for inguinal dermatophytosis is to remove the pathogenic fungus. Therapy should be comprehensive and include etiotropic, pathogenetic, and symptomatic treatment.
Etiotropic treatment consists of taking fungistatic and fungicidal drugs. They suppress the activity of fungi and destroy them. Pathogenetic treatment eliminates the factors leading to the development of the disease or arising during it. Symptomatic therapy eliminates other subjective and objective symptoms of the disease.
If patients experience acute inflammation, lotions, pastes or ointments are prescribed. Itching with dermatophytosis is relieved with sedatives and antihistamines.
Infection with dermatomycosis
This infectious disease is quite common. If you identify and begin to eliminate the disease in a timely manner, and follow all the doctor’s recommendations, then such effective therapy will give positive results. However, it may also happen that when the disease is advanced, its chronic form develops.
Infection with dermatomycosis occurs through direct contact with a sick person, or through contaminated objects. Such objects may include towels, shoes, and carpets. Some types of fungus live on damp surfaces, such as the floor of a locker room, bathhouse, or shower. The fungus can be contracted from pets suffering from ringworm (ringworm).
The causative agent of the disease is a fungus of the genera Microsporum, Trichophyton, Achorion.
Prevention
In order to prevent inguinal dermatophytosis, you should adhere to the following rules:
- promptly treat fungal diseases;
- monitor your health and weight, strengthen your immune system;
- do not use other people’s personal hygiene items;
- use personal slippers and towels in swimming pools and saunas;
- fight hyperhidrosis;
- wear loose-fitting clothes, especially in the hot season;
- after taking a shower, thoroughly dry the groin area with a towel;
- If symptoms are detected, contact a specialist.
Forecast
Despite the fact that epidermophytosis is characterized by a long course and a tendency to recur, the prognosis is usually relatively favorable. If treatment is prescribed correctly, recovery occurs. At the same time, it is important to carefully observe the timing of treatment, observe the rules of personal hygiene and eliminate all risk factors, including adjusting sugar levels in diabetes mellitus .
Athlete's foot is characterized by a more persistent course, but with proper and long-term treatment, the prognosis for recovery is also favorable. When bacterial infections are associated, the prognosis of the disease is more serious. Onychomycosis can be treated, but it must be long-term and use systemic drugs. The effect in the treatment of onychomycosis depends not only on the prevalence of the process, the form of nail damage and the correct choice of means, but also on the disinfection of shoes until a healthy nail grows back.
Frequently asked questions about dermatophytosis inguinalis
How dangerous is dermatophytosis inguinalis?
If not treated promptly, dermatophytosis inguinalis can lead to the formation of lichenification. This is a thickening of the skin and a violation of pigmentation due to scratching due to severe itching. It is also possible that a secondary infection may occur, erosions, ulcers, and ulcers appear, and pain increases.
How long does it take to treat dermatophytosis inguinalis?
On average, the duration of treatment for inguinal dermatophytosis is 4–6 weeks.
Which doctor treats dermatophytosis inguinalis?
A dermatologist deals with diseases of the skin. Sometimes, for more effective treatment, a dermatologist refers patients to a mycologist and trichologist.
Consequences and complications
When athlete's foot complications are considered:
- Transition from one form to another.
- Onychomycosis.
- The addition of a bacterial infection is secondary pyoderma , lymphangitis , lymphadenitis and recurrent erysipelas, resistant to antibiotic treatment. Against the background of such lesions, thrombophlebitis , lymphostasis and elephantiasis occur .
- Allergization of the body: urticaria , bronchial asthma , allergic rhinitis , the occurrence of mycids . These are secondary allergic rashes due to mycoses.
For inguinal athlete's foot:
- Mycotic eczema . It occurs in a chronic form, manifested by lichenification of the skin (thickening), which occurs from scratching. The process resembles neurodermatitis.
- Allergic dermatitis.
- Impetiginization is the development of impetigo as a complication of mycosis. Impetigo is a strepto-staphylococcal skin lesion.