Forms and complications of atopic dermatitis
Depending on your age, atopic dermatitis rashes may look different. There are infant, child and adult forms of the disease. In addition, there are currently two forms of atopic dermatitis depending on the presence of atopy - atopic and non-atopic.
In the atopic form, there is a connection between exacerbations with food, house dust allergens, and less often pollen. Other atopic diseases are often present: bronchial asthma, allergic rhinitis - both in the patient himself and in his close relatives.
It is assumed that there are other forms of atopic dermatitis, since in different patients the disease may have a different set of symptoms and proceed differently. However, clear markers that allow us to judge which scenario the disease will develop in a particular case have not yet been identified.
Atopic dermatitis can be complicated by the addition of an infection - bacterial, fungal or viral. If the pattern of rashes has changed, or you are concerned about your general condition (fever, lethargy, headache, etc.), you should consult a doctor.
Drug therapy
System
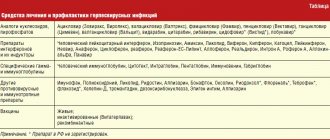
For general therapy (oral administration), depending on the skin disease, the following may be used:
- Anti-infectives: antibiotics, antiviral and antifungal drugs.
- Anti-inflammatory drugs: hormonal (glucocorticosteroids), antihistamines and calcium supplements.
- Vitamins.
Local or external
For external therapy, various dosage forms are used, such as ointments and creams for dermatitis, lotions, powders, talkers, aerosols, shampoos and gels.
Since the product for external therapy comes into direct contact with the affected skin, modern medicine places increased demands on it. It should:
- have anti-inflammatory and skin soothing effects;
- relieve swelling and itching;
- destroy foci of infections (have antimicrobial and antifungal effects);
- soften dry areas of the skin and dry out wet rashes;
- be safe and suitable for children.
External therapy agents can be divided into two large groups:
- ointments and creams based on hormones (glucocorticosteroids);
- non-hormonal drugs.
Causes of the disease
There is no single cause for the development of atopic dermatitis. The occurrence of the disease is facilitated by a whole complex of conditions: genetic characteristics and environmental factors. These include a violation of the protective function of the skin (it becomes more vulnerable to the effects of detergents or other irritating factors), characteristics of the immune system, climatic conditions (temperature, humidity, dust, tobacco smoke and other impurities in the external environment). Possible effects of the microbiome are being studied.
Local glucocorticosteroids
Glucocorticosteroids have high anti-inflammatory activity, but at the same time they have a wide list of side effects:
- development of skin atrophy;
- the appearance of stretch marks, acne;
- suppression of normal skin flora and risk of secondary infection;
- depigmentation.
In addition, hormonal drugs can cause the so-called “withdrawal syndrome,” in which the patient’s skin condition quickly deteriorates after completion of the course of treatment.
In young children, external hormonal preparations are usually prescribed in cases of severe forms of skin lesions and not on all areas of the skin.
Treatment of atopic dermatitis
A feature of the treatment of atopic dermatitis is a stepwise approach from simpler methods of external therapy and skin care to complex innovative techniques.
Remedies and methods for treating atopic dermatitis
When treating atopic dermatitis, the following are used:
- Softening and moisturizing creams and ointments are the basis for the treatment of atopic dermatitis. These products help keep your skin hydrated and soft.
- Steroid creams and ointments are applied to the skin and help relieve redness and itching. In severe cases, steroid tablets or injections may be required, but your doctor will keep the course of treatment as short as possible, since the high effectiveness of injections comes with a high risk of side effects.
- Medicines that affect the immune system are highly effective, but have side effects and may be prescribed when safer treatments do not produce the desired results.
- Antihistamines may be used in patients who report decreased itching.
- To increase the effectiveness of therapy, it is possible to perform wet wraps (Wet Dressing, Wet Wrap Therapy).
Wet wraps (Wet Dressing, Wet Wrap Therapy)
Treatment with Wet Wrap Therapy helps to quickly clear skin of rashes and can be used both in a medical facility or hospital, as well as at home. The effect is associated with improved penetration of the drug used, deeper and longer-lasting hydration, and reduced water loss by the skin. The dressings provide protection from scratching, which leads to the formation of an itch-scratch cycle, preventing scratches from occurring, which further intensify the itching, which makes the skin heal better. Cooling the surface of inflamed skin by evaporating water from the dressings helps reduce inflammation, itching and soreness.
For severe eczema, wet wraps are prescribed in a medical facility. They can also be used at home to maintain good health or at the first sign of deterioration and can reduce the need to seek medical help and the likelihood of hospitalization.
There are various modifications of Wet Wrap Therapy; the essence of the method is to use external medications (emollients or steroids) under two layers of bandages. The bottom layer is warm and moist, on top of which a second, dry layer is made. For the bandage, you can use a regular bandage, special tubular bandages, or special clothing. The bottom layer must be periodically moistened with ordinary warm water, preventing it from drying out. The use of topical steroids under a wet dressing can increase the effectiveness of treatment. The procedure can be performed 1-2 times a day, every day, during an exacerbation. As the exacerbation decreases, the procedure can be done less frequently, performed 1-2 times a week during the period of remission. If well tolerated, the bandage with the medicine can be left overnight, remembering to periodically moisten the bottom layer of tissue.
The procedure takes quite a long time, and in the first stages (especially in patients with severe skin damage) may require the participation of medical personnel. After training and improvement, the procedures can be continued at home.
Medicine knows about 2,000 different skin diseases, which are united by a common medical term - dermatoses.
Among them, psoriasis and atopic dermatitis are the most common. The head of the clinic of dermatovenerology and allergology-immunology of the European Medical Center, candidate of medical sciences, doctor of the highest category Eva Pechatnikova and you understand these common skin diseases and find out the most effective treatment methods phototherapy of the European Medical Center Dmitry Serov.
Atopic dermatitis and psoriasis: more similarities or differences?
Despite the fact that psoriasis and atopic dermatitis belong to the same group of diseases (dermatosis), they are completely different skin problems. Atopic dermatitis belongs to a group of allergic diseases, usually hereditary. Polypous rhinosinusitis, bronchial asthma, hay fever (pollen allergy) are all diseases similar to atopic dermatitis. Psoriasis has a completely different pathogenesis, which often causes inflammatory processes in the joints, kidneys and other organs and tissues. Thus, these skin problems have different clinical presentations. Moreover, they can be combined, that is, one patient can have both atopic dermatitis and psoriasis.
The only thing that is similar between these diseases is the prominent role of cytokines.
Cytokines are pro-inflammatory proteins that are secreted by immune cells (T-lymphocytes, B-lymphocytes, monocytes, macrophages, etc.). There are several groups of these protein formations, but the common property of all cytokines is their influence on immune cells, stimulating their development and transmitting information from cell to cell. In other words, cytokines are regulators of the body's immune responses. In the event of a violation of coordination of actions between immune cells, cytokines provoke processes that intensify rashes in both atopic dermatitis and psoriasis.
How do atopic dermatitis and psoriasis manifest?
Psoriasis affects about 3-7% of the world's population. This disease has no age limit, but is most often diagnosed in patients 29-36 years old. Typically, psoriasis appears as pink, scaly patches on the elbows and knees and on the scalp. Sometimes defects appear on the nails. In advanced forms of the disease, the entire body may be covered in pink, itchy plaques.
The main manifestations of atopic dermatitis (or neurodermatitis) are skin rashes, most often in areas of large folds, face and neck. The main distinguishing symptom of this disease is itching. As a rule, neurodermatitis manifests itself in childhood, and then becomes chronic and accompanies a person throughout his life.
How dangerous are these diseases?
If dermatosis is not detected in time, it often leads to complications. Advanced forms of psoriasis are dangerous for the development of psoriatic arthritis, that is, damage to the joints. In this case, complex treatment requires the help of not only a dermatologist, but also a rheumatologist.
Exacerbation of atopic dermatitis provokes inflammation of the lymph nodes (in the cervical, axillary, inguinal, femoral areas), ophthalmological abnormalities (recurrent conjunctivitis and ectropion, that is, eversion of the eyelid). In addition, there is confirmed medical evidence that patients with atopic dermatitis are more likely to suffer from herpes simplex virus and HPV. Often, bacterial and fungal infections develop in parallel with atopic dermatitis.
Causes of psoriasis and atopic dermatitis
The main and proven cause of both atopic dermatitis and psoriasis is genetic predisposition. For example, if one of the parents is a carrier of atopic dermatitis, then with a 50% chance the disease will be passed on to the child. If the carrier is the mother, then this probability increases.
Regarding psoriasis, we can say that this skin disease is not fungal, that is, it cannot be infected through household contact. Psoriasis can develop under the influence of stress, infectious diseases and trauma.
How is the disease diagnosed?
There are a number of tests that are always performed when you first visit your doctor. If necessary, the diagnosis is established using histological examination. But in most cases, a general clinical picture is enough to make a conclusion.
Traditional and modern treatments
When treating skin diseases, the doctor is guided by the rule of the so-called therapeutic ladder. The specialist begins by prescribing the simplest treatment methods. If such practices are ineffective, the doctor moves to the next stage of treatment, where systemic and biological therapy drugs can be used. Thus, the first stage is standard methods, the second is physiotherapeutic techniques, the third is systemic, and then biological therapy.
Laser therapy, ultrasound, magnetic therapy, and phototherapy are used as physiotherapeutic treatments. This type of treatment is very effective. However, it is worth noting that physiotherapy is not used in the acute phase of skin diseases. During periods of severe inflammation, treatment procedures can aggravate the situation and provoke the appearance of new lesions.
One of the ways to alleviate the manifestations of psoriasis is plasmapheresis - a procedure for cleansing the blood of toxins, poisons, salts and other harmful substances. It is important for people with psoriasis to watch their diet, eat a low-calorie diet, and avoid fried foods and alcohol. Psychotherapeutic sessions with a specialist are also a necessary element of treatment. The specialist helps the patient understand what disturbances in the psycho-emotional state could cause psoriasis, and in the future they work together on the optimal ways to respond to the triggers.
Of course, drug therapy is also used to treat skin diseases. Often, patient treatment is supplemented by the prescription of antihistamines, antibacterial, antiviral, and antimycotic agents. To restore damaged skin, emollients and moisturizers with a predominance of ceramides, lipid components of the cell membrane, are used. For mild cases of the disease, doctors recommend taking calcineurin inhibitors, that is, non-steroidal immunomodulators. In case of severe manifestations of atopic dermatitis, cyclosporine is prescribed. This remedy is very effective, but it cannot be abused over a long period of time (more than 1-2 years). This is due to the toxicity of some substances included in its composition.
To maintain a state of remission in patients, experts recommend, first of all, special skin care. To do this, every time after taking a shower, it is necessary to apply emollients to the skin - products whose composition is completely identical to the composition of the lipid mantle of our skin.
The above methods are used to treat both psoriasis and atopic dermatitis. The specific method of therapy for each patient is selected by the doctor based on the overall clinical picture. It is worth noting that in the treatment process, an important point is close interaction between doctors: dermatologists, allergists, rheumatologists. It is teamwork that allows us to achieve guaranteed positive results from the therapy.
Biological therapy - a revolution in the treatment of atopic dermatitis and psoriasis
Biological therapy completely changes the paradigm of treatment of skin diseases and helps to achieve sustainable remission.
The essence of this modern therapy is that it affects cytokines, that is, information molecules that cause the development of psoriasis and atopic dermatitis. It is biological drugs that make it possible to “freeze” the development of the disease. Previously, such medicines could only be found abroad, but now they are available in Russia.
A few years ago, getting rid of 50% of all skin rashes was considered an excellent result. Now, with the help of biological therapy, doctors are able to clear the patient’s skin almost 100%. At the moment, there is no type of psoriasis and atopic dermatitis for specialists that they cannot cope with.
As a result of treatment, the patient forgets about the existence of his illness. Unlike other types of systemic therapy, drugs consisting of large protein molecules do not have harmful effects on internal organs. Therefore, they can be appointed on a permanent basis.
The principle of action of biological drugs can be illustrated by the example of dupilumab, a drug based on monoclonal antibodies. This biological drug blocks inflammatory processes caused by cytokines. Thus, treatment with dupiluamab reduces the concentration of biomarkers in the blood that provoke a severe course of the skin disease. Such biological therapy is effective due to its selectivity and helps where all other methods have failed. Contraindications to the use of drugs obtained by innovative genetic engineering methods depend on the patient’s individual tolerance to certain substances.
Quality of life of patients after treatment
Even with severe forms of psoriasis and atopic dermatitis, doctors restore quality of life to patients. Those who could not attend work due to joint disease and significant skin damage can now live an absolutely normal life, have a family, children, etc. Some patients could not leave the house, were forced to leave work, fell into deep depression, and did not see any prospects for a complete cure. And it was biological therapy that was able to help them start a new life without discomfort.
Clinical signs
Throughout the childhood period, the clinical picture of dermatitis in children can change many times, not only regarding the type of rash itself, but also regarding the location of the lesions.
Signs of the infant form
They manifest themselves as the formation of red spots, skin swelling, and blistering rash. The opening of the bubbles forms pockets of weeping, which, when dry, become covered with yellow-brown crusts. The skin of the cheeks, forehead, scalp, buttocks and extensor joint surfaces is affected. The whole process is accompanied by severe itching, disturbing the child’s peace of mind.
At the initial stage of the disease, only the superficial layer of the skin is exposed to allergic inflammation. With timely elimination of the causative factor, the allergic process is easily amenable to involution. An attempt to stop the inflammatory reaction with medications or local preparations (creams, ointments) will not yield results. If the provoking allergen is not removed, the initial stage of atopic dermatitis will enter the phase of pronounced changes.
Manifestations of the child form
Vivid symptoms appear during periods of exacerbation. The localization of pathological foci is noted mainly in the folds of the skin in the area of flexion of the elbows, knees, feet, hands, on the neck and in the area behind the ears. The skin becomes dehydrated, peels off, and a pronounced, clear skin pattern appears (lichenification). The child’s face changes – the skin is dull, there is pronounced pigmentation around the eyes, and an additional fold of skin appears on the lower eyelid.
Even in the absence of exacerbation, intense itching is noted. The skin of the fingers and hands cracks due to severe dryness.
Symptoms of adolescent atopic dermatitis
They manifest themselves as widespread and permanent lesions of the skin. Localization of the pathological process - back, chest, face, neck, joint extension area.
Characterized by lichenification and dry skin, scratch marks, cracks on the feet and hands.
Diagnosis and treatment of dermatitis in a child
Any rash on the skin of children requires a professional assessment by a pediatric dermatologist, pediatrician or allergist-immunologist (sometimes an infectious disease specialist). To confirm the likelihood of children developing dermatitis, the doctor conducts a thorough examination of the skin, a detailed medical history, and prescribes a series of clinical and laboratory examinations.
When diagnosing allergic dermatitis, it is important to identify signs of eosinophilia in the blood plasma, increase the concentration of total and allergen-specific immunoglobulin E and G, using various allergy diagnostic methods (MAST, RAST, ELISA or RIST), skin and provocative tests.
Laboratory tests include:
- bacteriological analysis of smears for suspected secondary infection;
- examination of scrapings from a smooth area of skin to identify the pathogen;
- coprogram - to identify helminths and dysbacteriosis.
If necessary, an ultrasound examination of the peritoneal organs or a skin biopsy may be prescribed for a differential diagnosis.
During the diagnostic search, the form and cause of the development of dermatitis in a child are clarified, the presence of immunodeficiency and other skin pathologies, such as lymphoma, psoriasis, ichthyosis, scabies, microbial eczema, and pityriasis rosea is excluded or confirmed.
Allergic dermatitis
This is a disease caused by the presence of inflammatory processes on the child’s skin when it interacts exclusively with one specific, provoking irritant - an allergen. This reaction is usually called delayed, which is associated with a rather long period of its development - the first signs of the disease may appear only two weeks after contact with the allergen.
The speed of the immune response depends on how quickly a specific allergen is able to contact the amino acid composition of proteins contained in the skin and form an antigen. In response to the penetration of a foreign component into the body, macrophages form a standard immune response, which is manifested by the creation of a protective barrier in the form of an inflammatory reaction. Immune phagocytic (protective) cells (T-lymphocytes) remember the “intruder” and when it reappears, the inflammatory reaction resumes.
The cause of the development of allergic dermatitis in children can be both internal and external allergenic factors. Internal allergens include those allergens that a child takes orally with food or liquid (including medications), or inhales.
External factors include those allergens that directly affect the skin:
- Chemical exposure – dyes in children’s clothing and washing powders, hygiene products, food additives, flavorings and stabilizers, acrylic toys.
- Physical impact - cold or heat.
- Biological effects – fungal, bacterial or viral pathogens.
Allergic dermatitis can occur in children of any age - from two months to the end of puberty.