Pityriasis versicolor in humans: symptoms and treatment with ointments
Pityriasis versicolor (colored, multi-colored lichen) is a recurrent skin disease of a fungal nature, which affects only the outer layer of the skin (the upper stratum corneum of the epidermis), which has direct contact with the environment. Doctors note that the peak of the disease occurs in the hot summer, which is why this disease is often called “sun fungus.” Mostly young people suffer from pityriasis versicolor; it is much less common in children and the elderly.
The causative agent of tinea versicolor in humans is yeast-like fungi of the genus Pityrosporum, which can exist in three different forms, transforming into one another. The disease is considered conditionally contagious, that is, the fungus can be transmitted through contact with a sick person and his personal belongings, but this does not mean that the infected person will necessarily get sick.
What it is?
Pityriasis versicolor is a long-term (chronic) fungal infection of the stratum corneum of the epidermis. A common (slang) name that can be found at resorts is “solar fungus.” It is necessary to distinguish the disease from Vitiligo, pink zhibert and syphilitic roseola.
The name “lichen” (Lichen) has been known since the time of Hippocrates; it includes many skin diseases, which are characterized by the formation of colored spots and peeling. The causative agent of pityriasis versicolor was described by G. Robin in 1853, and in 1951 M. Gordon identified round and oval forms of the pathogen, both in places of pityriasis versicolor rashes and within healthy skin, classifying it as a yeast-like fungus.
Causes of infection
The causative agent of the disease is a yeast-like fungus, known in 3 forms: round Pityrosporum orbiculare, oval Pityrosporum ovale and mycelial Malassezia furfur, which can take different shapes.
It lives on human skin constantly, but is activated only under the influence of certain factors:
- violation of hygiene rules;
- for diabetes mellitus;
- profuse sweating - both during heat and during certain diseases, tuberculosis, for example;
- in case of disturbances in the functioning of the endocrine system and some diseases of the gastrointestinal tract, the opportunity for the fungus to “prove itself” appears due to changes in the acidity of the skin;
- immunodeficiency - both due to illness or general weakening, and as a result of taking certain medications: cytostatics, glucocorticoid hormones.
Until recently, it was believed that it was very difficult to catch pityriasis versicolor from a sick person, however, recent research in this area refutes the early conclusions of scientists. Nowadays, dermatologists are inclined to believe that pityriasis versicolor can appear not only after personal contact with an infected person, but also when sharing household items (bed linen, towels, washcloths, clothes).
Thus, it is quite possible to pick up a fungus even in the fitting room of a clothing store. The first symptoms of pityriasis versicolor appear within a period of several weeks to several months. The duration of the incubation period depends on the state of human health and the presence of provoking factors, which we already wrote about just above.
Pityriasis versicolor (tinea versicolor): symptoms
The disease is characterized by the following symptoms:
- the appearance of spots of different shapes, sizes (usually with uneven edges) and colors (white, red, brown, etc.);
- the spots become scaly and may sometimes itch;
- under the influence of the sun, spots can change color and intensity;
- as the disease progresses, the spots increase and unite into large groups;
- Sometimes, if the source of the spot is the scalp, the hair may fall out.
Localization of spots is the chest, back, groin area, arms, legs, less often the face, scalp and genitals. The incubation period ranges from two weeks to several months; in children, the first signs may appear earlier.
Pityriasis versicolor (colored, multi-colored or solar) lichen: causes of occurrence
The main cause of the disease is a fungus that gets on human skin. But there may be several factors that can provoke the active proliferation of this fungus and the appearance of such characteristic symptoms of pityriasis versicolor as multi-colored spots:
- individual (genetic) predisposition to dermatomycosis;
- skin type and/or disruption of the normal functioning of the stratum corneum;
- the presence of concomitant diseases of the endocrine system;
- diabetes mellitus, excess weight, vegetoneurosis;
- increased sweating;
- reduced immunity;
- chronic diseases;
- vegetative-vascular dystonia;
- diseases of the gastrointestinal tract, as well as liver and pancreas;
- respiratory diseases;
- severe stress and constant nervous tension;
- frequent changes in climate and time zones;
- uncontrolled use of medications and cosmetics that are unsuitable for your skin type;
- disturbances of hormonal levels and the functioning of the genitourinary system in women.
The reasons may also be external factors: hot weather or the use of antibacterial personal hygiene products (gels, creams, etc.). But, whatever the cause and no matter how the disease develops, if there are signs of any intensity, you should consult a doctor.
When contracting any skin disease, it is very important to treat not the symptoms, but the causes, while simultaneously getting rid of the existing factors that provoke the disease. This type of lichen may not go away for a long time, and accordingly, treatment may take a long time.
How to treat solar lichen (colored, pityriasis versicolor, multi-colored) and cure it, securing the result for a long time, dermatologists
medical
Modern diagnostic methods make it possible to get rid of the disease and prevent its relapses. An individual course is selected for each patient and maximum attention is paid during treatment to ensure comfort in the fight against an unpleasant disease.
Initial appointment
The initial appointment is an examination, studying tests and complaints to identify the causes that led to infection, as well as drawing up a general clinical picture. In some cases, already at the first consultation, the doctor can prescribe treatment and recommend a course of restorative procedures.
But if the case has any deviations or complications, then it is necessary to prescribe additional studies and consultations with other specialists.
Diagnostics includes:
- skin scraping examination;
- examination of the skin using a Wood's lamp;
- consultations and examinations with specialists such as a gastroenterologist
,
gastroenterologist
and psychotherapist; - examination of the skin using an iodine test.
What exactly the doctor will prescribe and whether any additional research will be needed depends solely on each specific case, as well as the selected methods and drugs for the treatment of pityriasis versicolor (tinea versicolor, solar lichen) in an adult or in children.
Treatment plan
If a course of treatment was prescribed at the patient’s first meeting with the doctor, then at the secondary appointment the doctor assesses the patient’s condition and the effectiveness of the prescribed regimen.
If the selected regimen and drugs for the treatment of pityriasis versicolor (variegated, colored) lichen do not work, then the doctor can either prescribe an additional examination or adjust the previously prescribed course. The doctor also draws up a treatment plan with an individual schedule for subsequent visits.
What can be included in the course of treatment?
Most often, the doctor prescribes:
- antifungal drugs;
- antifungal ointments and gels;
- special shampoos if lesions are found on the scalp;
- antibiotics from the tetracycline group for severe forms;
- topical products with exfoliating and anti-inflammatory effects.
During treatment, it is very important to strictly follow all the doctor’s instructions (take medications on schedule and in the right quantity, follow established rules, etc.), but remember that any deterioration or abnormal reaction of the body must be reported to the doctor so that he can adjust treatment.
Control reception
A follow-up visit to the attending physician's office is scheduled 21–30 days after the start of treatment. This is necessary to assess the patient’s condition after the main course and prescribe a number of restorative and preventive measures. Such measures may include physical therapy, restoration of gastrointestinal microflora, nutritional correction, etc.
Treatment result
The disease can be cured, but the timing of treatment and recovery is individual and is discussed at a doctor’s appointment. Also, if necessary, the doctor prescribes consultations and examinations for all family members, since infections could have occurred through personal hygiene items.
Prevention
A good prevention of this skin disease is:
- observing simple hygiene rules in public places (swimming pools, gyms, etc.);
- maintaining personal hygiene. Personal hygiene items can and should not only be changed frequently, but also constantly disinfected;
- ironing clothes after washing and before wearing (especially for children's underwear and clothes);
- wearing and using clothing and personal hygiene items only from natural materials of good quality;
- temporary avoidance of prolonged exposure to the sun;
- nutrition correction;
- hardening and dousing with acidified water;
- taking vitamins or vitamin complexes;
- compliance with sanitary standards in the apartment and in the workplace;
- individual selection of cosmetic skin care products;
- normal healthy sleep;
- a properly selected system of physical activity and sports to strengthen the immune system and increase the body’s resistance to external influences.
It is also important to exclude all causes that have led or may lead to a recurrence of pityriasis versicolor (colored, multicolored, solar) lichen. Compliance with minimum standards and taking care of your health will significantly reduce the risk of the return of this unpleasant skin disease, and will also bring your psychological state back to normal.
If the disease returns even after treatment and all the measures taken, then it’s time to think about a serious examination by a group of specialists, since inflammation of the skin may be a consequence of diseases that did not manifest themselves in any way before.
To make an appointment for a consultation or appointment with one of the medical dermatologists, you can use a special online form on the website or the phone number listed at the top of this page.
Symptoms in humans
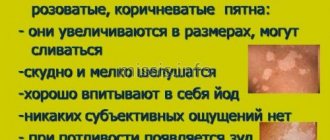
Typical symptoms of pityriasis versicolor in humans are (see photo):
- The appearance of pink spots with a yellowish color;
- A gradual change in their color to brown pigmentation, localized in typical places (primarily the décolleté area);
- Slight fine-plate peeling of rashes that appear on the skin;
- Intermittent itching of the spots, which is not very intense;
- The skin does not tan in the place where the rash is localized. This is explained by the functional inferiority of melanocytes - skin cells that produce pigment.
To determine if you actually have sunburn, visit a dermatologist. The doctor will check your skin with a lamp - the fungus has luminescent properties. If the skin glows pink or greenish-blue, a dermatologist will diagnose lichen.
In humans, the symptoms of pityriasis versicolor, in the form of itching and burning, are often not expressed. If the doctor suspects the presence of a fungal pathogen, he will send the patient for analysis of keratinized skin flakes.
Diagnostics
For an experienced dermatologist, an external examination of the patient is enough to suspect he has lichen colorus.
However, to clarify the diagnosis, a number of tests will be required, including:
- Microscopic examination of skin scrapings from spots. Under a microscope, the doctor examines the dermal scales, which are pre-treated with a 20% KOH solution. The fungi that cause tinea versicolor will be represented by long filaments with rounded growths located on them.
- Test using iodine. During the study, the skin is treated with a 5% iodine solution. After a few minutes, the tinea versicolor spots turn dark brown.
- Using a Wood's lamp for diagnostics. In the light of its rays, the spots acquire a reddish-yellow tint or a greenish-golden color.
- Check for Beignet's sign , in which skin particles flake off easily, even with minor scraping.
This is a complete list of diagnostic methods that allow you to identify tinea versicolor. In practice, doctors most often use only the iodine test and Wood's Lama.
What pityriasis versicolor looks like, photo
The photo below shows how the disease manifests itself in humans.
The areas of the skin affected by the disease are not exposed to sunlight (do not tan), and in the summer they look lighter than healthy skin. The spots can be located on the human body separately from each other, or they can merge. Peeling of the skin is observed, which is due to the fact that the activity of the fungus leads to loosening of the stratum corneum of the skin.
Prevention
To prevent relapses, you need to treat chronic diseases, maintain immunity at the proper level, harden yourself, and eat well. Wear clothes made from natural fabrics that do not restrict movement.
Do not wear other people's clothes, do not use other people's objects. On particularly hot days, wipe the skin with water with the addition of alcohol or lemon. Maintain cleanliness and order.
Take antifungal medications once monthly. Although the lesion is not accompanied by painful sensations, it spoils the appearance and causes inconvenience.
Ringworm on the arm - 115 photos of what lichen looks like and video recommendations from dermatologists for treating the diseaseRingworm - symptoms, development, types, tips on how to quickly and effectively cure at home (105 photos and videos)
Lichen planus - first symptoms, causes, information about the disease and effective treatment (100 photos)
Treatment of pityriasis versicolor with ointments and medications
At home, ointment and other external remedies (creams, lotions, powders, solutions, sprays, etc.) are used for pityriasis versicolor.
The following external antifungal agents are currently used:
- Products with naftifine (Mycoderil, Exoderil);
- Products containing sertaconazole (Zalain, Sertaconazole, Sertaconazole);
- Products with isoconazole (Travogen and Travocort);
- Products containing econazole (Ifenek, Ecodax);
- Products containing miconazole (Daktarin, Mikozon);
- Products with ketoconazole (Dermazol, Mycozoral, Mycoket, Nizoral, Perhotal, Sebozol);
- Products with bifonazole (Bifasam, Bifonazol, Bifosin, Mikospor);
- Products with clotrimazole (Amiclon, Imidil, Candibene, Candide, Candizol, Kanesten, Kanizon, Clotrimazole, Funginal, Fungicip);
- Products with terbinafine (Atifin, Binafin, Lamisil, Lamisil Dermgel, Lamisil Uno, Lamitel, Mikonorm, Tebikur, Terbized-Agio, Terbizil, Terbix, Terbinafine, Terbinox, Terbifin, Termicon, Ungusan, Fungoterbin, Exiter, Exifin).
Pityriasis versicolor tablets. The following oral antifungal medications are used to treat severe cases of pityriasis versicolor:
- Fluconazole (Diflazon, Difluzol, Diflucan, Disorel-Sanovel, Medoflucon, Mikomax, Mikosist, Mikoflucan, Nofung, Procanazol, Fangiflu, Fluzol, Flucoside, Fluconazole, Fluconorm, Flunol, Flucostat, Forkan, Funzol, Ciskan). The drugs are taken either 200 mg once a day for 1 - 2 weeks, or 400 mg once a week (a total of two doses with an interval of 7 days between them).
- Ketoconazole (Ketoconazole, Mycozoral, Nizoral, Oronazole, Funginok, Fungistab, Fungavis). The drugs are taken either 200 mg once a day for 1 - 2 weeks, or 400 mg once a week (a total of two doses with an interval of 7 days between them).
- Itraconazole (Irunin, Itrazol, Itraconazole, Canditral, Miconihol, Orungal, Orungamin, Orunit, Rumikoz, Teknazol). The drugs are taken 200 mg 2 times a day on the first day, then for 5 days 200 mg once a day.
The following external agents are used as keratolytics:
- Salicylic-resorcinol alcohol;
- Salicylic ointment 5%;
- Salicylic alcohol (salicylic acid) 3 – 5%;
- Resorcinol alcohol 5 – 10%;
- Glycolic acid 5 – 10%.
Shampoo and other cosmetics for pityriasis versicolor. Currently, for the treatment of pityriasis versicolor on the scalp, shampoos containing the following components that have an antifungal effect are used:
- Zinc pyrithione (Keto-plus shampoo; Skin-cap aerosol, shampoo and cream; Zinocap aerosol, cream);
- Selenium sulfide (Sulsen Mite paste and shampoo; Sulsen Forte shampoo; Sulsen, lotion, oil and shampoo);
- Sodium thiosulfate (sodium thiosulfate solution);
- Ketoconazole (shampoo Keto-plus, Mycozoral, Mikanisal, Nizoral, Perhotal, Sebozol).
Folk remedies can also be used as a supplement:
- Brew a spoonful of peppermint in a glass of boiling water. Use to lubricate damaged areas after soaking in a water bath for a quarter of an hour;
- Mix celandine and St. John's wort (a spoonful) in a three-liter jar of boiling water. To brew, you need to add the ingredients to cheesecloth. Store the solution for a month. Take 50 mg three times a day. Store the medicine in the refrigerator;
- To lubricate pathological areas, you can use burdock oil, burdock juice, cranberry, calendula, and sea buckthorn. Both monocomponent and multicomponent solutions are used for processing.
Unfortunately, despite the relative safety of the disease, lichen versicolor is prone to recurrence, so in most people the infection reappears within 2 years after successful treatment. Relapses do not mean that the treatment was performed poorly, it’s just that a person most likely has a hereditary predisposition to the disease, as a result of which he develops an infection very quickly compared to others if conditions are favorable for it.
To prevent relapses of pityriasis versicolor, it is necessary to periodically (once a month) take one tablet of antifungal drugs.
Causes
Tinea versicolor is caused by the yeast Malassezia. It is found on the skin of more than 90% of adults, where it usually lives without causing any problems. Tinea versicolor may develop if this yeast begins to multiply more than usual. It is not yet clear to scientists why this happens in some people and not in others. It is believed that several factors may increase the risk of developing lichen versicolor, including:
- living or staying in a warm, humid environment
- excessive sweating (hyperhidrosis)
- creams, dressings or clothing that do not allow the skin to breathe
- weakened immune system.
Tinea versicolor is not associated with poor hygiene. The disease cannot be spread from person to person because most people already have Malassezia yeast on their skin.
Previous Next
How to prevent the disease?
In order to prevent relapses, local treatment is carried out during the warmest periods of the year. The scalp is treated with ketoconazole shampoo. This shampoo can also be used as a shower gel, rubbing the body with it every month for 3 days in a row for up to 5 minutes. The rest of the time, the skin is lubricated with 1% salicylic alcohol once a week.
Despite the fact that pityriasis versicolor is not considered a contagious disease, it is recommended to carefully monitor the contact of family members of the patient with his clothing, personal hygiene, or bedding. All those suffering from this disease must have their own set of bed linen, towels and clothing. During treatment, disinfection of the patient's linen and clothing is carried out by boiling in a 2% soap-soda solution, followed by ironing five times with steam. Synthetic materials should also be avoided. Preference should be given to cotton fabrics.
People suffering from pityriasis versicolor are advised to avoid stressful situations, increased physical activity, excessive sweating, and high temperatures. We should also not forget about strict adherence to the rules of personal hygiene.
Relapses
Tinea versicolor often returns after treatment, especially in the summer or while on vacation in warm, humid countries. The patient can reduce this likelihood by regularly using antifungal shampoos as a preventative measure. For example, using shampoo once a day for a few days before going on vacation can help prevent a recurrence of tinea versicolor.
If a patient develops tinea versicolor again after treatment, they can try treating it themselves with an antifungal shampoo or contact their GP for advice and other treatments. If the patient has frequent and severe episodes of tinea versicolor, the GP may consider prescribing antifungal tablets several times a month to prevent recurrence of the condition and recommend consultation with a dermatologist.