Mastocytosis in adults - symptoms and treatment
Many systemic and cutaneous forms are generally treated the same way. Therapy consists of two large parts: symptomatic and cytostatic (chemotherapeutic). The choice of treatment for mastocytosis depends on the aggressiveness of the process:
- Patients with indolent forms of mastocytosis, as well as mast cell activation syndrome, require symptomatic therapy [18]. Basic measures are taken to improve the patient's quality of life.
- In case of aggressive mastocytosis, along with symptomatic mastocytosis, antitumor treatment is also carried out.
Symptomatic therapy
Symptomatic treatment is aimed at preventing attacks and reducing symptoms of mastocytosis. As a rule, patients themselves know what factors cause attacks of the disease and avoid them.
To reduce the negative impact of mediators on the body and reduce the frequency and severity of attacks, constant use of antihistamines and mast cell membrane stabilizers is necessary:
- Antihistamines block histamine receptors. It is optimal to use “daytime” antihistamines with a long action. These are ebastine, cetirizine, fexofenadine, loratadine, etc. [19]
- Mast cell membrane stabilizers are drugs that block not only histamine in the blood, but also the release of all mediators in general. Such drugs include cromolyn sodium and ketotifen [19]. The disadvantage of cromolyn sodium is the low availability of tablet forms in the Russian Federation. In addition, taking the drug 3-4 times a day can be psychologically difficult for some patients. Unpleasant side effects of ketotifen include drowsiness.
Patients usually tolerate treatment with antihistamines and mast cell membrane stabilizers well, so they are suitable for long-term, even multi-year, use.
The use of antihistamines in pregnant women. Most antihistamines in Russia are not approved for use in pregnant women. However, studies show that drugs such as cetirizine and loratadine are safe for the fetus, so they can be used during pregnancy [23][24].
To relieve labor pain, epidural or general anesthesia can be used according to surgical protocols for mastocytosis. Before delivery, it is extremely important to administer an antihistamine and a glucocorticosteroid, since labor itself and stress can lead to the release of mast cell mediators [8].
To reduce itching , in certain groups of patients, ointments with glucocorticosteroids and PUVA therapy are used - irradiation of the skin with safe ultraviolet rays with the intake of a photosensitizer, which increases the sensitivity of the skin to ultraviolet rays [15]. Many patients note an improvement in their well-being after a light tan [22].
To slow down the process of bone demineralization and reduce the risk of fractures, constant intake of antihistamines, mast cell membrane stabilizers and calcium supplements is necessary. If osteoporosis develops, then the full range of drugs is used, including bisphosphonates, RANKL receptor blockers and low doses of interferon [10][20][21].
To cope with heartburn, antihistamines that act in the gastrointestinal tract are used: famotidine, ranitidine.
In case of anaphylactic shock, a subcutaneous injection of adrenaline is helpful as an emergency measure, so all patients with mastocytosis should have this drug with them. Adrenaline raises blood pressure and gives the patient time to ask for help. It is optimal to use special syringe pens with adrenaline (Anakit, Anahelp, etc.). If such a syringe pen is not available, simple adrenaline from an ampoule in a dose of 0.3 mg will do [19].
When people with mastocytosis seek medical care for other reasons, doctors should pay special attention to them because of the increased risk of anaphylaxis. For example, one study analyzed the incidence of complications after general anesthesia. It was found that in patients with mastocytosis, the incidence of severe complications of general anesthesia is 40 times higher than in patients without mastocytosis [8]. Standard drug preparation, consisting of a combination of an antihistamine and a corticosteroid, montelukast and a benzodiazepine, led to a decrease in the number of complications after anesthesia [8].
As with other rare diseases, it is important to educate patients and physicians about the risks of mastocytosis. For this purpose, regular meetings between patients and specialists are held and brochures are published. A Russian-language manual for patients with mastocytosis and their loved ones, which describes actions during vaccination and general anesthesia, is given in the list of references [38][39].
Correctly selected symptomatic treatment allows the patient to feel better and live a full life.
Cytostatic treatment
The developed treatment options are aimed at reducing the tumor mass - cytoreduction, which in this case is carried out using chemotherapy. Chemotherapy is indicated only for patients with aggressive mastocytosis. In extremely rare situations, cytostatics are also used in patients with severe mediator reactions, but this approach is not supported by all specialists.
Treatment of patients with the KIT D816V mutation. When choosing therapy, the variant of the KIT gene mutation is important. If the D816V mutation is detected in the KIT gene, then cladribine and interferon-alpha are used as the main drugs. Their effectiveness is approximately the same and is about 50% [18].
- Interferon-alpha is not a chemotherapy drug. This is an immunodrug that is devoid of many side effects of cytostatics (hair loss, immune suppression, etc.). Most often, on the days of administration, interferon causes flu-like symptoms: aching joints and bone pain, but these quickly pass. Interferon was invented a long time ago and is still successfully used to treat aggressive forms of mastocytosis. It must be administered subcutaneously. In general, the drug is well tolerated, so treatment is often started with it. However, sometimes you have to wait several months for results.
- Cladribine is used when it is necessary to quickly remove the maximum number of tumor cells. The risk of severe complications with cladribine is slightly higher than with other drugs, although the drug is generally well tolerated. Its effectiveness is about 55%, but it acts much faster than other drugs [26].
In the treatment of aggressive mastocytosis, tyrosine kinase inhibitors work well - a group of drugs with a “targeted” effect on the enzyme tyrosine kinase, the activity of which has a significant contribution to the development of the disease. Point-of-care drugs are also called “targeted” (from the English target - “target”). Dasatinib, nilotinib and mazitinib were tried for mastocytosis, but they were ineffective and were abandoned in daily practice [33]. The most effective drugs in this group are imatinib mesylate, midostaurin and avapritinib.
- Midostaurin gives a positive antitumor effect in 60% of patients, which is accompanied not only by a decrease in tumor mass and improved analysis, but also by a reduction in attacks and an improvement in general well-being [27]. The drug was recently registered in Russia and is beginning to enter clinical practice for the treatment of patients with mastocytosis.
- Avapritinib will be available in the coming years . According to the results of clinical studies, it turned out to be more effective than midostaurin, both in terms of antitumor effect and symptom reduction [32].
Treatment of patients without the KIT D816V mutation. Up to 15% of patients with systemic mastocytosis do not have the KIT D816V mutation. Imatinib is effective in such patients [29][30]. This drug is able to suppress some enzymes of tumor cells and completely cure a number of diseases. The drug is quite safe, but only patients who do not have the KIT D816V mutation are sensitive to it [29].
Allogeneic hematopoietic stem cell transplantation is the only method that can cure mastocytosis. However, the procedure is associated with risks, so it can only be used in a situation where all other methods of therapy have already been tried.
Causes
Mastocytosis occurs in two forms - cutaneous and systemic.
Cutaneous forms of mastocytosis occur mainly in children and are rare; there are no differences in the lesions in girls and boys. Most often, children under 2 years of age are affected; most cases of the disease resolve spontaneously by adolescence.
However, there is also an adult form - systemic mastocytosis, which is more severe and does not have a tendency to resolve itself.
The exact causes of the development of systemic mastocytosis and the mechanisms of its formation are still unknown; theories have been put forward about damage to some chromosomes with transmission of this type of disease in an autosomal dominant manner. However, half of the patients do not have a family predisposition.
Manifestations of systemic mastocytosis
In systemic mastocytosis, internal organs are infiltrated by mast cells in parallel with or without skin lesions.
At the same time, specific disturbances associated with their work appear in the affected organs. Most often affected:
- liver, with its enlargement, hardening and fibrous nodes (liver tissue is replaced by connective tissue),
- skeletal system, with the formation of areas of osteoporosis (softening of bone) and osteosclerosis (replacement of bone with connective tissue), bone pain,
- lymph nodes, with their enlargement and pain,
- digestive tract, with diarrhea and ulcerative lesions,
- the spleen, with its sharp enlargement,
- bone marrow with its changes and replacement of normal cells with mastocytes, or with damage to the bone marrow with the formation of leukemia,
- nerve tissue.
Manifestations of skin forms
In this form, the lesions mainly affect the skin. The main symptoms are
- skin itching,
- skin redness,
- heart attacks,
- pressure reduction,
- periodic rises in temperature.
These are manifestations of the release of special substances from mast cells - histamine and its analogues.
Mastocytosis is characterized by five main types of skin lesions.
1. Maculopapular manifestations. In this case, multiple red-brown spots with strong pigmentation appear. When a special friction test is performed (Daria-Unna test), they take on the appearance of red bumps.
2. Nodular type - the appearance inside the skin of multiple spherical nodes up to 1 cm in size, with a dense consistency of red, pink or yellow color. The surface of the nodes is smooth, the Daria-Unna test is negative. The nodes may merge into plaques.
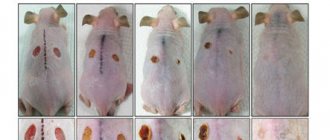
3. Formation of mastocytomas - single nodes ranging in size from 2 to 5 cm, smooth or wrinkled into an “orange peel”, with the consistency of rubber. Up to 3-4 nodes may appear on the neck, torso, and forearms. The Daria-Unna test is positive, and if the surface of the node is injured, blisters or pustules and tingling may appear on it. When they develop back, the skin above them sinks and wrinkles.
4. The erythrodermic or diffuse form is large, itchy, brown-yellow lesions in the area of the armpits or buttock folds. They have an irregular shape with clear boundaries and are dense to the touch. Due to friction, the surface can become ulcerated, scratches and cracks occur. As the lesions progress, the lesions spread and the skin becomes dense, the consistency of dough, and its color ranges from pink to dark brown. The Daria-Unna test is sharply positive, and minor trauma to the lesions results in the formation of blisters and itching. Gradually the process regresses.
5. The telagioectasia form mainly occurs in women and is manifested by red-brown spots consisting of a cluster of dilated subcutaneous vessels. These spots vary in shape and size and are located on a sharply pigmented skin base. Blisters appear at the site of their friction, mainly the chest and limbs are affected, itching and spread of the process to the bones are possible.
Forms of mastocytosis
Based on the clinical features, course of the disease and age of its onset, the following forms of the disease are distinguished:
- Infantile cutaneous form of mastocytosis: on average, the age of the lesion is up to 2 years, the symptoms gradually disappear, there is no transformation into a systemic process.
- Solitary (single) mastocytomas: the formation of lesions limited to several zones (nodes).
- Cutaneous mastocytosis in adolescents or adults: Systemic lesions are common but will not progress. However, a complete cure also does not occur.
- A cutaneous form similar to the previous one, but with the possibility of transition to systemic mastocytosis, which affects the internal organs.
- Systemic form with damage to internal organs.
- A malignant form of mastocytosis in the form of mast cell leukemia. This is a particularly severe form with an unfavorable prognosis and a rapid course.
Photo: website of the Department of Dermatovenereology of the Tomsk Military Medical Institute
Diagnostics
The basis of diagnosis is clinical manifestations and the detection of a large number of mast cells in tissues and skin.
First of all, they examine the blood, detecting changes in the formula, a large number of mast cells and their waste products (histamine and tryptase).
A biopsy of the skin, organs and bone marrow is performed to determine the abundance of mast cells, determine the type and anomalies of their development (especially tumor ones).
A chromosomal analysis is carried out to determine anomalies associated especially with chromosomes 11 and 20, less often 5 and 7.
Additionally, X-rays of bones are performed to determine the level of cell damage, as well as densistometry and MRI of bone tissue.
To diagnose disorders of internal organs, ultrasound and CT are performed, especially for the liver or spleen. If the digestive tract is damaged, endoscopic diagnostic methods are necessary.