It is believed that acne (acne) is mainly affected by teenagers - during a difficult transition period, both boys and girls experience global hormonal changes in the entire body. Many adults also face the problem of acne. Moreover, it is not immediately possible to find out the causes of such a disease in them. It’s one thing if the disease is mild. It’s completely different when acne leaves scars, scars and blemishes. Getting rid of them is very difficult, sometimes almost impossible. That is why it is necessary to actively engage in treatment. An anti-acne lotion can help with this.
Why do acne appear?
Modern hygiene products, it would seem, should have long ago saved us from such an unpleasant phenomenon as acne. But the causes of the disease are not related to the frequency of washing, but to the functioning of the sebaceous glands. So, the main causes of acne are:
- hereditary predisposition to acne;
- the occurrence of various types of inflammation on the skin (for example, allergic reactions);
- hormonal imbalance, which can occur, among other things, due to stress;
- constant exposure to too hot and humid climates;
- hyperseborrhea (too oily skin);
- excess sebum produced by the skin.
In the latter case, the glands become clogged due to the mixing of sebum with dead cells. Next, bacteria begin to actively multiply, the skin becomes inflamed, and a pimple appears in this place.
Interest in the problem of acne does not decrease. This dermatosis is most common among adolescents (affects up to 85% of both boys and girls), which is primarily due to the imperfection of anti-acne therapy. On the one hand, the low effectiveness of treatment causes the persistence of the disease with the formation of nosogenic psycho-emotional disorders, predominantly of the depressive spectrum, in approximately 40% of patients; on the other hand, dermatosis is fraught with the development of local and systemic adverse events [3, 4].
The initial link in the pathogenesis of acne is an increase in sebum production (as a result of relative or absolute hyperandrogenism), the key is follicular hyperkeratosis, which is clinically manifested by open and closed comedones. The duct of the pilosebaceous follicle (SVF) is inhabited by aerobic staphylococci and micrococci, facultative anaerobes Propionibacterium acnes
and
P. granulosum
.
Anaerobic conditions in the lower part of the SVF duct are unacceptable for aerobic bacteria, and therefore staphylococci and micrococci are localized in the upper part of the SVF duct and do not play a significant role in the pathogenesis of acne, unlike P. acnes
.
Density of skin colonization by microorganisms P. acnes
varies with age, reaching a maximum during puberty.
The highest density of P. acnes
is observed in seborrheic areas, since sebum is a breeding ground for these microorganisms.
It has been established that P. acnes
directly and indirectly influences the occurrence of both non-inflammatory acne (open and closed comedones) and inflammatory acne (papules, pustules, nodules). Extracellular lipase of microorganisms hydrolyzes sebum triglycerides to glycerol, which is a nutrient substrate for microorganisms and free fatty acids that have comedogenic properties. Antigens of microorganisms attract mononuclear phagocytes and neutrophils to the SVF from peripheral blood, which produce interleukins (IL)1α, -1β, -6 and -8; tumor necrosis factor alpha (TNF-α), stimulate the complement system. These proinflammatory cytokines activate the enzyme cyclooxygenase, resulting in the formation of the main inflammatory mediator leukotriene B4 (LTB4) from arachidonic acid, which stimulates neutrophils, T lymphocytes, monocytes and eosinophils with their subsequent release of hydrolytic enzymes and nitrogen monoxide (NO).
Inflammation within the SVF is the main factor in the formation of papulopustular and conglobate acne. Currently, 211 inducer genes and 18 suppressor genes responsible for this process have been identified. The production of IL-1α is sharply increased in the circumference of the comedon, which contributes to hyperkeratosis caused by the hyperproduction of keratin types 6 and 16, as well as fillagrin in the infrainfundibulum
SVF.
Proinflammatory toll receptors types 2 and 4, located on the surface of immunocompetent cells, are activated by P. acnes
. On the other hand, the level of antimicrobial peptides, such as defensin 1 and 2, is directly related to the content of free fatty acids [3, 4].
Oxygen and microorganisms break down triglycerides into free fatty acids, which have a pronounced comedogenic effect, thereby promoting the progression of hyperkeratosis (as well as squalene peroxidation products), which correlates with the level of pro-inflammatory IL-6. The oxidation products of saturated fatty acids are ligands for binding to the PPAR zone of the dimeric retinoid-sensitive receptor, which is normally responsible for lipogenesis and inflammation. A change in the ratio of saturated and unsaturated fatty acids in sebum is considered an initial factor in follicular hyperkeratosis and subsequent inflammation. It is known that a high content of unsaturated fatty acids (linoleic and linolenic) prevents comedonogenesis and suppresses sebum production (inhibition of the enzyme 5α-reductase). In addition, unsaturated fatty acids have pronounced antimicrobial and anti-inflammatory activity due to the suppression of LTV4 expression [20, 21]. Destruction of the wall of the sebaceous gland with the release of its contents into the dermis causes a picture of inflammation, manifested in the form of papules, pustules, nodules and cysts.
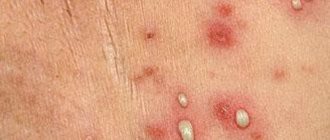
Acne rashes are represented by a pseudopolymorphic rash, which is characterized by a clear stage in the evolution of elements. Initial skin changes in acne are represented by open or closed comedones (according to the level of obstruction of the SVF duct). A comedon is a “cast” of the SVF duct, consisting of rejected corneocytes and microorganisms glued together with sebum. Open comedones, unlike closed comedones, resolve spontaneously and without a trace in approximately 80% of cases. The addition of an inflammatory reaction around the comedone leads to its destruction and the subsequent formation of papules and then pustules. The development of an inflammatory reaction in the dermis leads to the formation of nodes, and when they suppurate, cysts. The resolution of comedones, papules and pustules occurs without a trace. Nodules and cysts leave behind foci of dyspigmentation and, depending on the fibroplastic response of the skin, hypotrophic ( ice - pick
), hypertrophic or keloid scars. To assess the severity of acne (SSA) in practice, the most convenient classification is proposed by the American Academy of Dermatology (as quantitatively modified by M.A. Samgina and S.A. Monakhov, 2002) [2-4]:
— I degree is characterized by the presence of comedones (open and closed) and up to 10 papules;
— II degree — comedones, papules, up to 5 pustules;
— III degree — comedones, papulopustular rash, up to 5 nodes;
— IV degree is characterized by a pronounced inflammatory reaction in the deep layers of the dermis with the formation of multiple painful nodes and cysts.
Among acne-like rashes, the most noteworthy are drug-induced acne and gram-negative folliculitis, which in some cases are inevitable side effects of irrational anti-acne therapy with external and systemic antibacterial drugs. Drug-induced acne is characterized by sudden onset, widespread monomorphic rashes (papules or pustules) with frequent involvement of the skin of the distal extremities. The most common drugs that can provoke acne-like rashes are tuberculostatics (isonicotinic acid, isoniazid, ethionamide, rifampicin, ethambutol), anticonvulsants (trimethadione, diphenylhydanthione, phenytoin, barbiturates), lithium preparations, azathioprine, cyclosporine A, chloral hydrate, vitamins B1, B2, B12, D, tetracycline and streptomycin antibiotics, disulfiram, thyreostatic drugs, gold salts, medications containing iodides and bromides (iodine-acne, bromine-acne), oral contraceptives containing progestins with androgenic activity (levonorgestrel) [3, 4, 9].
Gram-negative folliculitis is an iatrogenic complication of long-term antibiotic therapy (systemic or external). Type I is characterized by a rash grouped in the perioral and perinasal areas (but other localization is possible) in the form of pustules with whitish contents, surrounded by a narrow rim of hyperemia; for type II - a papular-nodular rash, from the elements of which microorganisms of the genus Proteus
. Etiopathogenetically, this dermatosis is based on a violation of the bacterial biocenosis in the SVF. Long-term use of antibiotics suppresses the vital activity of gram-positive saprophytic microflora of the skin, which suppresses the vital activity of gram-negative microorganisms [4, 13, 31].
Among the external antibacterial agents, erythromycin and clindamycin are distinguished, which are prescribed for II-III degrees of severity of the process, both as monotherapy and in combination with external and systemic anti-acne drugs. It should be noted that today monotherapy for acne with local or systemic antibiotics is not recommended; preference should be given to combination agents that include an agent that prevents the development of bacterial resistance.
In women, a combination of local antibacterial drugs and combined oral contraceptives with antiandrogenic and antimineralkorticoid effects (Jess Plus, Yarina Plus) is possible. Considering that the clinically significant anti-acne effect of these drugs appears no earlier than the 3rd month of therapy, it is advisable for most patients with papulopustular rashes to be prescribed external antibacterial drugs during this period that quickly relieve inflammatory symptoms [1, 9, 10, 21, 26 ].
Slower healing of inflammatory acne lesions is due to the presence of inflammatory mediators synthesized by P. acnes
;
pronounced resistance of P. acnes
to destruction by neutrophils and monocytes;
persistence of P. acnes
(phagocytosed bacteria remain viable for a long time, despite the antimicrobial effect).
In addition, hypersecretion of sebum does not allow creating the necessary concentration of antibiotic in the SVF duct [11, 20]. Based on this, it follows that to reduce the mass of P. acnes
in spill elements by 10% of their initial amount, at least 3 weeks of treatment with antibacterial drugs is necessary [11].
Considering that during the first 2-3 weeks of using external anti-acne agents based on azelaic acid, benzoyl peroxide, adapalene, tretinoin and retinoic acid, the development of drug-induced dermatitis is inevitable, leading in some cases to the patient’s refusal to continue therapy, then according to the parameters the effectiveness / tolerability combined preparation for external use erythromycin (4%) + zinc acetate (1.2%) - Zinerit
- is preferable for II-III severity of the process, both as monotherapy for acne and in combination with antiandrogens and systemic retinoids during the first 2-3 months of systemic anti-acne therapy [1-4].
Pronounced anti-acne effect of Zinerit
explained by its influence on all parts of the pathogenesis of acne.
Erythromycin binds to the 50S ribosomal subunit, which is found only in bacteria, which leads to disruption of the synthesis of all proteins and stops the growth of bacteria. Analysis of data on antibiotic resistance demonstrates a clear pattern in the form of higher resistance of P. acnes
isolated from acne patients to drugs that have been used for a long time in the treatment of this dermatosis.
Thus, according to the results of a study conducted in 13 European countries and including 304 strains of P. acnes
isolated from various areas of the skin (77 isolates), the level of resistance to erythromycin was 17.1%, clindamycin - 15.1%, tetracycline - 2, 6%, with 100% sensitivity to benzylpenicillin, vancomycin and linezolid [22].
It has been demonstrated that the presence of zinc helps prevent the development of bacterial resistance to erythromycin. For example, in a study by B. Dreno et al. [34] it was found that initially erythromycin-resistant strains of P
.
acnes
(minimum inhibitory concentration of at least 1024 μg/ml) restored sensitivity to this antibiotic when zinc gluconate was added to the medium in increasing concentrations (7.5, 15 and 30 mg/l), while at the maximum of these concentrations sensitivity to erythromycin was completely was recovering.
However, a high proportion of erythromycin-resistant P
.
acnes
should be considered as an undeniable advantage compared to broad-spectrum antibiotics and low resistance to them on the part of normal skin flora.
The uncontrolled use of “strong” antibacterial drugs for acne is nothing more than relics of the dark past of dermatology, when acne was classified as a group of pyoderma. Erythromycin, without leading to total elimination
of
P. acnes
from the surface of the skin, does not disrupt the biocenosis of the skin, and thereby does not contribute to the development of gram-negative folliculitis, but mainly has only a pronounced anti-inflammatory effect. The concentration of erythromycin (4%) promotes optimal penetration of the drug into the skin. By reducing microbial contamination, erythromycin eliminates or sharply weakens both the second and fourth factors in the pathogenesis of acne - follicular hyperkeratosis and inflammation, respectively [1].
Zinc, which is part of the drug, inhibits the enzyme 5α-reductase type I, thereby preventing the transition of testosterone to dihydrotestosterone, and, as a result, weakening the initial factor in the pathogenesis of acne - androgen-mediated hypersecretion of sebum, which contributes to the sebostatic effect [23].
In addition, zinc has anti-inflammatory and antiseptic activity. In a study conducted by V. Jarrousse et al. [17], using immunohistochemical studies of human keratinocyte cell cultures and human skin samples treated with P. acnes
A 3-hour incubation with zinc salts (1 μg/ml) demonstrated a significant decrease in the expression of TLR-2 receptors, which was absent in the control group.
Apparently, this effect is one of the mechanisms responsible for the anti-inflammatory effect of zinc. Another mechanism of this action is associated with inhibition of inducible keratinocyte NO synthase (iNOS), the enzyme responsible for the production of NO by keratinocytes. In particular, iNOS activity is increased in acne, leading to the production of large amounts of NO. The latter, in turn, interacts with superoxide anion (O2–), which is accompanied by the formation of peroxynitrite (ONOO–), a cytotoxic agent that causes tissue damage and inflammation [32]. J. Yamaoka et al. [33] demonstrated that zinc ions in vitro
inhibit TNF-α and interferon-γ-stimulated iNOS expression by keratinocytes, which determines the anti-inflammatory effect. In addition to inhibition of iNOS expression, suppression of the activity of this enzyme under the influence of zinc, mediated by calmodulin, is also possible, as was demonstrated in a study by G. Abou-Mohamed et al. [6]. Another mechanism through which the anti-inflammatory effect of zinc is achieved, demonstrated in a study by A. Guéniche et al. [14], suppression of the expression of intercellular adhesion molecules and TNF-α by keratinocytes stimulated with interferon or nickel. Finally, the ability of zinc described above to suppress the degranulation of mast cells and basophils leads to a decrease in the concentration of inflammatory mediators released by them, in particular histamine.
The antioxidant properties of zinc are also well known [7, 27]. It has been established that zinc reduces damage to cells and their genetic apparatus caused by UV irradiation and increases the resistance of skin fibroblasts to oxidative damage [24, 25]. Zinc has a proven epithelializing property and takes an important part in the healing process of wounds, including excoriated acne [19]. This effect is mediated by several mechanisms. First of all, the normal healing process requires zinc-containing enzymes - matrix metalloproteinase and alkaline phosphatase. Zinc also has a moderate antibacterial effect [19]. An extremely important property of zinc is its ability to prolong the antibacterial effect of erythromycin on the skin due to retention of the antibiotic in the stratum corneum of the epidermis [16].
Zenerit solution
optimal for monotherapy of non-severe limited forms of acne.
A number of clinical studies have proven the high clinical effectiveness of the drug Zinerit
[8, 15, 18].
Thus, in a randomized study by L. Schachner et al. [28], conducted with the participation of 103 patients, demonstrated significantly greater effectiveness of the Zinerit
compared to 1% clindamycin phosphate gel;
at the same time, the severity and speed of onset of the clinical effect were significantly higher when using Zinerit.
In comparison with systemic antibacterial therapy,
Zinerit
also demonstrated equal or superior clinical efficacy.
Thus, in a double-blind controlled study conducted by C. Feucht et al. [12], involving 149 patients, showed equal effectiveness of Zinerit
and systemic tetracycline therapy at a daily dose of 500 mg.
In another multicenter, single-blind study conducted by J. Stainforth et al. [29], covering 105 patients, demonstrated higher efficacy of Zinerit
compared to oral therapy with minocycline at a daily dose of 100 mg.
In a double-blind study conducted by J. Strauss et al, [30] it was found that by the end of the 10th week of using the Zinerit
in acne patients,
P
.
acnes
by 98%, and by the end of the 4th week the content of free fatty acids in sebum decreases by 69%.
It should be noted the rapid development of the clinical effect when using the drug Zinerit
.
Based on a comparison of data from the instructions for the medical use of external preparations for the treatment of acne, registered in the Russian Federation, it follows that when using benzoyl peroxide, improvement is observed after 4 weeks, persistent improvement after 3 months [35]; azelaic acid—improvement after 4 weeks, persistent improvement after several months [36]; adapalene - improvement after 4-8 weeks, persistent improvement after 3 months [37]; external preparations of clindamycin - satisfactory results after 6-8 weeks of treatment [38]. According to the instructions for medical use of the drug Zinerit, visible improvements are possible after 2 weeks of treatment [39]. According to a clinical study by A.M. Lukyanova et al. [40], clinical improvement during treatment with Zinerit
was observed after 4 days of treatment.
Finally, according to a marketing study in which a survey of 300 patients suffering from acne was conducted, respondents noted an effect already on the 1st day of treatment with Zinerit
[41].
The indicated properties of the drug Zinerit
combined with the convenience of its use, have led to the fact that, according to retail pharmacy sales from IMS, in recent years this drug has been one of the popular anti-acne agents in Russia.
In the study conducted by A.Yu. Sergeev et al. [5] pharmacoepidemiological study of acne therapy based on anonymous assessment of treatment results by patients themselves, on the dynamics of demand for basic OTC products for the treatment of acne in the Russian Federation in 2010-2012. priority belongs to the Zenerit solution.
The results of an anonymous survey of 4660 acne patients (83% women, average age 22 years) on the website
www
.
ugrei
.
net
showed the advantages of the
Zinerit
in most individual assessments (in particular, safety, convenience and accessibility), as well as in the cost-effectiveness indicator.
The success of acne therapy largely depends on the patient's adherence to the prescribed treatment regimen. It was found that on average 28% of patients adhere to the treatment regimen recommended in the instructions, while higher subjective assessments were associated with longer use of drugs. In this context, the simplicity/convenience of using the drug Zinerit
and quick visible results contribute to patient adherence to treatment, which has a positive effect on its results.
Using the applicator, Zinerit
Apply a thin layer to the area of skin affected by acne.
To do this, tilt the bottle down with light pressure - this is how the active solution is formed. The application speed can be adjusted by the pressure applied by the applicator. An approximate single dose is 0.5 ml, 30 ml in a bottle. After drying, the solution becomes transparent, does not leave marks on the skin and clothes, after its use it is possible to apply makeup or use non-comedogenic cosmetics. If necessary, the patient can apply moisturizing creams 20 minutes after applying Zinerit
.
The drug must be used 2 times a day, the average duration of treatment is 10-12 weeks. Unlike external preparations based on retinoic acid (and its derivatives) and benzoyl peroxide, as well as systemic antibacterial drugs of the tetracycline and fluoroquinolone groups, Zinerit
does not interact with the sun (there is no photosensitization), which significantly expands its use in the spring and summer, as well as in resorts with increased insolation.
Once the therapeutic effect is achieved, it is advisable to use the zinc-erythromycin complex 1-3 times a week as maintenance therapy to maximize remission.
In women with moderate-to-severe acne localized on the face and trunk, as well as those with premenstrual exacerbation of the process, after consultation with a gynecologist, basic therapy with a microdose drospirenone-containing drug prescribed in the “24+4” mode for a period of at least 6 months is advisable. Zinerit solution to most patients during the first 2-3 months
to achieve a clinical effect more quickly (without the risk of irritating effects of the drug).
For severe forms of acne (conglobate, resistant to other types of anti-acne therapy), both men and women are prescribed therapy with systemic isotretinoin (isotretinoin + Lidose) in accordance with the daily dosage and the total course dose for a period of 8 months (with a minimum daily and course dosage) . Considering the exacerbation of the process in most patients in the first 2 months of therapy, it is advisable to use Zinerit
, which allows you to quickly neutralize the exacerbation of acne.
The purpose of our work is to evaluate the anti-acne effectiveness and tolerability of Zinerit
as monotherapy in 34 patients (14 men, 10 women) with grade III acne (group 1); in the form of combination therapy in 18 women with grade III acne who received a microdosed drospirenone-containing drug in the “24+4” dosing regimen (Jess plus) (group 2) as basic therapy, and also as concomitant therapy in 11 patients (8 men, 3 women) with conglobate acne who received systemic isotretinoin + Lidose (acnecutane) as basic therapy (group 3).
The dynamics of the number of open and closed comedones, papules, and pustules was assessed before and after treatment. At the specified time, along with the calculation of acne elements, a procedure was carried out to determine the level of sebum secretion (USS) using the Sebumeter SM 810 device (Cou-rage+Khazaka electronic GmbH, Germany). The principle of operation of the device is based on the quantitative determination of sebum using the photometric method (normally, USC is 60-90·10–6 g/cm2).
In the group of patients receiving Zinerit
as monotherapy, the average duration of treatment was 74±7 days - during this period comedones, papules and pustules regressed by 74.8, 81.6 and 97.4%, respectively (Fig. 1).
In patients with grade III acne who received basic therapy with Jess Plus, the duration of use of Zinerit
was 56±4 days - during this period comedones, papules and pustules regressed by 56.1, 85.4 and 89.1%, respectively (Fig. .2).
In 11 patients with conglobate acne, during the first 2 months of therapy with systemic isot-retinoin + Lidose, a pathogenetically caused exacerbation of the process was noted, which, given the best tolerability among external anti-acne drugs, was eliminated in 34 ± 12 days using Zinerit
.
Rice. 1. Patient D., 23 years old, with grade III acne.a - before treatment; b - after 6 weeks of using the Zinerit solution.
Rice.
2. Patient F., 21 years old, with acne of II severity. a - before treatment; b — after 6 months of taking a low-dose combined oral contraceptive (in addition, Zinerit solution was used externally for the first 4 weeks). USCS (10–6 g/cm2) before and at the end of therapy was: 216±22 and 179±18.2·10–6 g/cm2 in patients of group 1, 238±27 and 160±16.4·10 –6 g/cm2 - in the 2nd group and 252±31 and 138±19.5·10–6 g/cm2 - in the 3rd group.
Tolerability of therapy with Zinerit
was good in all patients.
Three patients of group 2, during the 1st week from the start of therapy, noted slight dry skin after applying the drug, which did not require drug correction and disappeared on its own within a week. Summarizing our long-term results of using all the main external anti-acne agents in patients with acne, it should be emphasized that the best tolerability was noted in the group of patients receiving mono- or combined (with antiandrogen drugs) therapy with Zinerit
, and the fastest anti-acne effect was achieved due to the absence of a period of drug-induced dermatitis and exacerbation of acne, which is invariably present at the beginning of a course of treatment with external preparations with a pronounced irritating potential (see table) [2].
The severity of the phenomena of drug dermatitis (on a 3-point scale) from the use of external anti-acne drugs
. Thus, the effect of Zinerit
, which affects all parts of the pathogenesis of acne, allows us to consider this anti-acne drug as the method of choice:
- in patients with acne of II-III severity and a process limited to the facial area, in the form of monotherapy;
- during the first months of anti-acne therapy in women with grade III acne receiving basic antiandrogenic drugs;
— for rapid relief of exacerbation of the process in patients receiving systemic isotretinoin therapy for severe forms of the disease.
The results of our own observations on the effectiveness and tolerability of therapy support this recommendation.
The author declares no conflict of interest.
Acne lotion “PROPELLER”: simple and reliable
For skin familiar with such a problem as acne, “PROPELLER” was developed - a special anti-acne lotion. A product with cincidone is an effective and quick way to cleanse the skin. According to reviews from consumers who have already evaluated the product, it not only copes with visible “blackheads”, but also normalizes the functioning of the sebaceous glands.
Features of acne lotion:
The “Propeller” cosmetic series lotion for acne has the following quality characteristics:
- antimicrobial properties;
- effective and rapid reduction of acne;
- prevention of the appearance of new inflammations;
- removing oily shine;
- smoothing skin texture;
- noticeable tonic effect.
The market offers therapeutic and prophylactic preparations “Propeller”, which allow you to easily cope with acne and its manifestations: enlarged pores and blackheads. Clinical trials and reviews from our consumers are the best confirmation.
Tsindol is indicated for such skin lesions as:
- bedsores;
- diathesis;
- chickenpox;
- sweat rashes;
- dermatitis;
- streptoderma;
- pityriasis rosea;
- simple herpes.
Thanks to the unique composition of the medicinal components of the suspension, the following effects are exerted on the body:
- cleansing contaminated pores;
- suppression and elimination of bacteria, microbes, works as an antiseptic;
- disinfects fabrics;
- healing of small skin wounds;
- drying of the skin;
- normalization of metabolism under the skin;
- relief and elimination of the inflammatory process;
- reduction and elimination of greasiness and oiliness of the skin;
- narrowing of capillaries, vascular walls become thicker;
- skin softening;
- creating a kind of protective coating;
- relieving pain, giving the skin tonic properties;
- prevention of the formation of acne and pimples.
Tsindol disinfects the skin and this allows you to effectively prevent new skin rashes.
Instructions for use
Here are the general rules for using the suspension in case of pimples and acne:
- the drug has a strictly external effect, it is strictly forbidden to take it internally;
- a test should be performed on the skin (wrist), if there are no painful manifestations, then treatment can begin;
- do not forget to shake the contents of the bottle until it has a uniform milky color;
- the suspension is not rubbed into the skin;
- Before use, you need to wash the affected areas of the skin with warm water, then carefully remove the moisture with a towel;
- the suspension is applied to individual pimples with a hygienic stick or cotton swab;
- the dried layer of suspension is removed with a soft cloth;
- If the suspension gets into your eyes, rinse them immediately with plenty of water.
Instructions for use for acne zindol recommend performing the procedure 3-5 times a day over a weekly course.
The applied layer of the drug dries out after 10-15 minutes and is then removed with a dry cloth.
Important:
In this case, the resulting deposit does not need to be washed off with water.
For problematic oily skin with a characteristic glow and rashes, you can make masks from a suspension. It is advisable to apply the cindol mask at night, as after the procedure a whitish coating remains on the face.
Instructions for acne lotion “PROPELLER”
Using Propeller, a lotion specially designed to fight acne, is as easy as shelling pears:
- apply a small amount of acne lotion to a disc or cotton wool and gently wipe the inflamed areas of the skin (you can use it without restrictions);
- For faster and more effective results, anti-acne products should be used in combination, for example, apply a special cream after the lotion, and additionally use a gel or scrub several times a week.
Review
Propeller preparations are a simple and reliable way to forget about unpleasant blackheads forever! Easy to use, no skin tightness, on the contrary, only positive emotions.