Tuberculosis is an infectious disease that occurs due to Koch bacilli entering the human body. The disease is dangerous because it affects the respiratory system. Less commonly susceptible to tuberculosis are the bones, skin, lymphatic, genitourinary, nervous, lymphatic systems, as well as other organs and systems.
The immune system (the body's natural defense against infection and disease) of most healthy people kills the bacteria without causing symptoms. Sometimes the immune system cannot kill bacteria, but can stop it from spreading in the body. In this case, no symptoms develop, but the bacteria remain in the body. This is called latent (hidden) tuberculosis.
Etiology of the disease
- The causative agent of skin tuberculosis is Mycobacterium tuberculosis, which was first discovered by R. Koch in 1882.
- The tuberculosis bacillus belongs to the family of radiant fungi, the genus of mycobacteria, which, in addition to it, includes the causative agents of leprosy, scleroma and more than 150 species of atypical mycobacteria.
- Mycobacteria reproduce by division and budding. This process lasts 24 hours.
- MBT exhibit significant stability in the external environment. They cannot be frozen out. They remain viable in boiling water for up to 15 minutes. They live in manure for up to 15 years, and up to 1 year in wastewater. When dried, the pathogen remains viable for 3 years.
- Mycobacteria are resistant to phagocytosis (macrophages cannot destroy the mycobacterium, although they begin to fight it - incomplete phagocytosis).
- There are human, bovine and intermediate types of MBT.
- The pathogen has the appearance of an elongated rod of a rather complex structure: a three-layer cell wall and intracellular membrane contain polysaccharides, lipoprotein complexes and proteins. Proteins are responsible for antigenic properties (tuberculin). Polysaccharides play a role in antibody detection. Lipid fractions help MBT resist acids and alkalis.
Rice. 2. Mycobacterium tuberculosis.
How to treat tuberculosis?
Treatment of the pathology depends on its type, but most often a course of antibiotics is prescribed. Tuberculosis is a dangerous disease that requires immediate treatment. This allows the person to return to their normal lifestyle.
Antibacterial therapy is aimed at suppressing the proliferation of the tuberculosis pathogen.
Treatment takes place in 2 phases: in the first, several drugs are used at once to reduce the population of microbacteria, the second phase is maintenance therapy. Antibiotics stop the proliferation of bacteria and their release into the environment, the inflammatory process.
After taking such potent medications, a person needs additional supportive therapy that will strengthen the body and reduce the toxic effect. For this, immunostimulants (restore liver function), sorbents (remove toxic breakdown products of chemotherapy drugs) and vitamin complexes are prescribed.
After taking the drugs for two weeks, most people are no longer contagious and feel much better. However, it is very important to continue taking your medications as directed by your doctor and complete your entire course of antibiotics.
Ways of spreading skin tuberculosis
- Patients with tuberculosis spread the infection through sputum, urine, through fistulas and household items. The source of infection is also sick animals and food products contaminated with MBT from sick animals. During the formation of immunity, primary skin tuberculosis occurs (tuberculous chancre, lichenoid tuberculosis of the skin).
- There are a number of diseases that are associated with tuberculosis not directly, but indirectly. These are allergic vasculitis, resulting from allergic immune (“paraspecific”) inflammation in response to infection with mycobacteria (rosacea-like Lewandowski tuberculide).
Rice. 3. The photo shows tuberculosis of the skin of the face and neck.
Methods of transmission
- Airborne - through the sneezing, coughing of a patient with an open form of the disease, and even when drying out, the bacillus retains its pathogenicity.
- Alimentary – through the digestive tract. The infection enters the body due to poor hand hygiene or poorly washed and unprocessed food.
- Contact – the infection enters a person through the conjunctiva of the eyes, through kissing, sexual contact, through contact of contaminated objects with human blood, or the use of other people’s hygiene items.
Pathomorphology
With tuberculosis, a tubercle (tuberculum) appears around the embedded tuberculosis bacilli, the components of which are:
- inside the tubercle there are phenomena of caseous necrosis (damage) of tissues and Mycobacterium tuberculosis (a component inherent only in tuberculosis);
- surrounded by MBT cells specific for any granulomatous disease - lymphocytes, epithelioid cells and Pirogov-Langhans cells (cell proliferation);
- the outer layer (exudative component) is represented by cells macrophages, neutrophils, eosinophils (nonspecific component).
Rice. 4. Histological preparation of a tuberculous tubercle.
With tuberculous skin lesions, tubercular structures with a nonspecific inflammatory infiltrate are more common (there are few or no MBTs in the tubercle). Tuberculous granulomas are characteristic of tuberculous lupus. With allergic vasculitis that occurs in response to exposure to mycobacteria and their decay products, diffuse forms of skin tuberculosis occur. In this case, the vessels of the skin and subcutaneous tissue are affected.
Treatment
Chemotherapy, antibiotics
Bactericidal and bacteriostatic drugs are used to achieve complete recovery. In this case, the correct combination of drugs is important, taking into account the resistance of some bacteria to this type of therapy. First, treatment is aimed at suppressing the growth of bacteria and eliminating their resistance to medications. Residual infection in the cells is then eliminated. Duration of therapy is 6-12 months.
Surgery
Pulmonary resection is practiced as a radical technique. The operation is performed for bronchial stenosis, fibrous-cavernous lesions, pleural empyema, abscesses in the lungs, tuberculomas prone to progression, etc. In addition, decortication is used, that is, removal of fibrous layers, and cavernotomy - cleansing of the opened cavity.
DOTS
A treatment system consisting of several levels: bacterioscopic examination, chemotherapy, anti-tuberculosis treatment.
Sources:
- N.M. Koretskaya. Tuberculosis in children and adolescents in modern conditions // Siberian Medical Review, 2010.
- A.V. Mordyk, E.A. Tsygankova, L.V. Puzyreva, A.A. Turitsa. Tuberculosis in children of the Russian Federation at the present stage // Pediatric pharmacology, 2014, v. 11, no. 3, pp. 27-30.
- https://www.ncbi.nlm.nih.gov/pubmed/24548085 Marais BJ. Tuberculosis in children // J Paediatr Child Health. 2014 Oct;50(10):759-67. doi: 10.1111/jpc.12503. Epub 2014 Feb 19.
- V.N. Krivohizh. Modern methods of early detection of tuberculosis among children and adolescents // Health is the basis of human potential: problems and solutions, 2013, pp. 570-585.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Primary cutaneous tuberculosis
This form of the disease is extremely rare. The disease develops during the development of primary tuberculosis. Children under 10 years of age are most often affected. Initially, a papule appears reddish-brownish in color. Next, an ulcer (tuberculosis chancre) appears in the center of the papule. Peripheral lymph nodes increase in size. Often ulcerate. Ulcers take a long time to heal. In their place, thin scars appear. With a weakened immune system, the disease returns again, disfiguring the body with scars and scars.
Types of tuberculosis
- Open form - the disease is clearly expressed, bacteria are easily detected in sputum and feces. The patient himself poses a danger to others, since the infection is transmitted by airborne droplets. Microbacteria can be found in sputum, urine, and feces.
- Closed form - not dangerous to others. Characterized by the difficulty of detecting infection in sputum. The most common tuberculosis is pulmonary tuberculosis, but this infection can also affect bones, joints, genitourinary system, intestines, peritoneum, meninges, central nervous system, peripheral lymph nodes, skin
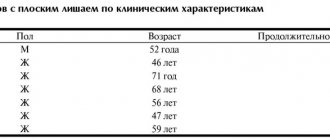
Secondary tuberculosis of the skin
The disease is represented by a variety of localized and disseminated forms that appear in previously infected people. Tuberculous lupus accounts for up to 75% of all cases.
In the last 10 years, there has been a predominance of disseminated forms of cutaneous tuberculosis.
Ordinary or vulgar tuberculous lupus (Lupus vulgaris)
In the recent past, lupus was the most common form of cutaneous tuberculosis. Today, disseminated forms are more often recorded. MBT penetrate into the skin from regional lymph nodes through the lymphatic tract and hematogenously (with the bloodstream). The disease often occurs in childhood, lasts a long time, with periodic exacerbations, and spreads slowly.
Symptoms of the disease
The disease affects the skin of the nose, face, neck, red border of the lips, mucous membranes of the mouth and eyes. The skin of the extremities is rarely affected. Tuberculous tubercles merge and form lupomas. Their color is yellowish-rusty. Size – up to 0.75 mm. At first, the lupomas are located deep, and then they begin to protrude above the skin.
The shape of the lupoma is round, the consistency is soft, with significant pressure from the probe, the elements of the lupoma rupture, causing pain and bleeding. Lupomas often merge. Their surface is smooth and shiny. If you press a glass slide onto the affected area, the lupomas become the color of “apple jelly” (apple jelly symptom). With a favorable outcome, resorption begins in the center of the tubercles and replacement of the damage with thin skin in the form of tissue paper.
Rice. 5. Photo of lupoma.
Rice. 6. Symptom of “apple jelly” in tuberculous lupus
Rice. 7. Lupus vulgaris.
Rice. 8. Consequences of Lupus vulgaris.
Forms of tuberculous lupus
Tuberculous lupus of the mucous membranes
The most severe form of Lupus vulgaris. The disease affects the mucous membranes of the nose, eyes and mouth. Initially, red-yellow formations (plaques) appear on them. Their surface has a grainy appearance, reminiscent of fish eggs. Over time, the process affects the cartilage of the nose and ears. Next comes spontaneous rejection of damaged dead tissue, which ends in permanent facial disfigurement.
Rice. 9. The photo shows a lesion of the tongue due to tuberculous lupus.
Rice. 10. Damage to the oral mucosa.
Tumor form of tuberculous lupus
Tuberculous tubercles merge, forming a tumor-like formation up to 3 cm in diameter. As the process progresses, a breakdown of the underlying tissue appears, accompanied by damage to the cartilage and lymph nodes.
Rice. 11. The photo shows a tumor form of tuberculous lupus.
Flat form of tuberculous lupus
Tuberculosis foci merge, but the affected area does not protrude above the level of the skin. As the disease progresses, ulcers appear with uneven edges and a granular bottom.
Rice. 12. Flat shape of Lupus vulgaris.
Psoriatic form of tuberculous lupus
Tuberculosis foci merge. The surface of the damage is covered with many small scales.
Rice. 13. Psoriatic form of Lupus vulgaris.
Rice. 14. Psoriatic form of Lupus vulgaris.
Exfoliative (scaly) form of tuberculous lupus
Tuberculosis foci merge. The surface of the damage is covered with many large whitish scales, which adhere tightly to the underlying tissues. The appearance of the lesion resembles a butterfly.
Rice. 15. Exfoliative (scaly) form of Lupus vulgaris.
Rice. 16. Exfoliative (scaly) form of tuberculous lupus.
Rice. 17. Exfoliative (scaly) form of tuberculous lupus.
Sarcoid-like form of tuberculous lupus
Merging, tuberculosis foci form tumor-like formations of a reddish color - lupus carcinoma. The process is prone to malignancy.
Classification of types of oral tuberculosis
Oral tuberculosis is a disease that appears and develops mainly in patients with reduced immunity. The disease is caused by Koch's bacillus. The source of inflammation located in the patients' oral cavity is secondary in most cases. It develops as a result of the spread of infection from the main focus, and spreads through the circulatory or lymphatic systems. In the case when the patient is affected by the pulmonary form of tuberculosis, the infection spreads to the oral cavity due to the penetration of mycobacteria contained in the sputum.
There are four forms of oral tuberculosis. Among them:
- Primary tuberculosis of the oral cavity. Transmitted by the respiratory or fecal-oral route, this disease almost never occurs in adults. Most patients with this diagnosis are infants.
- Tuberculous lupus. It is the lupus form of oral tuberculosis that is most often encountered in dental practice. Erosive elements are localized on the mucous membrane of the gums. If treatment is not started on time, these tumors can develop into a malignant form.
- Miliary-ulcerative form. This form usually develops in patients who have already been weakened by tuberculosis. Along with their cough, they produce sputum, which is a source of bacteria that cause oral tuberculosis. The lesions are on the palate and tongue, in rare cases - in the area of marginal gums or on the side of the cheek.
- Scrofuloderma. This form of the disease is diagnosed in most cases in children. The clinical signs of scrofuloderma are somewhat different from those of other forms of oral tuberculosis. In the first stages - the appearance of not a tubercle, but a rather large nodule. After its softening and necrosis occurs, the stage of formation of fistula tracts begins. The healing process of the surface of the resulting ulcers takes a long time, and after it characteristic fringed scars form.
Colliquatic cutaneous tuberculosis (scrofuloderma)
After tuberculous lupus, this form of skin tuberculosis is in second place in terms of frequency of the disease. It got its name from the Latin scrofulae - swollen lymph nodes of the neck and colliquescere - to melt. MBT enter the skin from infected lymph nodes through the lymphatic ducts. Cracks and ulcerations appear above the area of enlarged lymph nodes. The process is localized on the lateral parts of the neck, chest and collarbones. Young women are predominantly affected.
Symptoms of the disease
At the beginning of the disease, dense, painless nodules appear, which quickly increase in size, forming nodes tightly fused to the underlying tissues. Their sizes range from 3 to 5 cm. The skin over the lymph nodes acquires a bluish tint. Over time, the node becomes soft and opens. A cold abscess forms (suppuration without any manifestations of an inflammatory reaction). Pus with blood clots and pieces of destroyed (necrotic) tissue begins to be released from the fistula tracts. The ulcer has soft edges. The bottom of the ulcer is covered with a yellowish coating. Numerous granulations are visible. As the ulcer heals, irregularly shaped scars appear, which are connected by jumpers and bridges. The top of the scars is covered with papillary processes.
Rice. 18. Scrofuloderma.
Rice. 19. Scrofuloderma.
Rice. 20. Scrofuloderma.
How is tuberculosis diagnosed?
To diagnose the disease, you must first consult with your primary care physician, who, if tuberculosis is suspected, will refer you to a phthisiatrician (tuberculosis specialist) for further diagnosis and treatment. Diagnosis will depend on the type of disease.
Diagnosis of pulmonary tuberculosis
An X-ray of the chest is required, which provides an image of the lungs. For pulmonary TB, the scan should show changes in the appearance of the lungs, such as scarring.
To confirm the diagnosis, samples of mucus and sputum are taken and analyzed under a microscope for the presence of tuberculosis bacteria.
Examination for extrapulmonary tuberculosis
- CT scan
- magnetic resonance imaging (MRI)
- ultrasound examination (ultrasound)
- blood tests
- Analysis of urine
- biopsy - a tissue sample is taken from the affected area to be tested for the presence of tuberculosis
Examination for latent tuberculosis
To prevent the disease, every person is required to undergo fluorography and an X-ray of the lungs at least once every two years.
Ulcerative skin tuberculosis (Tuberculosis cutis ulcerosa)
The disease most often affects men who already had tuberculosis of internal organs. Tuberculosis bacilli enter the skin from the urine, feces or sputum of the patient himself, affecting areas of natural external openings: the skin around the anus, glans penis, nose, area around the mouth, mucous membrane of the tongue.
Symptoms of the disease
Merging, tuberculous tubercles form small yellowish nodules. Over time, the nodules suppurate and open with the formation of painful ulcers that make natural acts difficult.
The ulcers have soft, undermined edges. The color of the ulcers is pale red. The size of the ulcers is up to 1.5 cm, the bottom is granular. Javas often bleed. Sharply painful. As the disease progresses, tuberculous tubercles reappear at the bottom of the ulcers and around them. The tissues are destroyed, forming yellowish microabscesses, the so-called “Trel grains”, containing a large amount of MBT. The disease is difficult. Ulcers heal slowly. In their place, thin scars form, located below the skin level (atrophic scars).
Rice. 21. Ulcerative tuberculosis.
Warty skin tuberculosis (Tuberculosis cutis verrucosa)
Warty skin tuberculosis occurs among veterinarians and slaughterhouse workers who come into contact with the corpses of animals with tuberculosis. This form of the disease is rare. The skin of the back of the hand or feet is affected. The skin of patients is affected by tuberculosis from constant contact with infected sputum.
Symptoms of the disease
First, tubercles appear, the skin above which becomes bluish in color. Gradually, the tubercles merge with each other, forming dense infiltrates of a bluish color. Over time, they become covered with warty growths, dense scales and cracks. The lesion is surrounded by a bluish-red shaft, followed by a zone of shiny skin. During the healing process, the horny masses are rejected, and scars appear at the site of infiltration. The course of the disease is long-term.
Symptoms and first signs of tuberculosis in children
First of all, tuberculosis in children is manifested by such clinical signs as:
- weakness;
- stopping weight gain;
- irritability;
- fatigue during school hours;
- absent-mindedness;
- lagging behind peers in studies;
- body temperature – up to 37.5°C;
- enlarged lymph nodes;
- sweating;
- chills.Source: N.M. Koretskaya Tuberculosis in children and adolescents in modern conditions // Siberian Medical Review, 2010
Forms of tuberculosis and early signs
| Form | Symptoms |
| Tuberculosis of the bronchial glands | Cough, elevated body temperature for a long time, lethargy, fatigue, pallor, thinness. |
| Pulmonary form | Cough, shortness of breath, weakness after sleep, apathy, decreased performance, absent-mindedness, unhealthy blush, thinness, pale skin, sweating, chills, dry (and then “wet”) cough for more than 3 weeks, sputum with blood. |
| Lymph node involvement | An increase in the size of the lymph nodes, their softening, suppuration (the contents leak out), the formation of fistulas in places where pus comes out, scrofuloderma (skin lesions in the form of tumors with subsequent release of the contents). |
| Involvement of bones and joints in the process | Slow development, pain when moving, changes in gait, lameness. |
| Damage to the meninges (tuberculous meningitis) | Anxiety, lethargy, loss of appetite, bad mood, headaches, fever, vomiting, convulsions. |
| With damage to the gastrointestinal tract | Constipation or diarrhea, increased body temperature, blood in the stool, pain. Source: A.V. Mordyk, E.A. Tsygankova, L.V. Puzyreva, A.A. Turitsa Tuberculosis in children of the Russian Federation at the present stage // Pediatric pharmacology, 2014, v. 11, no. 3, pp. 27-30 |
Clinical manifestations by age of children
| Age | Symptoms |
| Infancy (up to one year) | Low mobility, apathy, weakness, attacks of suffocation or coughing, retraction of part of the chest, weight loss (including muscle mass), loss of appetite, cessation of crying, insomnia. Early detection and diagnosis are extremely important, because at this age this pathology is most dangerous. |
| 5-8 years | Decreased activity, weakness, lack of sleep and appetite, loss of body weight, cough, condensation of the chest. |
| 8-15 years | Rapid appearance of pain in the lungs against a background of apathy and weakness, active urge to cough, shortness of breath even at rest, thinning or discoloration of the skin, the appearance of cracks, wounds, hemoptysis, changes in lymph nodes in size and structure, intoxication of the lungs (at the last stage) . |
Manifestations of the chronic form:
- sleep disorders;
- liver enlargement;
- lagging behind peers in physiological development;
- dry and pale skin;
- mild euphoria.
Papulonecrotic tuberculosis of the skin (tuberculosis cutis papulo-nectrotica)
Papulonecrotic tuberculosis of the skin is more often recorded in young people. The disease is manifested by the appearance of papules, the size of which does not exceed 3 cm in diameter. The skin of the buttocks, abdomen, extensor surfaces of the limbs and chest is affected. The skin over the papules becomes pinkish-bluish in color. Over time, the papules become ulcerated. At the site of the ulcers, a grayish-white crust appears, which is replaced by a whitish scar.
Rice. 25. Tuberculosis cutis papulo-nectroticа. Multiple bluish-purple infiltrates and nodes on the legs.
Rice. 26. Papulonecrotic tuberculosis of the skin of the legs. Multiple bluish-purple infiltrates and nodes on the legs.
Rosacea-like Lewandowski tuberculosis
This form of the disease occurs as an allergic vasculitis. Erythema (redness) and telangiectasias (numerous dilated small vessels) appear on the skin of the face. Gradually the skin acquires a bluish-reddish tint. Rashes (tuberculids) are dense formations up to half a centimeter in diameter, without necrotic elements. During healing, atrophic scars form at the site of tuberculides.
Rice. 27. The photo shows Lewandowski’s rosacea-like tuberculosis.
Treatment of oral tuberculosis
Treatment of this form, like all others, is carried out in specialized institutions - tuberculosis dispensaries. First of all, the underlying disease is treated. To prevent the bacterial infection from spreading further, antiseptic baths are prescribed.
After the acute condition has been relieved, it is necessary to take care of timely and high-quality sanitation of the oral cavity. It is important to promptly consult a specialist at the first symptoms: advanced oral tuberculosis leads to serious consequences for the patient’s health.
Lichenoid tuberculosis of the skin (Tuberculosis cutis lichenoides seu lichen scrofulosorum)
Lichenoid tuberculosis of the skin often develops in weakened children, less often in adults with tuberculosis. The disease is manifested by the appearance of tubercles, which are covered with light gray scales. The tubercles are located symmetrically, most often on the skin of the abdomen and limbs. After healing, pigmentation or small scars remain at the site of the rash.
Rice. 28. The photo shows lichenoid tuberculosis of the skin.
Indurative tuberculosis of the skin (indurated erythema)
This form of the disease manifests itself in 2 varieties - Bazin's erythema nodosum and Hutchinson's ulcerative erythema. The disease often affects patients with tuberculosis of internal organs.
Erythema nodosum of Bazin
The disease is more often registered in women aged 16 to 40 years. Dense nodes or flat, extensive infiltrates that appear on the skin of the legs, thighs, buttocks and upper extremities are bluish-red in color. The size of the seals is 3 – 8 cm. Seals and infiltrates are often located symmetrically, in the deep layers of the skin and subcutaneous fatty tissue. With regression of tuberculous elements, ring-shaped atrophic areas and pigmentation remain.
Hutchinson's ulcerative erythema
Sometimes the lesions merge, forming an extensive lesion with ulcerations in the center and dirty gray granulations. This form is named after the English dermatologist who first described it - Hutchinson's ulcerative erythema. Without treatment it lasts for a long time, sometimes even years. After healing, sunken pigmented scars remain.
Rice. 29. The photo shows indurative tuberculosis of the skin (indurated erythema of Bazin).
Rice. 30. Ulcerative erythema of Hutchinson.
Types and forms of pathology
According to the period of occurrence in medicine, stages are distinguished:
- infiltration;
- decay;
- contamination;
- resorption;
- seals;
- the appearance of scars;
- calcification.
| Form | Peculiarities |
| Chronic and early | It occurs against a background of body temperature up to 40℃, cough, pain in the lungs, uneven breathing, wheezing, decreased appetite, and loss of strength. |
| Respiratory damage | Includes pathologies:
|
| Other localizations | There may be lesions:
|
Diagnosis of skin tuberculosis
Rice. 31. View of Mycobacterium tuberculosis in the light of a fluorescent microscope.
The diagnostic process consists of the following components:
- Bacteriological diagnosis (detection of MBT in discharge from ulcers and lymph node punctures).
- Diagnostic biopsy followed by histological examination, which allows to identify the morphological components of the tuberculous tubercle.
- Detection of tuberculosis of internal organs.
- Detection of scars on the skin as a result of a previous tuberculosis lesion.
- Tuberculin diagnostics.
- Trial treatment.
Diagnostic biopsy together with bacteriological examination is the most significant method in diagnosing tuberculosis.
Dermatologists are prescribed to detect skin tuberculosis. Knowledge of risk groups, which include patients in this category, early symptoms of the disease and diagnostic methods helps doctors to detect the disease in a timely manner.
Identification of the pathogen in the early stages of the disease will allow the patient to be successfully cured.
Diagnostics
Primary tuberculosis of the oral cavity is diagnosed during an external examination. Thus, it is characterized by the presence of lacerations and ulcers in the corners of the mouth with yellow, gray and bluish layers. Areas with ulcers tend to gradually enlarge.
At the same time, the lymph nodes begin to enlarge.
Diagnosis is carried out on the basis of the collected anamnesis, as well as using histological and bacterioscopic studies. During examination, dense painful lumps or ulcers are found on the mucous membrane, depending on the severity of the condition.
There is minor inflammation. The process of formation of adhesions begins between the lymph nodes and the surrounding surface.