Possibility of unforeseen consequences
Laser correction of moles is one of the safest ways to get rid of nevus, avoiding complications and unforeseen consequences. A beam of directed light radiation literally evaporates the pigmented cells of moles, which is visually manifested by the complete removal of the epidermal formation in just a few minutes. Minimization of negative consequences occurs due to the following objective factors.
- The laser beam acts in a strictly targeted and selective manner, without injuring healthy skin structures, which allows the technique to be used even to remove the smallest nevi in the eyelid area and mucous membranes;
- There is virtually no risk of infection, since the laser exhibits a powerful antibacterial and antimicrobial effect, protecting the wound surface from infection;
- Laser destruction is not accompanied by bleeding or hemorrhage, since during the manipulation process all blood capillaries supplying the body of the mole undergo thermal coagulation;
- The laser activates regenerative processes in the skin, which significantly accelerates wound healing;
- The technique is low-traumatic, which avoids the formation of connective tissue and all the negative consequences associated with this factor.
Despite the safety of the method, it should be borne in mind that before the procedure it is necessary to carefully study the list of contraindications, since the consequences and complications of laser correction most often result from neglect of this list, which includes the following conditions:
- Pregnancy;
- Acute infectious process;
- Oncology of any localization;
- Inflammation in the intended area of laser exposure;
- Period of menstruation in women;
- Immunodeficiency;
- Exacerbation of chronic pathologies;
- Hyperthermia.
When deletion is indicated
Epidermal nevi are benign formations and are harmless to health. However, any nevus carries a potential threat; there is a possibility of degeneration into a malignant tumor - melanoma. This is one of the most dangerous types of cancer. Therefore, it is important to monitor existing moles and consult a doctor if there is the slightest change.
You should visit a dermatologist as soon as possible in the following cases:
- the mole has increased in size, changed color, shape, outline;
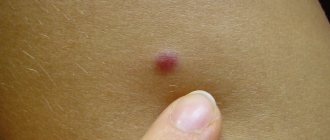
- pain, itching, bleeding, burning, peeling, ulceration appeared, the surface became lumpy and uneven;
- the nevus was injured.
There is a high risk of degeneration for nevi located in open areas of the body. This is due to intense exposure to ultraviolet rays during the hot season. Also subject to removal are nevi that are constantly injured by elements of clothing - the handle of a bag, a collar, elastic bands of underwear, etc. Those formations that are located on the hairy areas of the body are also at risk - there is a possibility of tissue damage during shaving, waxing or sugaring.
Current issues
Most patients, after undergoing a laser mole removal procedure, observe some characteristic reactions of the body during the first two weeks, some of which are normal responses that are compensatory in nature. Let's consider several pressing issues regarding the consequences of removing nevi on the face and body.
Can cancer occur after mole removal? Skin cancer, or melanoma, usually develops as a consequence of the malignant transformation of a melanoma-prone mole. Moreover, if during the laser correction process the specialist incorrectly determined the required depth of the beam and did not completely remove the mole, the risk of developing melanoma increases.
After removal, a tubercle appeared. Despite the low-invasiveness of the technique, in the process of removing the nevus, healthy surrounding tissue remains, which will have to undergo the healing process of the wound surface that has formed in place of the mole. In this case, this zone can form a small tubercle, which will be covered with a dense crust in a few days. This is considered a normal reaction to manipulation.
Inflammation after removal of a birthmark. The inflammatory process after laser correction usually lasts for the first days, after which it goes away. If inflammatory signs persist for a long time, you must immediately contact the specialist who performed the procedure.
Can a scar or scar form after removal of a nevus? The formation of scars can only be observed in the case of forced premature removal of the protective crust from the wound surface.
The scar itches and hurts after mole removal. Itching, burning, peeling and redness around a mole after removal are characteristic symptoms of a burn, which can be caused by unprofessional work of a doctor. This unpleasant complication develops if the specialist incorrectly determined the depth of exposure and subjected healthy skin cells to laser burning.
Stages of healing
The first stage of healing lasts the first seven days, during which the crust gradually darkens and becomes more rigid. You should never touch it, as it protects the wound from infection and promotes the appearance of new healthy tissue. In the first week after the procedure, the operated area should be protected from any injuries and damage; it should not be covered with clothing too often, wetted with water or rubbed with a washcloth, scratched or applied with any cosmetics.
The use of disinfectants is allowed if they have been prescribed by a doctor. You can also treat the crust with a mild solution of potassium permanganate.
The next stage of healing includes the second week after surgery. During this time, the dark crust at the site of the former mole disappears on its own, and light pink skin remains instead. It is still recommended to protect this area from any excessive exposure as well as ultraviolet rays. To this end, it is worth reducing the time spent in the open sun, as well as treating the skin with sunscreen with a maximum protective factor (about SPF 50). Young skin can become significantly pigmented when exposed to the sun, especially on the face.
The final stage of recovery lasts 14 to 20 days after surgery or more. By this time, completely healthy skin has formed at the site of the removed mole, which has protective factors from ultraviolet radiation and other external influences, including mechanical ones. A slight itching may persist, which can be relieved with soothing ointments. Otherwise, skin surface care is no longer required.
If a hole remains at the site of the removed lesion, do not worry: usually the skin smoothes out on its own over the next 1-2 months.
Care after laser mole removal
If the laser ablation procedure was performed by a qualified specialist, the risk of side effects is minimal, but the patient will also have to follow certain post-procedure rules, listed below.
- It is necessary to provide rest to the wound surface, without injuring it by friction of clothing or shoes, and also by taking care of the protective crust;
- Contact of the wound with water should be avoided for two weeks after manipulation;
- It is recommended to protect the skin surface from direct sunlight, and also use creams with a high UV protection factor. To the question of when you can sunbathe after removing a mole, the answer will be at least three weeks;
- You cannot use ointments, creams and gels for healing on your own without a doctor’s prescription;
- The procedure area should be protected from any mechanical damage, carefully protecting the integrity of the protective scab.
Laser removal is one of the simplest and least traumatic methods of mole destruction. Compliance with simple rules of rehabilitation will allow you to avoid scars, cicatrices and other unpleasant consequences and obtain an ideal physiological and aesthetic result.
Selecting a removal method
So, an oncologist or dermato-oncologist recommended removing the mole, or you decided to get rid of the formation. Consult with a specialist which removal method is best for your situation.
In many cases, histological examination of a removed mole is a mandatory procedure. It is important to evaluate the structure of the nevus tissue and make sure that the formation is truly benign and that nothing threatens your health. In this case, traditional mole removal with a scalpel is one of the most suitable methods. Some modern instruments do not leave a trace of tissue, so it will not be possible to study them in the laboratory.
If a large mole is located on the face or open areas of the body, discuss with a specialist the prospects of using a laser or radio wave removal method. These methods have fewer cosmetic consequences - they do not leave noticeable scars, so it is often advisable to resort to them. Remember that health is more important - if the doctor insists on conventional surgical removal, you should listen, because the prevention and early diagnosis of cancer depends on this.
Scenario three – a mistake by the pathologist
A mole was removed; according to histology, it was a nevus, but skin cancer developed at the site of removal.
It is human nature to make mistakes - this was noted by the ancient Romans. Doctors are people too and can make mistakes too. Neither a therapist, nor a surgeon, nor even a pathologist is immune from mistakes. What can a doctor do to avoid mistakes? If in doubt, consult with colleagues. If necessary, from other institutions. Unfortunately, not all laboratories have the technical capabilities for this.
How to avoid becoming a victim of the third scenario?
- Be careful when choosing a laboratory.
- If there are any doubts about the result of the study, take the material and take it for review to another laboratory, or even two others. Don’t be afraid to send it to laboratories in the capital by courier.
You might be thinking, “How terrible! You can't trust anyone and you can't be sure of anything! There’s no way I’m going to remove a mole that bothers me so much, it’s better and safer to deal with it...”
Don't give in to neurosis. Human error can lie in wait anywhere, and you can never be 100% immune to it. The laboratory doctor may do the analysis incorrectly, and we will not know that we are sick and will not begin timely treatment. A radiologist or ultrasound doctor may make a mistake when conducting a study, and the consequences of such a mistake will also be very sad. A builder can drop a brick on our head, a car can hit us on the street - there are a huge number of chances to go to another world. However, it is not worth developing hypochondria and depression on this basis, because if you follow the logic of maximum reinsurance to the end, it is better to stay at home and never go out J
Where to remove a mole?
You can remove a mole at any of our cosmetology centers.
On the day of treatment, after consultation with a cosmetic surgeon, in the absence of contraindications, the procedure can be performed; in this case, the consultation will be free for you
You can consult a doctor and have a mole removed by first making an appointment by calling
+7
Mon-Fri: 9:00-20:00, Sat: 9:00-18:00
Sign up for a consultation
General characteristics of formations
A mole is a pigment formation of one of the shades of the brown palette. The base contains melanin and the melanocyte cells that produce it. Melanins are high molecular weight pigments. They are characterized by a heterogeneous structure and complex chemical composition. Pigments are found not only in moles, but also in all skin, hair, iris, inner ear and even some parts of the brain.
Content:
- General characteristics of formations
- Indications/contraindications for the procedure
- What you need to know about melanoma?
- How to properly prepare for mole removal
- Technique of the operation
- Possible complications and side effects
- Features of rehabilitation
It is important not to confuse nevi and birthmarks. Moles do not form in the prenatal period, but as a person grows older and are closely related to his lifestyle. The cause of the formation of pigment spots can be a hereditary factor, exposure to ultraviolet radiation, or hormonal changes.
Each mole is a separate formation with a unique life cycle. At first it is a flat spot, which can increase and rise slightly above the skin as it grows and develops. The size and location of the formation depends on the level of melanocytes. If they are in the epidermis (top layer of skin), the mole will be flat. The deeper the melanocyte is immersed in the dermis, the higher the formation is located on the surface of the human body.
Convex nevi, which rise slightly above the skin, should not frighten their owners. This condition has no negative consequences and is considered a variant of the norm. The main thing is that the mole is miniature, round and uniform (in terms of color and structure) throughout its life cycle.
Can a mole disappear on its own and how safe is it? Yes, the formation can disappear without the influence of mechanical factors. This happens gradually and can alert a person. First, a white outline is formed around the formation, which resembles an orbit. This contour begins to increase and gradually covers the surface of the entire formation. The nevus disappears, and a small white spot remains in its place. Most often this occurs after severe sunburn. The disappearance of moles can also be a harbinger of the rare disease vitiligo.
If you notice changes in a mole (increase/decrease, uneven edges, change in shade or structure), be sure to consult a specialist.
Preparing for the intervention
No preparation is required for surgery: you can eat and drink water without restrictions, and you do not need to take medications. However, it is important for women to plan the day of surgery taking into account the menstrual cycle; it is better to do this after menstruation. The recommendation applies to any surgical intervention. Also, in cases where the nevus is located on open areas of the body, it is better to remove it from October to April. This will eliminate the need to hide the wound and protect it from ultraviolet rays.
If you are taking medications that affect blood clotting, tell your surgeon. You should not stop taking medications on your own—check with your doctor.
Indications/contraindications for the procedure
The surgical method is most often used when malignant degeneration of a nevus is suspected. Doctors recommend removing formations that are constantly in contact with clothing or located on the scalp, which increases the risk of damage. Moles in the groin, neck, chin, back or in the folds of the skin are most often damaged - consult a dermatologist to decide whether to remove them. Large formations on “legs” also pose a colossal danger. They can come off or become twisted, which can cause pain and infection.
Excision covers not only the affected area, but also healthy tissue, which prevents recurrence of skin growths. The main advantage over more modern laser removal or cryodestruction is the obtaining of material for histological examination. The excised tissue is sent for diagnostics in order to better understand the causes of the disease, understand the possible risks and create a preventive course for the patient.
Surgical procedures can only be performed in specialized medical institutions. Beauty salons or home procedures are not suitable for this and can cause irreversible consequences for the body.
| Indications | Relative contraindications |
| Increasing the size of education | Infectious diseases regardless of stage |
| Deep penetration of the mole under the skin | Acute inflammatory processes |
| Bleeding, change in color or texture | Chronic pathologies in the acute stage |
| Frequent injury to the mole, the formation causes pain or inconvenience | Pregnancy and breastfeeding period |
| Aesthetic discomfort |
There are no direct contraindications to surgical removal of nevi. In case of relative contraindications, the patient must undergo additional tests and consult a specialist.
The doctor will determine the advisability of removal, indicate possible complications and features of rehabilitation. In some cases, surgery will have to be postponed until the patient fully recovers.