Lumps, formations and other growths on the toes can appear at any time. If in winter and in the off-season they are practically invisible, then in summer the situation is different. In hot weather, this problem also becomes cosmetic. What could be growths on the toes, and how to get rid of them?
The growths can be a skin problem, or they can also appear as a result of diseases of the musculoskeletal system or other diseases, most often associated with metabolism. It is very important to diagnose formations correctly and timely. Only a specialist can do this correctly.
The same causes can have different types (this, for example, can be said about warts). And even more so, you should not prescribe medications or perform procedures that are not prescribed by a doctor, especially when it comes to a child.
Hallux valgus
In fact, it’s not even a growth, but a protrusion of the big toe, or a violation of the anatomy of the foot. In other words, this is an acquired skeletal deformity. For what reasons does this disease appear? It could be:
- Tight, uncomfortable shoes. When the foot remains in an uncomfortable position for a long time, the bones begin to shift so that they take on shapes similar in shape to a pair of shoes.
- Increased load. Most often we are talking about athletes. The risk group includes people who professionally lift weights (bodybuilding, weightlifting) or who have prolonged activity on their feet (dancers, football players). Increased load on the forefoot is also present in those women who prefer to walk in high heels. A pair of shoes leads to such consequences if the heel is over 5 cm.
To correct the situation, you first need to eliminate the source, the cause of this condition. Of course, few people will decide to give up professional training, but you can temporarily limit the load. If it's all about the shoes, then you need to replace them with anatomically correct ones. By the way, it is absolutely not necessary to buy shoes in specialized stores, because they cost a lot of money there.
It is enough to purchase special correctors. They can be made of plastic or silicone and are inserted into shoes from the inside. Such correctors fix the finger in the correct position and evenly distribute the load. They should be worn for a long time, several months.
Over time, the arch of the foot will acquire its previous correct shape. Most likely, the patient will be prescribed a course of anti-inflammatory or painkillers, since hallux valgus is usually combined with other diseases (bursitis, arthrosis, etc.).
Dermatofibroma
This formation, unlike the previous one, has a solid structure. It often appears on the top of the fingers, on the back side. To diagnose it yourself, just try to collect a patch of skin in this place. If a dermatofibroma is present, the skin will pull inward into a fold.
Normally, this area of skin has a darker reddish tint. If the dermatofibroma grows to a large size, then in the center you can clearly see a tubercle, more solid in structure than the entire formation.
Causes of dermatofibroma:
- insect bite;
- untimely opened boils;
- penetration of foreign objects into the thickness of the skin.
Its main danger is that it has the ability to degenerate into dermatofibrosarcoma, and this is an oncological diagnosis with all that it implies. And, of course, it causes a lot of inconvenience to a person, preventing him from leading a normal active life. It is almost impossible to treat dermatofibrosarcoma at home.
The thing is that this formation lies deep under the thickness of the skin layers. It is most reliable to remove it using the traditional surgical method.
Warts
These benign formations appear on the toes quite often, but mainly in those individuals who have weakened immune systems. They look like calluses, but they are hard inside. And also on the top of warts you can see dark dots, these are dead blood vessels. Warts are not as harmless as they seem. This is not a simple cosmetic defect that prevents a person from wearing open shoes.
Warts cause severe pain when walking if there is friction between the skin and shoes. In the area of the fingers this happens extremely often. This can be observed especially often if the formation is located under the thumb or second finger. A person’s gait changes, and he intuitively tries to shift some of the load to other parts of the foot.
Sweating and elevated temperature only aggravate the situation and help in activating the human papillomavirus, which became the source of such formation on the toes. Pain and discomfort while walking lead to a change in a person’s gait, and this is a serious reason to immediately consult a doctor.
In addition, constant friction against this growth leads to microtraumas of the skin, and the epidermis becomes wounded and more permeable to many pathogens from the external environment. In addition to warts, a person may soon encounter fungi and streptoderma. If a wart appears near the nail, in the area of its base, then it can affect the size and shape of the nail and affect the rate of its growth.
Warts are treated in a specialized cosmetology office. You can choose the cryodestruction method, wave technique or laser. In some cases, if the location of the wart allows, it is removed surgically. The difficulty is that you need to completely remove the growth particles from the skin. Otherwise, after some time the wart will grow back.
There are also traditional methods of removing warts, which are no less effective. The most popular method is to periodically smear this area with fresh celandine juice. The juice should dry on its own. After two weeks of this therapy, the wart will dry out and begin to fall off. You can also use vinegar. Both regular and apple cider vinegar are suitable for these purposes.
You need to soak a cotton swab in vinegar and wipe the wart with it. You cannot pour vinegar directly onto the formation! This may cause skin burns. To prevent the growth of warts, it would be useful to take a course of antiviral drugs, but only a therapist should prescribe them. It is not always possible to cure warts completely. It is important to monitor your immunity, because this is the only way to prevent the activation of the virus.
Treatment of exostoses of fingers and toes
To relieve pain and inflammation, patients are prescribed drug therapy. It is selected individually depending on the complexity of the situation and the nature of the patient’s chronic diseases. Most often, NSAIDs are prescribed in the form of ointments, gels, creams or oral forms. But their use does not lead to the resorption of the osteochondral growth, but only helps to eliminate the symptoms.
The only effective way to treat exostosis of the phalanx of the finger is surgery. It is shown when:
- large amounts of exostosis;
- finger deformities;
- persistent pain syndrome;
- the development of complications or the appearance of signs of malignancy.
The operation is not technically difficult and can even be performed under local anesthesia. They mainly resort to the method of marginal resection of the tumor. It involves making a transverse incision in the projection of the bone growth. Its magnitude depends on the size of the formation, but is usually on the order of several millimeters. The soft tissue is carefully separated from the bone to obtain a clear view of the exostosis and accurately determine its boundaries.
After this, using a surgical chisel or other instrument, the growth is carefully removed within healthy tissue. It is important for the surgeon to completely remove the entire tumor along with its cartilaginous cap, since otherwise there is a high risk of relapse. The surgical wound is actively washed with saline to wash out the smallest bone particles, and only then is it sutured and covered with a sterile bandage.
If a patient is diagnosed with deformity of the phalanges of the fingers, a corrective osteotomy is indicated. The operation involves not only removing the osteochondral exostosis, but also cutting the bone, followed by juxtaposition of the resulting fragments in such a position that the phalanx acquires an anatomically correct shape. The bone is fixed with special metal systems in a given position, after which the wound is sutured and covered with a sterile bandage.
Calluses
On the foot, they most often appear in the area of the heel and toes, that is, exactly where the skin rubs when walking. The appearance of calluses in the toes most often indicates increased stress on the forefoot. It can be assumed that the patient likes to wear high heels.
Wet calluses cause a lot of problems. The skin in this place stings and aches. Walking normally and even standing is very painful. It is especially dangerous if the contents of a wet callus are revealed. Where a sufficient layer of new skin has not yet formed, increased tissue permeability is observed. Pathogens from the external environment can enter the bloodstream.
Treatment of calluses involves applying an antiseptic patch. It is advisable to periodically remove the patch to allow the callus to dry out. If calluses appear periodically, from time to time, then most likely the problem is the wrong shoes, and they need to be replaced.
Corns
Most often they appear on the big and index toes - on the side, below or between the toes, since this is the area on which a person usually leans when walking. Corns can be described as a collection of dead skin, in this case the fingertips. Removing corns at home in one go is quite difficult.
To properly get rid of several layers of skin, use the following methods and recipes:
- Gels, creams and ointments. They can contain various components, most often natural acids, which help soften rough layers of skin. After several such applications, all that remains is to remove the soft cells. Such creams may also contain antiseptic components.
- Special patches. The simplest ones are based on salicylic acid. It must be applied strictly to keratinized skin. When applied to normal areas of the skin, the patch can lead to softening and, as a result, disruption of the integrity of the skin.
There are also homemade ways to soften dead skin in order to subsequently remove it:
- Lemon. You need to cut off a slice of lemon and apply it over the corns overnight. In a few hours, the keratinized skin will soften. The number of treatments that may be required depends on the thickness of the corn. On average, up to 5 such procedures may be required.
- Vodka compress. It is necessary to moisten a piece of cotton wool with vodka, apply it to the corn, fix it, cover it with film, put on a woolen sock and leave it in this state for several hours. During this time, the skin will soften, and it will be easy to remove with ordinary pumice.
Keratomas
Keratoma is a benign neoplasm on the skin; it appears as a result of an imbalance in the constant renewal of skin epithelial cells. For some reason, the epidermis cannot independently get rid of old dead cells, but new ones have already been formed. Because it is made up of keratinocyte cells (the normal cells that make up skin), it is considered benign.
Such pathological processes are observed most often on the extremities, and therefore they can often be found on the toes. In approximately 8–20% of all cases, keratomas turn into cancer. How to diagnose keratoma yourself? At the initial stage, it looks like a slightly protruding spot of coffee or gray color.
If you touch it, you will notice that it is rough. Gradually, the elevation above the rest of the skin begins to increase, and now the growth is already visible to the naked eye. If the keratome rises too much, there is a danger of injury, which will lead to bleeding and pain.
Experts believe that keratomas on the fingers can be considered safe if they are in a stable condition. If a person notices their increase, darkening of color or bleeding for no reason, then an urgent need to consult a doctor. Removal of keratomas is carried out in different ways: radio waves, laser, liquid nitrogen, acids, electrocoagulation or the standard scalpel.
If there is a suspicion that an oncological process is occurring inside the keratoma, it can be removed only by radio waves, laser or traditional surgery. The remaining methods are considered weaker, gentler, and therefore, after using them, a person may subsequently experience rapid growth of cancer cells in this area. That is, the therapy itself will provoke the development of cancer.
Reasons for development
Exostoses of the fingers and toes may represent an osteochondroma, i.e., a benign tumor, or be a consequence of injury, chronic inflammation, or even prolonged wearing of tight shoes. The latter factors more often provoke the formation of exostoses in adults.
Osteochondromas are mainly typical for children and adolescents under 20 years of age. They can be single or solitary, as well as multiple. Solitary osteochondromas of the fingers and toes are a rare occurrence. More often, in the presence of exostoses with such localization, similar lesions of other skeletal bones are found, in particular the femur, tibia, humerus, spine, clavicle, etc.
The reasons for the formation of osteochondromas have not yet been fully established. It is believed that isolated neoplasms of this kind are a consequence of displacement of the epiphyseal plate. This may be due to disorders of embryonic development, radiation therapy at an early age, or exposure to other types of ionizing radiation. Epiphyseal plates are areas of bone growth that are made up of cartilage and are located directly under the “head” of the bone. Due to the fact that its cells are in the process of constant mitotic division, the child’s bones lengthen as they grow older. Subsequently, the cartilage cells located furthest from the epiphyseal plate ossify and form bone tissue.
If, due to the action of one factor or another, a fragment of the epiphyseal plate moves to the side, it continues to synthesize new cells, which also gradually ossify. This is how exostosis forms in children. Initially, it is represented only by cartilaginous tissue, but over the years it becomes dense and hard, but the cartilaginous cap remains. It usually grows in proportion to the rate of bone growth, and therefore is usually detected during puberty, when a sharp growth spurt occurs.
Multiple exostosis disease is considered to be a hereditary disease. Massive skeletal damage by exostoses is usually detected in early childhood and requires dynamic monitoring, since with it the likelihood of malignancy of neoplasms increases. Single exostoses become malignant in less than 1% of cases.
Hygroma
Hygroma is a lump that often appears on the phalanges of the toes, especially the big and little fingers. Inside the finger, with this benign formation, a capsule is formed with liquid contents inside (fibro-mucosal or fibro-serous fluid). Most often, the growth does not stand out much above the rest of the finger. It is stable, that is, it does not move, since it is closely connected to the tendon apparatus.
Such small hygromas may not cause problems to a person, and therefore many simply do not notice them. As the size increases, painful sensations appear, because the formation affects neighboring areas with nerve endings. If such symptoms are ignored, a person may experience limited mobility of the toe joints.
The most effective method of treating hygroma is puncturing it, that is, puncturing the area where the fluid is localized. This is usually combined with physiotherapeutic methods that restore blood microcirculation and improve local immune processes. In some cases, when a capsule with liquid has just formed, it may be reabsorbed on its own when the load on the foot is reduced.
Symptoms
In some cases, exostosis of the toe or hand is asymptomatic. If it forms on the side of the finger, it can cause manifestations of soft tissue hyperkeratosis. But since their volume is relatively small, a full-fledged callus is not formed. If you remove areas of thickened skin, the discomfort does not go away, and the tissues soon become keratinized again.
When exostosis reaches a large size, it injures soft tissues and provokes inflammatory processes in the joints. This leads to discomfort or even pain, especially when wearing tight shoes. It can also protrude beyond the physiological boundaries of the finger. When palpated, exostosis is a dense bony protrusion with a smooth or rough surface. This further aggravates the discomfort.
With active growth of the tumor, the phalanx may become deformed, as well as neighboring fingers. This already leads to the development of an aesthetic defect.
At a certain location, exostosis can compress the neurovascular bundle. The consequence of this is local swelling of the finger, a feeling of numbness or goosebumps.
The most common condition is exostosis of the big toe. This may be accompanied by valgus deformation of this finger, which is manifested by its deviation from the normal axis towards neighboring fingers. As a result, 2-3 toes may also become deformed, acquiring a hammer-like shape.
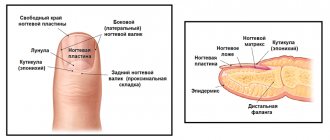
With subungual exostosis, there is a protrusion at the end of the phalanx of the finger, which looks like a thickened subungual ridge. In this case it is observed:
- pain when pressing on the nail, fingertip, or during physical activity;
- impaired nail growth, up to ingrowth or peeling;
- redness of soft tissues;
- callus formation.
Malignant growths
These reasons are extremely rare, but they should not be ruled out at all. Malignant tumors can form from any structure - bones, blood vessels, muscles, cartilage, ligaments. In the first stages, the growth of malignant tumors is very slow.
Then some provoking factor appears, and the tumor begins to progress rapidly. A growth on one toe quickly spreads to the entire phalanx, and this is far from the limit. Consultation, diagnosis and treatment of such patients should be carried out only together with an oncologist.
Diagnostics
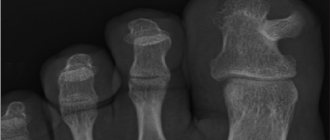
The appearance of signs of exostosis requires contacting an orthopedist-traumatologist. At the appointment, the doctor carefully examines the finger, palpates the growth and finds out the nature of the symptoms. If a dense bone formation is detected, an x-ray is indicated.
With its help, you can not only diagnose exostosis of the toe, but also evaluate its location and size. The images also provide data on the degree of deformation of the distal phalanges and allow you to plan the most effective course of treatment. In rare cases, CT and MRI are additionally prescribed.
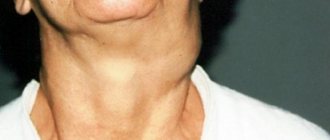
Tophi
A growth on the toe called a tophi is caused by gout. It is formed from crystals of uric acid salts. These nodules are bounded by connective tissue. Color – from white to light yellow. The skin over them differs from neighboring areas; it is rough because it is very poorly supplied with nutrients. The very appearance of tophi indicates a severe stage of the disease, as well as the duration of its course. This area hurts, not only when walking, but also at rest.
The appearance of growths on the toes should alert a person, because any external change is a reflection of internal processes. In most cases, formations should be removed because they interfere with a comfortable life, but only a doctor can make this decision.
Rehabilitation
The duration and complexity of the recovery period are determined by the type of surgery performed. After marginal resection, discharge can be carried out on the day of surgery, but patients are advised to limit physical activity for 2 days. Drug therapy is also prescribed to reduce the risk of developing infectious complications and eliminate pain. After 2 days, a dressing is required, the stitches are removed after 7-10 days.
When performing a corrective osteotomy, recovery is more complex and lengthy. It involves immobilization of the operated finger, which is necessary for the healing of an artificial fracture.
Thus, exostoses of the fingers and toes are a rare phenomenon, but can significantly reduce the level of physical activity, cause cosmetic defects, pain, and generally worsen the quality of life. The solution to the problem is only possible through surgery. In this case, the operation is usually simple and does not require complex recovery. The main thing is to contact an orthopedic traumatologist as soon as possible after signs of exostosis appear, before its active growth provokes deformation of the fingers.