Pityriasis versicolor or pityriasis versicolor is a superficial skin lesion caused by a yeast-like fungus of the genus Malassezia.
These microorganisms are representatives of typical skin microflora, are found in most people and do not cause the development of the disease. But under the influence of external or internal factors, the pathogen can transform from a non-pathogenic form into a pathogenic one: the fungus penetrates the upper layers of the skin and damages melanocytes - the cellular structures responsible for the pigmentation of the skin.
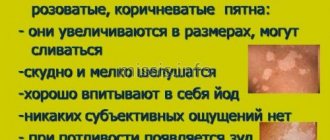
As a result, the patient develops small spots of different colors: from pale pink to red-brown, with noticeable peeling in the center. When touched, the scabs flake off easily and resemble flakes, which is what gives pityriasis versicolor its name.
What is pityriasis versicolor?
Pityriasis versicolor is a dermatological disease, most often diagnosed in people under the age of 30, while it is rare in children and the elderly. A predisposing factor to the occurrence of infection is often excessive activity of the sweat glands, so the disease often develops in the summer, at resorts and in countries with a humid, hot climate.
Lichen versicolor develops against the background of:
- chronic gastrointestinal diseases (gastritis, ulcers);
- endocrine disorders;
- autoimmune diseases;
- hormonal fluctuations, including those caused by taking oral contraceptives, pregnancy, infertility treatment;
- genetic predisposition.
Ringworm can be triggered by taking certain medications, for example, immunosuppressants, glucocorticosteroids. Uncontrolled drug therapy also often causes lichen.
A decrease in the body's natural defenses can also trigger the growth of fungal colonies.
This can lead to:
- recent serious illnesses, injuries or surgeries;
- severe vitamin deficiency;
- hypothermia of the body;
- stress;
- prolonged exposure to adverse factors (for example, work in hazardous industries, contact with chemicals and reagents);
- food poisoning;
- period of increased mental and physical stress;
- sudden climate change;
- alcohol abuse.
Among the external factors that cause tinea versicolor, wearing tight synthetic clothing in the hot season stands out. Artificial materials disrupt natural skin respiration, increase sweating, and irritate the upper layers of the skin. As a result, colonies of the fungus penetrate the epidermis and begin to actively multiply.
Mycozoral against lichen
Ketonazole in the drug actively fights against fungi, bacteria and microbes. Effective treatment is possible even when the skin is damaged by staphylococci, streptococci, dermatophytes or yeast fungi. Positive dynamics are visible on the second day of treatment.
When used correctly, it prevents the reappearance of pityriasis versicolor.
The drug has a number of serious side effects and contraindications. A medical specialist will recommend strictly adhering to the dosage. Use the ointment for no longer than seven days, apply a thin layer once a day. Children and pregnant women are prohibited from using the ointment. Does not affect the blood when applied topically.
For children, tablets are prescribed. The dosage is calculated based on the child's weight. It is acceptable to use a soap solution or shampoo for prevention. A cumulative effect is possible, so the doctor prescribes an individual dosage for any form of medication.
What does pityriasis versicolor look like?
The first symptom of the disease is the appearance of small spots, most often localized on the torso, arms, scalp or external genitalia. The rash may be accompanied by mild itching or may not cause the patient any noticeable discomfort.
The rashes do not have a sharp outline, are not inflamed and do not swell. Initially they are pink in color, but gradually change shade: from pink-yellow to brown and red-brown. The number of spots increases: the fungus spreads across the skin, occupying more and more surface area of the body. The rash may appear on the hands, legs, face, but never affects the mucous membranes, palms or feet, which is due to the special structure of the epithelium in these areas.
The rashes can increase in diameter (up to several centimeters) and merge with each other. Peeling zones appear in the center - when you touch the spot, the scales easily peel off. An atypical form of pityriasis versicolor includes pityriasis alba, in which the affected areas completely lose their pigment (become white). In this case, there may be no peeling.
A distinctive feature of pityriasis versicolor is a disorder of skin pigmentation. Fungal colonies damage melanocytes, which are responsible for the production of melanin, the substance responsible for the color of the skin. Areas of hypopigmentation are especially noticeable during tanning: the epithelium damaged by yeast remains white. This effect can persist for a long time even after recovery.
Pityriasis versicolor is prone to a chronic course and frequent relapses.
To quickly recover and avoid the unpleasant consequences of the infection, it is recommended to consult a dermatologist at the first symptoms of the disease:
- the appearance of a pink or reddish rash;
- mild itching of the skin;
- a feeling of tightness and flaking in certain areas of the skin of the torso and arms.
Symptoms of versicolor
The fungus can exist in the body for a long time without causing illness, but then it begins to multiply vigorously. This is facilitated by:
- Prolonged exposure to the sun and abuse of solariums;
- Lack of hygiene and frequent use of hygiene products with antibacterial components for washing the body;
- Loss of strength, stress, prolonged painful condition, decreased immunity;
- Irrational use of antibiotics.
Signs of the disease appear as soon as immunity reaches a critical point. For example, during pregnancy this is most often the fifth or sixth month of gestation.
Lightened lesions appear on the skin, which gradually become pinkish, yellowish or dark brown. The affected areas do not hurt, itch or get wet, and over time become covered with scales similar to bran, which give the name to the disease.
So, it is not difficult to detect the disease, since it has a number of noticeable signs:
- Pink, yellow or light brown spots appear on the skin.
- The affected areas of the skin dry and peel.
- There is itching, initially not too strong.
The spots appear around the hair follicles, gradually increasing in size and connecting with each other. At first they are light in color, but over time they can turn dark brown or brown. The spots feel flaky to the touch. The small scales covering them are white and are easily scraped off. The location of the spots is asymmetrical - they can appear on the right or left half of the body, or on both. Most often they can be seen on the back, stomach, neck and chest.
The disease does not affect the general condition of a person in any way. This leads to patients not seeing a doctor for a long time. The outbreaks gradually grow, capturing new areas. The skin on the chest and back is most affected. Sometimes rash spots with jagged edges cover the entire body, with the exception of the feet and palms. Due to hair loss, bald spots appear on the head.
The following types of disease are distinguished:
- Inverted
- spots appear in the folds of the skin, under the breasts, on the bends of the elbows and knees, in the armpits. The disease does not bother the patient, since the affected areas of the skin are not inflamed. - Erythematous-squamous
- spots can appear throughout the body, but also do not show signs of inflammation. - Follicular
is a dangerous type of pityriasis versicolor. The skin in areas affected by the fungus becomes inflamed, small ulcers appear, there is noticeable itching and significant discomfort.
How is pityriasis versicolor transmitted?
Pityriasis versicolor is transmitted through household contact, but this is rare: the disease is not very contagious. The causative agent of pityriasis versicolor, a fungus from the genus Malassezia, is present on the skin of most people, but does not penetrate the epithelium and does not lead to the appearance of a rash. However, under the influence of various factors, yeast transforms into a pathogenic form and begins to destroy skin cells. This process can be triggered by various factors: from excessive sweating to endocrine disorders.
Despite the low contagiousness of this type of lichen, patients are advised to adhere to some recommendations:
- do not share bed linen or towels;
- do not wear other people's clothes;
- do not visit baths, saunas, public swimming pools.
You should also take special care to disinfect the patient’s underwear, clothing and hats: wash at high temperatures (possibly boiling), iron with a hot iron, use steam treatment.
Treatment methods
Alarming symptoms in the form of redness, burning, the appearance of pustules and the formation of spots signal the development of multi-colored lichen. At the initial stages, patients are often treated with folk remedies, but this leads to a worsening of the situation. They go to the doctor at the next stage of development.
Purulent processes are the result of the penetration of a secondary infection through the skin.
Pityriasis versicolor is treated with tablets, ointments, and creams. The main thing is to achieve intensive exfoliation of the epidermis. The skin is cleansed of fungi and affected tissues. The deeper the treatment penetrates, the faster the effect will be noticeable. For infectious diseases, a wide range of medications are used.
Methods can include either a single component or a set of measures. More often, treatment with tablets is accompanied by the use of ointments and dietary supplements. Your doctor may prescribe compresses to relieve itching.
Medications
Treatment options are often systemic in nature. Antifungal drugs, sprays, creams with intense effects help treat the disease and relieve unpleasant symptoms. The method is selected regardless of whether the lichen is on the back, face or neck. In the fight against the disease, imidazoles, triazoles, and allylamines are used.
| Effective ointments, gels | ||
| Name | Peculiarities | Price |
| Travogen | Antimicrobial, antifungal drug. Apply once a day to the affected area. | From 480 rub. |
| Lamisil | Destroys pathogen cells. Apply once a day to cleansed skin for a month. | From 520 rub. |
| Exoderil | Apply once a day for four weeks. Destroys fungi and bacteria, stops the development of the pathogen. | From 440 rub. |
| Antifungal drugs | ||
| Orungal | Stops the proliferation of fungi, take one tablet a day for a week. highly effective drug. | From 2,000 rub. |
| Nizoral | Suppresses the development of pathogenic microflora. Relieves symptoms in a short time. | From 350 rub. |
| Fluconazole | A highly effective antifungal agent. The dosage regimen is prescribed individually. | From 30 rub. |
| Products for treating affected areas | ||
| Kanesten | A drug with a wide spectrum of action. Spray onto the affected area twice a day for three weeks. | From 1,600 rub. |
| Thermikon | A spray that has an antibacterial and antifungal effect. Apply twice during the day. The course lasts up to seven days. | From 350 rub. |
| Fungoterbin | Destroys bacteria, fungi, stops the development of pathogenic microflora. Within seven days it completely eliminates symptomatic manifestations. | From 300 rub. |
Your doctor may recommend salicylic acid. The solution is prepared in individual proportions. Wipe the affected areas to prevent fungal growth and infection. It is acceptable to prescribe Betadine, Vocadine and Iodopirone.
Other means
Lichen versicolor can be cured at home only with medication. But traditional medicine will help minimize unpleasant symptoms and prevent the recurrence of the disease. Use:
- infusion of pine needles;
- infusion of blackberry and calendula leaves;
- peppermint decoction;
- homemade St. John's wort ointment;
- boiled buckwheat compress.
If the pills do not help, the doctor may prescribe complex therapy. In conditions of extensive lesions, medications, physiotherapy, and the use of drugs to exfoliate the stratum corneum are used. Multicomponent treatment may include:
- Ultrasound therapy
. Reduces the frequency of exacerbations, stops the development of pathogenic bacteria. Strengthens the effect of medications. - Laser therapy
. Activates natural skin regeneration, normalizes local immunity. Can be used contact or remotely. - Ultraviolet medium wave therapy
. Increases the effectiveness of natural defense mechanisms and has a beneficial effect on the skin.
A complex effect on the lesions and the internal pathogen will allow you to quickly reduce the frequency of symptoms, relieve itching and irritation. The spots of pityriasis versicolor gradually fade and disappear from the skin. After competent therapy, there are no scars, scars or other visible marks on the skin.
Is it possible to cure pityriasis versicolor?
With proper therapy, pityriasis versicolor is easily treated and goes away within 2-3 weeks. To do this, you need to make an appointment with a dermatologist, who will conduct an examination and prescribe additional tests.
As a rule, the diagnosis is established in the presence of a typical clinical picture, but to confirm it, the following analyzes and tests are performed:
- examination under a Wood's lamp: fungal colonies are illuminated;
- microscopic examination of the scraping: shows the presence of yeast;
- Balzer test using iodine-containing solutions.
A dermatologist may also prescribe histological studies, general blood and urine tests. Based on the results of the examinations, treatment tactics are developed.
Depending on the severity and severity of the infection and the symptoms of lichen, therapy includes:
- the use of external agents (sprays, lotions, ointments) with antifungal components. If the scalp is affected, special shampoos are prescribed;
- antifungal drugs for internal use. Prescribed to patients prone to relapses of pityriasis versicolor, or to patients with atypical manifestations of infection.
If the patient suffers from severe itching (which is extremely rare), antihistamines may be prescribed.
Tinea versicolor: possibilities of using shampoo containing ketoconazole and zinc pyrithione
Pityriasis versicolor (pityriasis versicolor) is a common superficial skin lesion caused by lipophilic fungi of the genus Malassezia [1]. Fungi of this genus are the only representatives of the fungal kingdom that are commensals of normal human skin [2]. It is believed that at least 90% of the entire population of the Earth are carriers of Malassezia, and approximately up to 10% of the planet's inhabitants are affected by it, although the disease is considered opportunistic and not contagious. The intensity of colonization changes with age: it is extremely low in newborns and then gradually increases towards puberty, as the activity of the sebaceous glands increases [3]. In the population, the incidence statistically depends on: – age (peak incidence is at the age of 14–40 years) [2]; – gender differences (men get sick 1.5–2 times more often) [2]; – the presence of concomitant diseases of the gastrointestinal tract, endocrine disorders, vegetative diseases, immunodeficiencies of various etiologies [2]; – geographic latitude (in temperate climates – about 2%, in tropical climates – up to 40% of the total population) [4]; – professional activity of patients (in persons engaged in physical labor and sweating heavily) [3]; – hereditary predisposition [1]. The above factors significantly influence the composition of the sweat-fat mantle. A change in the chemical composition of sebum, favorable for the fungus, is an increase in the concentration of oleic, palmitic, linoleic, linolenic, stearic, and myristic fatty acids [2]. The favorite place of localization is the skin of the chest and back; less often, elements are noted on the skin of the neck, abdomen, lateral surfaces of the torso, and the outer surface of the shoulders. In addition, rashes can be found on the scalp, but without affecting the hair, sometimes in the groin folds and axillary areas. The disease is manifested by the appearance of pinkish-brown spots with slight pityriasis-like peeling without inflammation and subjective sensations (rarely - slight itching). Merging, the spots can form quite large lesions with scalloped borders. Their color gradually becomes darkish brown. The spots do not protrude above the skin level, and their surface is covered with small pityriasis-like scales. Insolation and ultraviolet irradiation have a detrimental effect on the colonies of the pathogen, and the skin under them does not tan, and white spots (pseudo-leukoderma) appear against the background of a general tan [5]. In addition to the classic course, there are also atypical forms of lichen versicolor: erythematous-squamous, lichenoid, urticaria-like, erythrasma type, vitiligo, diffuse, circinate, as well as special forms: Malassezia folliculitis and the so-called black form [2]. A study of the clinical forms of lichen versicolor shows that the most common (≈90%) is the classical form of the disease, less often - atypical clinical variants of lichen versicolor. The widespread form of the lesion (≈80%) and typical localization of the rash (≈90%) predominate. Knowledge of atypical clinical variants and localizations of pityriasis versicolor is necessary for timely diagnosis and effective treatment of the disease [6]. Verification of the diagnosis is carried out: • anamnestiically; • according to the clinical picture; • detection of hidden peeling of the skin (Balzer test with 5% iodine solution); • microscopy of scales from lesions; • using examination under the rays of a Wood's lamp [1, 7]. Tinea versicolor is usually well treated with topical antimycotics. The US FDA has not approved any systemic drugs for its treatment for a long time, even though some of these drugs have already been included in clinical guidelines [8]. Among the traditionally used treatment methods, such as Demyanovich treatment are not currently used, and antiseptics such as 2% alcohol solution of iodine or 2% salicylic alcohol are used along with modern antimycotics. Along with antifungal creams, ketoconazole in the form of 2% shampoo should be noted. The use of external forms that allow covering a significant surface of the body is of no small importance in the treatment of lichen versicolor. Even with individual small lesions, it is recommended to treat all areas where lichen versicolor usually develops. The shampoo is used once a day for 5 days [9]. Ketoconazole in the form of shampoo as a drug for the treatment of lichen versicolor was included in the clinical recommendations of the 2010 RODVC [10] and is widely used in world practice [11].
But there are also some features of the mycosis under study, which increasingly force one to turn to systemic and combination therapy. First of all, these are recurrent, widespread and atypical forms of the disease, as well as cases of failure of local therapy. The most important problem of local therapy is the impossibility of 100% visual control of the treatment of lesions, since the pathogen can remain in subclinical quantities in places that patients do not treat during treatment for various reasons. This is especially true for men, who are initially generally recognized to be less compliant with external therapy, although they get sick more often. Therefore, the level of relapses of lichen versicolor is at least 20% after local treatment, and, according to some data, the number of patients with relapses of this pathology after treatment varies from 60% in the first year of observation to 90% over 2 years, more often with immunosuppression, excessive sweating, the presence of seborrhea, etc. [12, 13]. Complex treatment with local antifungal agents: cream + shampoo (as a shower gel), as well as combination therapy with systemic and local drugs using antifungal shampoo is one way to solve this problem. Along with the main one, at the second stage, preventive maintenance local therapy is required using shampoo 1-2 times a week. [9, 12], mainly after episodes of severe sweating. The establishment of the dependence of the clinical manifestations of mycotic infection on the composition of the sweat-fat mantle has led to the fact that in recent years, shampoo with a combination of zinc pyrithione and ketoconazole has become more actively used in the treatment of patients with Malassezia infection (including pityriasis versicolor) and associated skin diseases [14]. It has been shown that the use of drugs with a sebostatic effect reduces the likelihood of relapses in Malassezia-associated skin diseases [15].
Zinc pyrithione and ketoconazole are included in Keto Plus shampoo (Glenmark Pharmaceuticals Ltd., India). Ketoconazole, like all azoles, inhibits the biosynthesis of ergosterol and has a fungistatic effect in low concentrations, and has a fungicidal effect in higher concentrations - 2%, as in shampoo. Zinc pyrithione has antiseptic, drying, keratoregulating, sebostatic and anti-inflammatory properties. The combined action of the components of Keto Plus shampoo mutually potentiates the effectiveness of therapy. A treatment option has also been proposed, where instead of a 5-day period of use of shampoo, a 2-week period is used, followed by a transition in the case of common forms to preventive use with the application of 1 r./week. for a long period of time in order to increase the reliability of the regimen and reduce the likelihood of relapses [16]. In our practice, we have been using Keto Plus shampoo for the treatment of lichen versicolor since 2009 [17], and during this period we have accumulated sufficient experience in its use both in primary treatment regimens and at the preventive stage. Giving preference to combination regimens using systemic itraconazole (200 mg once a day for 7 days) or an integrated approach using modern topical antifungal drugs in the form of a cream or solution (1-2 times a day for 1-3 weeks. depending on the drug), we almost always, in addition to such treatment, recommend a combination of zinc pyrithione and ketoconazole in the form of shampoo as a shower gel for the entire duration of therapy in the patient’s usual hygienic regimen (optimally 1 time per day). The use of shampoo containing ketoconazole and zinc pyrithione was assessed positively by patients: the texture and smell of the shampoo are pleasant, it foams well, so we began to recommend it instead of cosmetics. In addition, it must be taken into account that most cosmetic shampoos, shower gels and soaps often have a slightly alkaline pH value, and excessive alkalization of the skin creates more favorable living conditions for fungi of the genus Malassezia, which is excluded if replaced with a special Keto Plus product. If the use of shampoo as a drug for treatment in the practice of dermatovenerologists already occupies a worthy place (both in monotherapy and in complex therapy with local antifungal agents), then information about its use for secondary prevention in individuals prone to relapses is rare [16]. We have accumulated sufficient experience in such use, primarily in risk groups: young people who sweat frequently, who are actively involved in physical education and sports, as well as among law enforcement officers who are forced to wear multi-layered warm clothing for a long time. We present the results of our observations. Purpose of the study: to develop approaches to secondary prevention for lichen versicolor in people prone to relapses, using shampoo containing a combination of ketoconazole and zinc pyrithione. Materials and methods: the work was carried out in conditions of predominantly outpatient dermatological appointments in the period from 2011 to 2015. The study included 62 people aged 21 to 36 years, who underwent annual medical examination and had at the time of inclusion at least the second episode of the disease in 3 years, whose skin condition and the occurrence of relapses could be assessed within a period of at least 2 years after the course of combination therapy according to the scheme indicated above. Therapy was continued until complete clinical resolution. Men made up the majority - 55, women were 7 people. The diagnosis before the course of treatment was verified anamnestiically, clinically, Balzer test, laboratory, the clinical form in 45 patients was quite common. HIV infection was excluded in patients. After completion of treatment, it was recommended to use shampoo with a combination of ketoconazole and zinc pyrithione (Keto Plus, Glenmark, India) as a shower gel for prophylactic purposes. Method of application: the shampoo is worn with the formation of foam on wet skin during the shower from the hair to the level of the pelvis, if necessary, lower, and is not washed off for 5-6 minutes, after which the patient is quickly rinsed. The procedure was recommended to be carried out at least 1 time per week, and if episodes of intense sweating occur, even after such episodes, but not more than 3 times per week.
Results and discussion: of the 62 people whose history was tracked during the observation period, 17 patients did not comply with the instructions and stopped using the shampoo immediately after completing the course of therapy. This group was no less interesting than the groups in which patients used Keto Plus shampoo for prevention, and it was assigned the role of a control group. The first group, in which Keto Plus shampoo was used for more than six months but less than a year, included 31 participants. The second group, where patients reported using Keto Plus shampoo for 2 years according to the recommended preventive regimen, included 14 patients.
In the control group that did not receive preventive therapy, relapses at different times during the observation period were noted in 6 (≈35%) people, while common forms of infection reappeared in 2 patients. In the first observation group, in which the period of preventive use of shampoo was from six months to 1 year, no relapses were noted during the period of preventive use of Keto Plus shampoo. The appearance of clinical manifestations of lichen versicolor was observed in 6 patients over a period of at least 8 months. after completing a course of preventive use of shampoo, mainly in the autumn-winter period, they were represented by single typical colonies on the skin of the trunk or neck. The percentage of relapses in the first group was ≈16%, which is more than 2 times less than in the control group. In the second observed group, which used Keto Plus shampoo in the recommended preventive regimen, there were no relapses of the disease continuously throughout the observation period, i.e. for at least 2 years. Patients in this group positively noted the appearance of a large package of shampoo (150 ml instead of 60 ml), which was regarded by patients as an economically advantageous offer, and we, in addition, assessed it as increasing patients’ compliance with the preventive regimen. I would like to note that both during the main course of therapy and during periods of long-term preventive use of Keto Plus shampoo, there were no cases of individual intolerance, either by subjective or objective indicators.
Conclusions: Our observational study clearly demonstrates the effectiveness and safety of a shampoo containing a combination of ketoconazole and zinc pyrithione as a means for secondary prevention of tinea versicolor in the recommended regimen, especially in individuals predisposed to the disease. Unfortunately, the refined contingent of selected patients, small samples and not very long follow-up periods do not allow us to make population-based, statistically based conclusions about the timing of such preventive therapy. We are cautious about recommendations for many years of continuous use of shampoo with a combination of ketoconazole and zinc pyrithione throughout the peak period of the disease, limited, for example, as indicated above, to the age of 40 years. We have formed the opinion that a two-year period of preventive continuous use of Keto plus shampoo in a regimen of at least 1 rub./week, and in the event of episodes of intense sweating - and after such episodes, but not more than 3 rub./week., is quite sufficient for disease control. Based on clinical experience with the use of such a regimen, we can conclude that preventive treatment after the main course of therapy reduces the likelihood of relapses. In some cases, namely, if in some individuals the tendency to relapse of lichen versicolor persists after discontinuation of the prophylactic use of shampoo, it will be more economically profitable to carry out a repeated course of the main treatment, but again with a subsequent repetition of a two-year course of anti-relapse therapy, rather than continuous preventive use throughout the entire peak period of illness.
Thus, in modern conditions, in the arsenal of dermatologists and mycologists there is an effective local component of the treatment of versicolor versicolor in the form of easy-to-use Keto Plus shampoo, which is an etiopathogenetic combination of ketoconazole and zinc pyrithione as a shower gel. It is especially advisable to use it in common, recurrent and atypical forms of the disease, both in combination with systemic drugs and in complex use schemes together with local antifungal creams (solutions) to increase the effectiveness of treatment of lichen versicolor and prevent (reduce the likelihood) of relapses of the disease. In addition, Keto Plus, due to its pronounced antifungal, antiseptic, drying, sebostatic and anti-inflammatory activity, can be recommended for the preventive treatment of lichen versicolor after the main course of treatment 1-2 times per week. lasting up to 24 months. And the unique pharmacological properties of Keto Plus, combined with ease of use, safety (good tolerability) and pleasant organoleptics, give hope for high patient compliance with the prescribed treatment and prevention regimens.
Literature 1. Klimko N.N. Mycoses: diagnosis and treatment. Guide for doctors. 2nd ed. M.: VG Group, 2008. P. 114. 2. Yakovlev A.B., Suvorova K.N. Malassezia is an infection of human skin. Academic method. allowance. M.: GOU DPO RMAPO, 2005. 3. Sergeev A.Yu., Sergeev Yu.V. Fungal infections. Guide for doctors. 2nd ed. M.: BINOM Publishing House, 2008. pp. 230–238. 4. Fitzpatrick T., Johnson R., Wolfe K. et al. Dermatology. Atlas-directory. Per. from English M.: Praktika, 1999. 5. Tarasenko G.N., Tarasenko Yu.G. Fundamentals of practical mycology. M.: OASIS-Design, 2008. pp. 29–34. 6. Abdulloeva M.A., Zoirov P.T. Clinical forms of versicolor versicolor // Healthcare of Tajikistan. 2011. No. 4. pp. 12–15. 7. Arabian R.A., Klimko N.N., Vasiliev N.V. Diagnosis of mycoses. St. Petersburg: Publishing house SPbMAPO, 2004. pp. 60–62. 8. Wolfe K., Johnson R., Surmond D. Dermatology according to Thomas Fitzpatrick. Atlas-directory. Per. from English M.: Praktika, 2007. pp. 834–837. 9. Sergeev Yu.V., Shpigel B.I., Sergeev A.Yu. Pharmacotherapy of mycoses. M.: Medicine for everyone, 2003. pp. 137–138. 10. Dermatovenerology - 2010. Clinical recommendations (Russian Society of Dermatovenerologists) / Ed. A.A. Kubanova. M.: DEX-Press, 2010. pp. 299–301. 11. Wolf K., Goldsmith L.A., Katz S.I. and others. Fitzpatrick’s dermatology in clinical practice: in 3 volumes; lane from English; total ed. A.A. Kubanova. M.: Panfilov Publishing House; BINOMIAL. Knowledge Laboratory, 2012. Vol. 3, 2013. pp. 1995–1998. 12. Ustinov M.V., Sirmais N.S. Systemic therapy of pityriasis versicolor // Polyclinic. 2014. No. 1. P. 80–83. 13. Faergemann J. Pityrosporum infections // J. Am. Acad. Dermatol. 1994. Vol. 31 (Suppl. 1). P. 18–20. 14. Kudryavtseva E.V. Malassezia infections in the practice of a dermatologist // Advances in medical mycology. T.13. M.: National Academy of Mycology, 2014. pp. 118–120. 15. Albanova V.I., Kalinina O.V. Seborrheic dermatitis of the scalp: the role of Malassezia // Advances in medical mycology. T.14. M.: National Academy of Mycology, 2015. pp. 11–13. 16. Abidova Z.M., Shorahmedov Sh.Sh., Alimzhanov D. Study of the clinical effectiveness of ketoconazole shampoo // Advances in medical mycology. T.11. M.: National Academy of Mycology, 2013. pp. 121–123. 17. Ustinov M.V. Treatment of recurrent common forms of lichen versicolor // All-Russian scientific and practical conference “Current issues of dermatology and urogenital pathology”. Abstract. reports. M.: FMBA of Russia, FGOU IPK FMBA of Russia, 2009. pp. 48–50.
Is it possible to cure pityriasis versicolor permanently?
If you follow medical recommendations, pityriasis versicolor responds well to treatment: the rash completely disappears in 2-3 weeks. But the infection tends to become chronic: in this case, relapses occur every time sweating increases, for example, in the warm season, when traveling on vacation, or during intense physical activity.
To avoid this, you must:
- consult a dermatologist at the first signs of the disease. At the initial stage, pityriasis versicolor can be easily confused with other skin infections: tinea versicolor, seborrheic dermatitis, eczema, vitiligo, and so on. Each disease requires specific treatment, which is why it is so important to recognize the disease as early as possible;
- refuse self-medication. Uncontrolled use of medications and the use of “folk remedies” will not only not lead to a cure, but can also aggravate the course of the infection;
- follow your doctor's recommendations. This applies to both the use of prescribed medications and personal hygiene.
In this case, the patient can quickly recover from pityriasis versicolor and avoid its relapse.
How do you know if pityriasis rosea is going away?
After a course of therapy, the spots disappear without scarring. In place of the plaques, clean skin remains, possibly lighter. Over time, the color evens out. In patients with atypical lichen, ulcers may form.
Complications during self-medication:
- infection of affected areas with bacteria;
- suppuration, ulcers;
- hyperpigmentation.
Hyperpigmentation
To prevent this development of the disease, at the first symptoms of pityriasis rosea, it is recommended to make an appointment with a dermatologist.
Is it possible to sunbathe with pityriasis versicolor?
This dermatosis is popularly called “sun fungus”: during the beach season, the yeast is activated and the disease is diagnosed most often. At the same time, the areas of the skin affected by the colonies do not tan and remain white - the patient is covered with light spots, which bring him to the dermatologist’s office.
Since pityriasis versicolor can be diagnosed during rest, patients are often interested in: is it possible to sunbathe with pityriasis versicolor? Opinions differ on this matter. Previously, quartz treatment was prescribed for the treatment of lichen versicolor: under the targeted influence of ultraviolet light, colonies of the fungus died. But now many dermatologists dispute this method of treatment.
UV radiation can be dangerous for an organism weakened by infection. In addition, the occurrence of pityriasis versicolor indicates a decrease in immune strength. Therefore, experts do not recommend exposing the skin to additional stress.
If the patient doubts whether it is possible to sunbathe with pityriasis versicolor, he is recommended to consult a dermatologist. The doctor will give recommendations taking into account the individual characteristics of the body, the severity of the disease, its form and location. If you follow medical prescriptions, the patient will avoid the complications of lichen and will be able to recover in a short time.
It should also be remembered that if the patient decides to sunbathe with pityriasis versicolor, the areas of the skin affected by the colonies will remain light: it will not be possible to get an even and beautiful tan. Therefore, it is better to first get rid of the disease, and only after that return to the beach.
Incorrect treatment of pityriasis rosea
- Lubrication with iodine, brilliant green
. These antiseptic drugs do not provide results in the treatment of pink dandruff. The virus is located deep in the skin, so iodine or brilliant green cannot affect it, but at the same time they dry out the skin, causing a burn. - Celandine
. The poisonous sap of the plant leads to damage and inflammation of the skin. Celandine causes burns, increasing the risk of complications. - Zinc ointment
. Causes skin tightness. - Salicylic acid, alcohol
. Ineffective against the virus. Dries and irritates the skin, increasing peeling. Leads to hyperpigmentation. - Vinegar
. Dries out the skin and increases peeling.
To treat Gibert's disease, you can only use products prescribed by a dermatologist.
Can pityriasis versicolor be cured with iodine?
Iodine-containing products are used in the diagnosis of lichen versicolor. Yeast colonies are sensitive to iodine, causing them to absorb it to a much greater extent than surrounding healthy skin. Therefore, if you apply an iodine solution to the epidermis, the affected areas will be much darker.
But many patients believe that iodine is suitable not only for diagnosis, but also for self-treatment of pityriasis. An alcohol solution of iodine is a popular antiseptic that is often used to disinfect the skin. Fungi from the genus Malassezia, which cause tinea versicolor, are sensitive to it and are partially killed upon contact with this substance, but it is impossible to completely destroy them with iodine.
In addition, an alcohol solution of iodine greatly dries already damaged skin, which can lead to various complications of dermatosis.
As a result of self-medication:
- the disease drags on - recovery does not occur, and the rash spreads to new areas of the body;
- the likelihood of relapse increases - after the rash disappears, it appears again when the immune system is weakened and is chronic;
- new symptoms are added to the symptoms of the disease: tightness and dryness of the skin treated with iodine, itching may occur.
Pityriasis versicolor can be cured with antifungal medications prescribed by a dermatologist. Special creams and ointments affect only colonies of the pathogen and do not affect healthy epithelium. Also, many products contain care components that additionally moisturize the skin, accelerate its regeneration and promote the resumption of melanin synthesis.
Reasons for the development of pink lichen of Zhiber
Although the disease has been known for a long time, its pathogenesis still remains unclear. Various factors and pathogens have been proposed as causes:
- infectious;
- viral;
- bacterial;
- fungal;
- Mycoplasma pneumoniae;
- “toxic rash due to unknown gastrointestinal infection”;
- insect bites;
- isomorphic response;
- autoimmune disease;
- psychogenic cause.
Insect bite
Early research suggested a connection to new, unused clothing. Lassar and Rosenthal attributed this role to flannel and knitwear.
The development of a peculiar skin plaque was observed at the site of insect bites, especially fleas, as well as on old scars, with healing gunshot wounds, and at the site of intramuscular injections, which suggests that pink dandruff is simply an isomorphic reaction.
Some scientists have tried to show that pityriasis rosea is a psychogenic disease and is more common in "highly stressed" or mentally ill people. According to them, stress can aggravate the lesion and cause itching. Others consider the psychosomatic theory unlikely.
Attempts have also been made to hypothesize that RP is a “toxic rash of gastrointestinal infection,” the result of dietary error and gastric dilatation.
In 1970, Birch and Rowell postulated an autoimmune cause of the disease, in which the predisposition was genetically determined and sensitized by microorganisms.
However, the infectious background of the disease is most widely considered. Clinical features of the pathology, such as the irregular occurrence of prodromal symptoms and the severity of morbidity in the autumn-spring period, indicate a viral etiology. There appears to be an association with a recent upper respiratory tract infection in some patients.
The spread of the disease in the family, among children at school, among soldiers in the barracks, among people using Turkish baths has not been confirmed, so many experts believe that it is a non-infectious disease.
However, pityriasis rosea has been found to be more common among dermatologists than among otolaryngologists, suggesting that it is spread through contact with low infectivity, leading to increased incidence with increasing number of contacts.
In addition, the pathology is more common in people with weakened immune systems, for example, pregnant women and patients with bone marrow transplantation. Spontaneous resolution and relapses, occurring in less than 3% of patients, are also consistent with the theory of a viral origin of the disease.
There is some objective evidence to support the viral theory of the disease. In 1968, scientists demonstrated the presence of picornavirus-like intranuclear bodies in the tissues of African green monkeys inoculated with a liquid that affected the color of the lesions, and in electronic sections of these lesions. However, none of the studies have identified the genome of picornaviruses. Pityriasis rosea has also been described in a patient with proven Echo virus infection.
The HHS-7 virus, a Roseola virus from betaherpesviruses, is also suspected. Viruses of this family cause acute and chronic infections. They can also remain latent for many years, and a weakened immune system leads to their activation. HHS viruses have been detected in children with RP and adults with pink dandruff in serum, white blood cells, and biopsies of skin lesions.
However, the relationship between pityriasis rosea and HHS-7 remains controversial according to some scientists, due to the low DNA sequence index of HHS-7. The virus has also been detected in the plasma of healthy people.
It has been suggested that the disease is associated with bacterial infection, including syphilis and tuberculosis. In 1942, student. Benedek explained the occurrence of the disease by the reactivation of latent foci of Baccillus endoparasiticus.
The role of Staphylococcus albus and hemolytic streptococci was also increased. In recent years, infections with Legionella micadadei, L. longbeachae, L. pneumophila, Chlamydia pneumonie, Ch. trachomatis, but the opinions of dermatologists about their role in the pathogenesis of RP are divided. Thus, the issue of the involvement of these microorganisms requires further research.
The clinical appearance of the mother's plate, with morphological features often resembling a lesion of mycosis, especially ringworm, suggests that the cause of pink dandruff may be a fungal infection.
Some medications also sometimes cause skin lesions similar to pityriasis rosea. Among them:
- captopril;
- metronidazole;
- isotretinoin;
- D-penicillamine;
- levamisole;
- diphtheria toxoid;
- bismuth;
- gold;
- barbiturates;
- ketotifen;
- clonidine;
- terbinafine;
- omeprazole
Pityriasis rosea has been reported following administration of BCG, IFN-alpha and hepatitis B vaccines.
Now scientists are inclined to conclude that such a reaction of the body can be caused by various factors, and this is very important to take into account when diagnosing pathology. By identifying the suspected cause, you can quickly and permanently get rid of unpleasant symptoms.
The most likely reasons are a weakened immune system and the activation of one of the types of herpes viruses against this background. Therefore, it is necessary to consider all causes that weaken the immune system.
When is deprivation shampoo treatment effective?
Medicinal shampoos are topical preparations that affect the pathogen directly at the sites of inflammation. Their use is justified in cases where the disease is caused by a scalp fungus. Dermatologists include shampoos in complex therapy for the following types of lichen:
- pityriasis (colored);
- shearer;
- pink.
Topical fungicidal preparations are suitable for the treatment of seborrheic dermatitis and candidiasis of the scalp. Medicinal shampoos alleviate scaly and weeping lichen, which are also called psoriasis and eczema, respectively.
Contraindications and features of the use of shampoos
Therapeutic shampoos for lichen contain antifungal substances, many of which are highly allergenic. Therefore, they are used in accordance with the instructions and recommendations of a dermatologist or trichologist. Frequently washing your hair with preparations is fraught with itching, burning, redness and peeling of the skin.
Features of using shampoos:
- a small amount of product (5-7 ml) is applied to damp hair;
- rub into the scalp in a circular motion for 1 minute;
- After 3-5 minutes, remove with running water.
The use of drugs is contraindicated for:
- hypersensitivity to components;
- purulent inflammation of the skin;
- burns;
- abrasions.
In the first days of treatment, a third of patients complain of hair loss. It is possible that the natural shade of the hair will change.