Urticaria (nettle rash, nettle fever) is a skin disease of allergic and toxic origin, which is characterized by the appearance of severely itchy blisters on the skin or mucous membranes, reminiscent of a burn resulting from exposure of human skin to nettles (hence the name).
Depending on the cause and duration of its occurrence, urticaria has two main forms of manifestation:
- Acute
- Chronic.
Acute urticaria is most often a form of food or drug allergy. This is an allergic reaction of the body to any external irritant (medicines, food, insect bites, household chemicals and cosmetics). The acute form of the disease can occur unexpectedly and also disappear suddenly (its duration ranges from several hours to 1.5-2 weeks). In children, the acute form of urticaria most often predominates, mainly an allergic manifestation of the disease. One of the more severe manifestations of the acute form of urticaria is Quincke's edema, in which there is swelling of the facial skin and swelling of the larynx (which can lead to suffocation).
Chronic urticaria is a manifestation of chronic diseases in the body (such as stomach ulcers, helminths, gastritis, malignant and benign neoplasms, thyroid diseases, etc.). As a rule, the duration of this form of urticaria is more than 6 weeks and can last on average 3-5 years, its course is characterized by repeated attacks.
Symptoms.
The main symptoms of urticaria:
- Multiple rashes on any part of the skin in the form of flat blisters that have a pale pink color (the blisters can merge and acquire gigantic sizes)
- Severe itching or burning in the area of the rash
- Complete reversibility of the rash without any remaining scars, pigmentation or white spots on the skin. True, unlike nettle burns, this disease appears again, and in other places.
- With prolonged progression of the disease, accompanying symptoms appear - headache, general malaise, fever.
In adults and children, the symptoms of urticaria are similar and do not depend on the age of the patient.
Diagnostics
Demographic urticaria is easily determined by a dermatologist. If necessary, the specialist will prescribe examinations and tests to make an accurate diagnosis. It is important to differentiate the disease, since there are a sufficient number of varieties of urticaria.
The following examination methods will help diagnose pathology:
| Name | Diagnostic methods |
| Visual inspection |
|
| Laboratory research |
|
| Skin tests |
|
| Instrumental diagnostics |
|
In some situations, to make an accurate diagnosis, you will need to consult other specialized doctors (gastroenterologist, allergist, endocrinologist, neurologist, psychiatrist, immunologist).
Treatment of acute and chronic urticaria.
First of all, it is necessary to identify and eliminate all factors that could cause the allergy. In the case of chronic urticaria, when the allergen cannot be identified, it is necessary to undergo a more detailed examination by relevant specialists (gastroenterologist, rheumatologist, dermatologist, otolaryngologist, infectious disease specialist, etc.) and begin treatment for concomitant diseases.
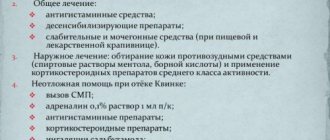
To treat urticaria, the patient is prescribed:
- Antihistamines
- Corticosteroids (to treat the most severe forms of the disease)
- Aerosols, antipruritic ointments
- A special diet that excludes foods that cause allergies from the diet.
When to see a doctor
Demographic urticaria can be easily determined at home using a simple test. But only a dermatologist can confirm the diagnosis and select medications. Considering the source of the allergic reaction, you will need to consult, for example, a parasitologist if the cause of the urticaria is parasites.
If you have thyroid disorders, you should be examined by an endocrinologist. Assess blood sugar levels and hormone production. A gastroenterologist will confirm or rule out the development of gastritis. The immunologist will check the condition of the body, namely its defenses.
Prevention
You can prevent the occurrence of an allergic reaction, just remember the useful advice of your doctor:
- give preference to clothes made from natural fabrics;
- use belts and elastic bands less;
- remove from your wardrobe items made from rough fabric with convex seams;
- refuse tight socks, stockings, tights;
- strengthen immunity;
- do not put backpacks or bags on your shoulders;
- in the shower or while taking a bath, use soft washcloths, remove pumice stones and brushes;
- during long sedentary work, take periodic breaks and warm up;
- do not wear tight shoes or heels;
- It is recommended to avoid long walks;
- avoid hard massage;
- engage in light sports where falls and impacts are excluded.
Demographic urticaria requires careful attention to your health. A person needs to eliminate bad habits from life, eat right, protect the body from stress and increased emotional stress.
For preventive purposes, visit a doctor, get tested and, if necessary, undergo additional examinations. Timely detection of the disease will allow it to be cured and negative consequences to be prevented.
Summary
Chronic urticaria is diagnosed when it lasts more than 6 weeks. Most cases of chronic urticaria can be classified as chronic idiopathic urticaria, which has no externally visible cause. More than half of all cases of chronic idiopathic urticaria are believed to have an autoimmune mechanism, primarily due to the production of autoantibodies directed against the high-affinity FcεRI immunoglobulin E (IgE) receptors. It is assumed that the basis of chronic urticaria is an autoimmune mechanism. This hypothesis is supported by evidence of a combination of chronic urticaria and various autoimmune diseases, such as thyroid disease, rheumatoid arthritis, systemic lupus erythematosus, Sjögren's syndrome, celiac disease and type 1 diabetes mellitus. Here we look at the connection between chronic urticaria, thyroid disease and other autoimmune diseases, and the impact of such correlations on the treatment of chronic urticaria.
Introduction
It is believed that 25% of the population have experienced urticaria during their lifetime1. Chronic urticaria (CU) includes cases lasting more than 6 weeks. Chronic urticaria usually lasts from 1 to 5 years, but in 14% of patients its duration may exceed 5 years2. The literature describes 2 patients with CU who experienced emotional distress, feelings of isolation and fatigue in response to their condition, which is comparable to similar disorders in patients with coronary heart disease3. This highlights the importance of minimizing both the physical and psychological effects of this disease. CU may occur in response to medications, physical stimuli, manifest as a syndrome of inflammatory or hereditary diseases, or may be idiopathic in nature. Acetylsalicylic acid (ASA) or non-steroidal anti-inflammatory drugs (NSAIDs) are contraindicated in CU. These drugs are thought to inhibit cyclooxygenase, which causes increased production of leukotrienes4. Physical urticaria (classically divided into heat, cold, solar, vibration, pressure-delayed, dermographic, aquagenic, and cholinergic-induced urticaria) occurs in response to external stimuli5. In urticarial vasculitis, skin elements of urticaria persist for more than 24 hours6. CU can be observed in a number of hereditary diseases, such as familial cold autoinflammatory syndrome, Muckle-Wells syndrome, NOMID/CINCA7 syndrome. Urticaria is characteristic of many inflammatory diseases, such as Schnitzler syndrome8, Still's disease9 and Gleich syndrome10. Chronic idiopathic urticaria, unlike physical urticaria and urticaria caused by acetylsalicylic acid (ASA) or nonsteroidal anti-inflammatory drugs (NSAIDs), does not have any noticeable external causes11. Chronic idiopathic urticaria is the most common type of CU, accounting for up to 90% of all cases of CU.1 It has been estimated that between 0.6%12 and 5%13 of the population will experience chronic idiopathic urticaria during their lifetime. More than half of all cases of chronic idiopathic urticaria are thought to be caused by an autoimmune mechanism14. This is supported by the fact that 60% of patients with chronic idiopathic urticaria respond positively to an autologous serum test15. Approximately 50% of patients with chronic idiopathic urticaria have autoantibodies against high-affinity immunoglobulin E receptors FcεRI (IgE) on skin mast cells and circulating basophils14,16. Additional immunological disorders that play a causative role in the development of CC are IgG antibodies directed against IgE antibodies with low affinity IgE receptors (FcεRII)17, antiendothelial antibodies18, and C8 alpha-gamma (C8α-γ) defensins19. Approximately 35% of patients with chronic idiopathic urticaria experience episodes of angioedema and 25% experience dermographism20. Like many autoimmune diseases, chronic idiopathic urticaria has a higher incidence in women than men, with a female to male ratio of 2:121.22 to 4:123. Numerous autoimmune conditions accompany chronic idiopathic urticaria, including thyroid disease, celiac disease, and rheumatoid arthritis (RA).
The purpose of this review is to discuss the association of CU with thyroid disease and other autoimmune diseases, and the implications that these associations have for the management of CU.
Thyroid diseases and chronic urticaria
Thyroid diseases are the most common autoimmune diseases in patients with CU. In the literature, the frequency of autoimmune thyroid diseases in patients with urticaria has a wide range of values and ranges from 6.5% 24 to 57%. 25 Patients with an autoimmune thyroid disease concomitant with chronic urticaria have a more severe and prolonged course of urticaria than those with urticaria without autoimmune disease. thyroid disease.26 Patients suffering from CU and autoimmune thyroid disease have an increased risk of developing angioedema. Leznoff and Sussman, the triad of autoimmune thyroid disease, CU, and angioedema was observed in 15% of patients with CU.27 The risk of developing angioedema in patients with autoimmune thyroid disease and CU is 16.2 times greater than in CU without autoimmune thyroid disease. glands.28 In a recent large study conducted in 12,778 patients with HC, Cofino-Cohen et al found that 9.8% of patients suffered from hypothyroidism, while in the control group such pathology occurred in only 0.6%.21 Hypothyroidism is the most a frequently detected thyroid disorder in patients with CU. The combination of hypothyroidism and CU was more common in women than in men. Patients with hyperthyroidism and CU made up 2.7% of those examined, compared to 0.09% in the control group. In most patients, thyroid disease was detected 10 years after the diagnosis of CU. This means that autoimmune thyroid disease has existed since the onset of CU. The same study found that antithyroid antibodies were significantly more common in HC patients than in the control group. In patients with CU and clinical euthyroid goiter, antibodies to antithyroid peroxidase were detected in 2.7% and antibodies to antithyroglobulin in 0.6%. Aamir et al also noted an association between antithyroid antibodies and CU. However, levels of antithyroglobulin and antimicrosomal antibodies were significantly increased in patients with CU and hypothyroidism.25 The development of thyroid disease is often considered a marker of an autoimmune process. CU has been associated with thyroid disease and with various other autoimmune diseases, including pernicious anemia, celiac disease, type 1 diabetes mellitus, and systemic lupus erythematosus (SLE).29 Although the specific mechanism of the link between the development of thyroid disease and CU is not yet clearly understood , it can be assumed that both diseases arise due to the body’s tendency to autoimmune reactions. It has been hypothesized that thyroid disease may worsen urticaria and contribute to the development of angioedema through activation of the complement system. Blanchin et al. demonstrated a thyroid peroxidase enzyme containing a fragment that binds to the complement protein C4, cleaving it to C4a and activating the classical complement cascade pathway.30 Kirpatrick noted that C4a levels decrease when thyroid disease is treated, resulting in improvement in thyroid cancer. .31 Thyroid disease may aggravate urticaria and promote angioedema through direct mechanisms that lead to complement activation.
Other autoimmune diseases and chronic urticaria
In addition to thyroid diseases, many autoimmune diseases have been studied in association with CU. Confino-Cohen et al found that 12.5% of patients had one underlying autoimmune disease, 2.1% had two diseases, 0.1% had three diseases, and single patients each had four or five more diseases. Among patients with CU and hypothyroidism, rheumatoid arthritis was the most common comorbid autoimmune disease. The incidence of RA in patients with CU and hypothyroidism was 13.25 times higher than in the control group.21 The most important laboratory marker of rheumatoid arthritis, rheumatoid factor, was reported by Ryhal et al. to be significantly increased in patients with CU.32
The risk of developing type 1 diabetes increases in HC patients of both sexes. Women with CU had a significantly higher risk of developing Sjögren's syndrome, celiac disease, or SLE than controls. Most patients were diagnosed with an additional autoimmune disease 10 years after CU diagnosis, 21 highlighting that these diseases were recognized subsequently and were not coincidentally comorbid with CU. An association of celiac disease and CU has previously been noted among children.33 Raynaud's syndrome34 has been described in CU by Asero et al.35 Additional autoimmune diseases such as vitiligo and pernicious anemia have also been associated with CU.36 CU has been shown to have a genetic association with human leukocyte antigens (HLA) - DR4 and HLA-DQ8 alleles.37 Interestingly, HLA-DR4 is strongly associated with rheumatoid arthritis,38 and HLADQ8holds is associated with celiac disease39 and type 1 diabetes40. Other abnormalities have been associated with autoimmune diseases such as Sjögren's syndrome, 41 RA, 42 and SLE. 43 Park et al. reported the development of CU, antinuclear antibodies, and spondyloarthropathy in a 9-year-old boy with C8α-γ defensin19. CU was described in a 10-year-old boy with a strong autoimmune phenotype.44 The patient suffered from alopecia totalis, vitiligo, psoriasis, Graves' disease, Cu, an autoimmune form of Lambert-Eaton myasthenic syndrome, and IgA deficiency. This patient had HLA genes located within the expanded 8.1 AH haplotype, which was responsible for the development of multiple autoimmune diseases.45 This case highlights that CU can arise as part of a larger grouping of autoimmune diseases.
Therapeutic intervention
Guidelines for the treatment of CU have been established with the help of international recommendations.46,47 Using second-generation non-sedating H1 antihistamines as first-line treatment for patients with CU.48,49 If no response is achieved after 2 weeks of treatment with first-line drugs, then As a second line, increase the dose of antihistamines up to four times the standard dose.50 The patient should be warned that sedation may occur with increasing doses of antihistamines. Cetirizine, desloratadine, fexofenadine and bilastine (the latter not licensed for use in Canada) have been identified as the safest antihistamines.51 In 50% of patients, symptoms do not improve with one antihistamine.52,53 A third line of treatment involves switching antihistamines. drug or the addition of a leukotriene antagonist. However, leukotriene antagonists have been shown to be effective in patients with acetylsalicylic acid or NSAID intolerance and food-induced hypersensitivity, but not in chronic idiopathic urticaria.54 A short 3- to 7-day course of systemic steroids can be used in combination with other third-party medications. lines55. If third-line therapy fails, fourth-line drugs include cyclosporine A, H2 blockers, Dapsone, or Omalizumab.56 The most effective fourth-line drug for CS is believed to be omalizumab,56 a humanized monoclonal anti-IgE antibody approved for the treatment of severe asthma . Maurer et al published a randomized, double-blind trial evaluating the efficacy of omalizumab in patients with CC, due to the lack of response to first-line treatment and found that it significantly reduced the symptoms of CC.57 Omalizumab reduces IgE and levels of high-affinity IgE receptors present on mast cells and basophils, 58 in a manner that leads to decreased activation of mast cells and basophils, memory cells involved in the development of CC. Additional treatment options for patients who fail fourth-line drugs include mycophenolate mofetil,59 hydroxychloroquine,60 methotrexate,61 tacrolimus,62 sulfasalazine,63 and intravenous immunoglobulin (IVIG)64. Treatment of concomitant thyroid disease has been reported to result in remission of CU.65 Kirkpatrick conducted a study in patients with CU who had clinical and serologic evidence of autoimmune thyroid disease.66 These patients had previously been treated unsuccessfully with antihistamines and fourth-line agents. It was shown that in all six patients with autoimmune thyroid disease and CU, treatment with levothyroxine resulted in remission of angioedema and urticaria. Rumbryt reported that seven out of ten euthyroid patients with antithyroid antibodies achieved clinical remission of CU after treatment with thyroxine, but relapsed after discontinuation of therapy.67 These studies suggest that in patients with CU, targeting thyroid pathology with levothyroxine can achieve remission. HC. However, Magen et al observed patients with CU and thyroid disease treated with levothyroxine and patients not treated with levothyroxine and found no significant differences, observing improvement in both groups.68 This led to the conclusion that improvement in the clinical symptoms of CU occurred spontaneously, regardless of thyroid treatment. Conflicting data in the literature regarding the effect of treatment of autoimmune thyroid diseases on the clinical course of CU indicate the need for larger studies to establish the role of levothyroxine in patients with CU. The use of NSAIDs has been shown to worsen CU in approximately 20% of patients.69 NSAIDs are widely used to suppress pain and inflammation in rheumatoid arthritis, inflammatory spondyloarthropathies, and arthritic skin congestion. Autoimmune inflammatory arthropathies, especially rheumatoid arthritis, have been shown to occur more frequently in patients with CU than in the general population.21 Thus, exacerbation of symptoms caused by NSAID use should be monitored in patients with CU and autoimmune inflammatory arthropathy. Zembowicz et al. showed that selective COX-2 inhibitors fail to induce urticaria in patients with CU and their condition is worsened by NSAIDs.70 This suggests that selective COX-2 inhibitors may be preferable to NSAIDs for preventing exacerbation of CU symptoms. Previously, it was suggested that Helicobacter Pylori was a possible etiological factor in CU. This was based on reports demonstrating a high prevalence of Helicobacter pylori infection among patients with CU, 71 and improvement in clinical symptoms of CU following H. pylori eradication 72 , 73 . However, this hypothesis has been called into question, because other authors have found no difference in the prevalence of H. Pylori between healthy individuals and patients with CC, 74 and no difference in the formation of autoantibodies, 24 and based on the fact that eradication of H. Pylori does not affect the course of CC75. It has been suggested that these discrepancies in the literature are due to different methods of detection, resistance to therapy, and the possibility of recurrence of H. pylori infection soon after discontinuation of therapy.76 Further complicating the issue, recent evidence suggests that eradication of H. pylori may cause HC.77 Shakouri et al completed a review of the literature on eradication of Helicobacter pylori infection and CU using a grading system, and concluded that the evidence for treatment was weak and large studies are needed to establish whether patients with CU benefit from eradication of HC. pylori.78
Conclusion
CU is defined as urticaria lasting more than 6 weeks. It is now believed that up to 50% of cases of CU are caused by autoimmune mechanisms.14 High-affinity autoantibodies to IgE receptors are the main substances that activate mast cells, basophils and the complement system, leading to the formation of blisters and an inflammatory response.14,16 It is believed that CU occurs in patients due to a predisposition to the development of autoimmune diseases. In accordance with this hypothesis, it is possible to explain the more frequent occurrence of concomitant autoimmune diseases in patients with CU. Thyroid disease, especially hypothyroidism, is the most common comorbid autoimmune disease in patients with CU.21 In addition, thyroid disease can directly aggravate the severity of CU by activating complement.30,31 Other autoimmune diseases that occur more frequently in patients with CU include: include rheumatoid arthritis, SLE, vitiligo, pernicious anemia, celiac disease and Sjörgen's syndrome. 21, 36 In selected cases, CU has been identified as part of a larger autoimmune phenotype. 19, 45 These associations support the theory that the development of CU is due to an innate propensity for autoimmune reactions. As reported in the literature, to achieve remission of CU, it is necessary to treat the pathology of the thyroid gland, which allows for a diversified effect on the course of CU, which has been demonstrated.65 - 67 At the same time, it is expressed as an alternative that these diseases do not have any effect on the clinical symptoms of CU68. Autoimmune diseases occurring in patients with CU, especially thyroid disease, may be an important therapeutic target, but further research is needed to determine the extent to which therapy for concomitant autoimmune diseases influences the clinical course of CU.