Hives are an allergic reaction to external and internal irritants. It looks like redness of certain areas of the skin, accompanied by rashes and blisters, reminiscent of a burn. It is often accompanied by itching, fever and other symptoms. In children, the disease is less common, but it has a more pronounced, recurrent form.
1.What is idiopathic urticaria?
Hives
is a skin reaction that most people have experienced at least once in their lives.
Most often, itching and skin rashes have specific causes (which can range from foods eaten and plant odors to liver disease, parasites or exposure to cold). Atypical diseases of unclear, purely individual origin are considered idiopathic. Thus, idiopathic urticaria
is itchy skin that has no specific cause.
Idiopathic urticaria can develop in a person of any age and social status, in any climate zone, and is one of the most common diseases. 25% of cases of causeless skin allergies become chronic.
There is no consensus on the causes of idiopathic urticaria, but most doctors are inclined to the hypothesis that antibodies are not working correctly, which for some reason begin to attack their own body and thereby disrupt its immune status.
A must read! Help with treatment and hospitalization!
General notes on therapy
Treatment Goals
- regression of rashes;
- no relapses.
Diet.
- In case of a proven food allergy, it is recommended to avoid eating foods that provoke the development of the disease. Eliminating identified allergens from the diet leads to an improvement in the condition of the skin after 24-48 hours.
- In patients with daily or almost daily urticaria, it is recommended that a hypoallergenic diet be included in the extensive evaluation plan. In the case of a pseudo-allergic reaction, improvement with a hypoallergenic diet occurs after 3 weeks.
Pharmacological drugs
.
- Non-sedating 2nd generation H1-histamine blockers are recommended as basic first-line therapy for acute and chronic urticaria.
- The use of 1st generation H1-histamine blockers is currently limited due to their low effectiveness and the risk of side effects (sedation, anticholinergic effects, sleep disorders, etc.) and is indicated only in a number of exceptional cases.
- Treatment of acute urticaria with glucocorticosteroid drugs is not recommended. Indications for the use of systemic glucocorticosteroids are: lack of effect when treated with H1 receptor blockers, delayed urticaria due to pressure, angioedema.
- It is not recommended to use, due to very low evidence of effectiveness: H2-receptor blockers (both monotherapy and in combination with H1-histamine blockers), montelukast, zafirlukast, tranexamic acid, sodium cromoglycate, topical corticosteroids, colchicine, indomethacin, nifedipine.
Indications for hospitalization
to the dermatological hospital: widespread urticaria, accompanied by intense itching and a disturbance in the general condition, as well as lack of effect at the outpatient stage of therapy. to the intensive care unit: concomitant angioedema in the larynx, anaphylactic reactions
Requirements for treatment results
- stopping the appearance of fresh rashes;
- complete resolution of existing rashes;
- absence of subjective manifestations of the disease.
Prevention
Prevention of urticaria involves a thorough analysis of the allergy history before prescribing drug treatment. Particular attention should be paid to the manifestations of atopy in patients with urticaria. For preventive purposes, the use of 2nd generation H1-histamine blockers is recommended [8]. For patients with chronic urticaria, it is important to sanitize foci of chronic infection, treat concomitant pathologies, and also limit the effect of potential allergens.
Acute urticaria
- Eliminate exposure to trigger factors.
- Carry out drug therapy aimed at relieving the symptoms of the disease:
- treatment with H1-histamine receptor blockers;
- if there is no effect, treatment with systemic glucocorticosteroid drugs;
- urgent measures to relieve angioedema.
Chronic urticaria
- Elimination of exposure to factors that cause exacerbation of the disease (if possible).
- Hypoallergenic diet with the exclusion of suspected allergens and/or obligate allergens. When eliminating a food allergen from the diet, the condition improves after 1-2 days. When the rashes disappear, a gradual introduction of excluded or new foods begins, one at a time, one every other day, until new rashes appear. The ineffectiveness of the elimination diet for 1 month indicates the absence of a connection between urticaria and food products and serves as an indication for canceling the elimination diet.
- Drug therapy aimed at reducing symptoms of the disease.
Algorithm for drug treatment of patients with chronic urticaria.
| First line of therapy: | H1-histamine blockers 2nd generation |
| Symptoms persist for 2 weeks | |
| Second line of therapy: | Increasing the dose of 2nd generation H1-histamine blockers by 4 times* |
| Symptoms persist for 1-4 weeks | |
| Third line of therapy: | Omalizumab |
| A short (maximum 10-14 days) course of glucocorticosteroid drugs can be administered at any time. Indication: severity of exacerbation | |
* it is required to justify the prescription in doses exceeding those specified in the instructions for the use of drugs, to invite the patient or his legal representative to sign an informed consent, explaining the benefits and risks of such a prescription, to approve the prescription by a medical commission.
2nd generation H1-histamine blockers are effective in 40-60% of patients with chronic spontaneous (idiopathic) urticaria. If there is no effect from treatment with them for 2 weeks, a 4-fold increase in the dose of drugs is possible. Increasing the dose of H1-histamine receptor blockers allows you to limit the use of glucocorticosteroid drugs and, thus, avoid side effects of therapy and steroid resistance.
Features of the treatment of individual forms of urticaria
- Cold urticaria
. Patients should avoid sudden exposure to cold temperatures. 2nd generation antihistamines (rupatadine) can be used. Systemic glucocorticosteroid drugs are ineffective. - Delayed pressure urticaria
. Pressure on the skin should be avoided. For severe delayed urticaria from pressure, the most effective are systemic glucocorticosteroid drugs, which are prescribed for a short period of time with a gradual reduction in dose. Histamine H1 receptor blockers are usually ineffective. - Solar urticaria
. Antihistamines and ultraviolet light irradiation in gradually increasing doses are effective (tolerance induction). Adequate photoprotection (UVA+UVB) is important. - Urticarial dermographism
. No treatment is required unless the patient consistently responds to minimal trauma. 1st generation H1-histamine receptor blockers are effective. In some cases, the disease is severe and continuous therapy with 2nd generation antihistamines is required. - Cholinergic urticaria
. Patients should avoid intense physical activity. 1st and 2nd generation H1-histamine receptor blockers are used. Belladonna alkaloids/phenobarbital/ergotamine and radobelin/phenobarbital/ergotamine are indicated for the treatment of cholinergic urticaria. - Contact urticaria.
Avoid contact with provoking factors. Antihistamines are effective methods of therapy. Preventive administration of 2nd generation H1 histamine blockers is acceptable in cases of possible contact with trigger factors (for example, insect bites). Topical glucocorticosteroid drugs may be prescribed. For severe manifestations of the disease, systemic glucocorticosteroid drugs are used. - Thermal, aquagenic, vibration urticaria.
Antihistamines are not always effective. - Angioedema
. With the development of angioedema, epinephrine is administered parenterally (intravenously, intramuscularly or subcutaneously, depending on the severity and location of the lesion) and H1-histamine receptor blockers (intravenously or intramuscularly). If this therapy is ineffective and in cases of the development of severe angioedema with a violation of the general condition, systemic glucocorticosteroid drugs are used. In cases of difficulty breathing, aminophylline is used. - Adrenergic urticaria.
Avoid contact with provoking factors, oral propranolol. Nonspecific therapy, including tranquilizers and antihistamines.
Treatment regimens
1. 2nd generation H1-histamine receptor blockers
- Loratadine 10 mg orally 1 time per day until the rash disappears and 4 weeks after the rash disappears
- desloratadine 5 mg orally once a day until the rash disappears and 4 weeks after the rash disappears
- fexofenadine 180 mg orally 1 time per day until the rash disappears and 4 weeks after the rash disappears
- Cetirizine 10 mg orally once daily or 5 mg orally twice daily until the rash disappears and 4 weeks after the rash disappears
- Levocetirizine 5 mg orally once a day until the rash disappears and 4 weeks after the rash disappears
- ebastine 10-20 mg orally 1 time per day (depending on the severity of symptoms) until the rash disappears and 4 weeks after the rash disappears
- Rupatadine 10 mg orally once a day until the rash disappears and 4 weeks after the rash disappears.
2. First generation H1-histamine receptor blockers
- diphenhydramine 25-50 mg orally 4-6 times a day or 20-50 mg intramuscularly 1-2 times a day for 7-10 days
- clemastine 1 mg orally 2 times a day or 2 mg intramuscularly 2 times a day for 7-10 days chloropyramine 25 mg orally 1-2 times a day or 20-40 mg intramuscularly 1-3 times a day for 7-10 days
- cyproheptadine 2-4 mg orally 3-4 times a day for 7-10 days
3. Glucocorticosteroid drugs
- betamethasone 1-2 ml intramuscularly with an interval of 7-10 days, 1-2 injections
- dexamethasone 4-16 mg per day intravenously or intramuscularly until pronounced clinical improvement occurs, with further transition to oral administration (except for the treatment of angioedema)
- dexamethasone 1.5-4.5 mg per day orally until pronounced clinical improvement occurs, with a further gradual dose reduction of 0.125-0.25 mg once a week until complete withdrawal
- prednisolone 30-100 mg per day intravenously or intramuscularly until pronounced clinical improvement occurs, with further transition to oral administration (except for the treatment of angioedema)
- prednisolone 10-30 mg per day orally until pronounced clinical improvement occurs, with a further gradual reduction in dose by 2.5-5 mg once a week until complete withdrawal.
4. Adrenergic agonists
For severe urticaria and/or angioedema (laryngeal edema, exercise-induced anaphylaxis, severe cold allergy), epinephrine, a solution of 0.1% (0.1 to 0.3 ml), is administered subcutaneously or intramuscularly, if necessary, the administration is repeated after 10 -20 minutes up to 3 times.
5. Omalizumab
The drug is indicated for the treatment of chronic idiopathic urticaria, resistant to therapy with H1-histamine receptor blockers, in patients aged 12 years and older. The recommended dose of the drug for chronic idiopathic urticaria is 300 mg subcutaneously every 4 weeks. It is recommended that the attending physician periodically evaluate the need for continued treatment. The effect of omalizumab, as a rule, can be observed already in the first day, with its subsequent increase over a number of weeks. According to clinical studies and real clinical practice, the effectiveness of omalizumab reaches 90%.
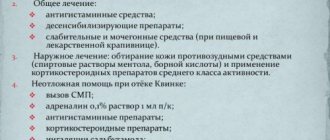
Treatment of angioedema (Quincke's edema)
- epinephrine, solution 0.1%: 0.1-0.5 ml intravenously or intramuscularly, or subcutaneously once;
- chloropyramine, or clemastine, or diphenhydramine 1-2 ml intravenously or intramuscularly once;
- prednisolone 60-100 mg intravenously or intramuscularly or dexamethasone 8-16 mg intravenously or intramuscularly until pronounced clinical improvement;
- aminophylline 10 ml of 2.4% solution intravenously, slowly, once.
Related treatments
In the treatment of urticaria, drugs that affect the central nervous system are used as concomitant therapy: anxiolytics (tranquilizers) and antidepressants.
1. Anxiolytics (tranquilizers) for cholinergic urticaria:
- Hydroxyzine 25 mg orally 4 times a day with meals for 7-10 days
- belladonna alkaloids/phenobarbital/ergotamine 1 tablet orally 2-3 times a day for 1 month
- radobelin/phenobarbital/ergotamine 1 tablet orally 3 times a day for at least 1 month.
2. Antidepressants as concomitant therapy for patients with urticaria in the presence of depression and anxiety.
- amitriptyline 25-50 mg orally 1 time per day for at least 1 month.
3. External therapy. To reduce itching and burning, use warm showers and baths, lotions, shaken suspensions with menthol, anesthetics that do not contain glucocorticosteroid drugs.
Open recommendations
- Some experience has been accumulated in the use of cyclosporine A in combination with 2nd generation H1 histamine blockers for chronic urticaria.
- There are few studies showing the effectiveness of plasmapheresis in chronic urticaria of autoimmune origin.
- The latest consensus documents on the treatment of urticaria also recommend leukotriene receptor blockers, 2nd generation H1 histamine blockers in combination with omalizumab, ketotifen, dapsone, sulfasalazine, oxatamide, nifedipine, warfarin, intravenous gammaglobulin, autologous plasma, montelukast. However, this therapy has low-quality evidence, with no efficacy data from high-quality randomized clinical trials (CDs) [26–29, 34–43].
Treatment of pregnant women and during lactation
When managing pregnant and lactating women, you should adhere to rules similar to those when managing children. It is important to avoid the use of any systemic drug during pregnancy, especially in the first trimester, but the most effective treatment should be ensured. There are indications of an increase in histamine levels in pregnant women, which determines the need for the use of antihistamines. Prescription of 2nd generation H1-histamine blockers during pregnancy should only be used if necessary, when the expected benefit to the mother outweighs the possible risk to the fetus. In the first trimester, medications should be avoided.
A low dose of loratadine may be used for a short time. Use of 1st generation H1-blockers immediately before birth may cause respiratory depression and other side effects in newborns.
To date, there is not a single indication in the world of congenital pathology in children born to women who took 2nd generation H1-histamine blockers (cetirizine, loratadine) during pregnancy. It is advisable to prescribe loratadine to pregnant women with urticaria; recommendations for loratadine can be extrapolated to desloratadine. Recent clinical observations have shown that the safest drugs during pregnancy are loratadine, and during lactation, loratadine and cetirizine [45].
Treatment during lactation.
It is necessary to avoid taking medications during breastfeeding. If necessary, loratadine and cetirizine can be used.
Treatment of children
In children, acute urticaria is more often recorded, which can manifest itself as an allergic reaction, for example, to food. The disease usually develops within an hour after eating food and resolves within 24 hours. Chronic urticaria is less common among children than among adults. In childhood, the most commonly reported urticaria are pressure urticaria and cold urticaria, which are often combined with dermographic or cholinergic urticaria. In most cases, the positive effect of therapy is achieved by taking antihistamines and eliminating trigger factors. For children, 1st line of therapy is recommended, similar to that for adults. It is important to consider the age restrictions and age dosages of each of the H1-histamine blockers:
- loratadine: children aged 2 to 12 years with body weight less than 30 kg - 5 mg 1 time per day, children over 12 years old, and also with body weight more than 30 kg - 10 mg 1 time per day;
- Levocetirizine: children aged 2 to 6 years - 2.5 mg per day, children over 6 years - 5 mg per day;
- Cetirizine: children over 6 years of age (weighing more than 30 kg) - 1 tablet 1 time per day.
Desloratadine, fexofenadine, rupatadine are approved for use in children aged 12 years and older. In infants and children under 2 years of age, first generation H1-histamine receptor blockers can be prescribed. In rare cases, the use of systemic glucocorticosteroid drugs is allowed (for 3-5 days ) .
2.Symptoms of urticaria
Usually urticaria appears quite clearly. These are, first of all, skin disorders:
- itching and swelling of the skin;
- watery blisters;
- small purple rashes.
In severe cases, when large areas of skin are affected, an exacerbation may be accompanied by general malaise, sleep disturbances, headaches, chills, and neurotic disorders
caused by itchy skin.
Most often, idiopathic urticaria differs from other skin allergies by prolonged exacerbations, which can last up to one and a half months
. However, starting with small spots and blisters, urticaria lesions can merge with each other, forming larger zones.
Severe skin itching, in addition to purely cosmetic problems, is the main, very unpleasant and unsafe symptom of this disease. Constant daytime irritation causes serious psycho-emotional trauma, sometimes forcing the patient to take sedatives. Involuntary scratching during sleep is no less dangerous, since it carries the risk of infection of the resulting wounds and scratches. When the blisters are injured, a clear liquid is usually released, and then a dry crust forms, which also itches.
Visit our Dermatology page
Chronic urticaria in children
Particular attention must be paid to the appearance of symptoms in children. It is in them that local lesions can quickly progress and take on a generalized form (spread throughout the body). At the same time, in 90-95% of cases it is almost impossible to identify the cause of the disease.
In children, chronic urticaria can last for years. At the same time, periods of remission tend to increase with age:
- in 50% remission occurs after 6 months;
- in 40% within 8 years;
- Just under 2% of all patients will suffer from recurrent manifestations of the disease for 25 years or more.
If your child has been diagnosed with chronic urticaria, hidden areas of the body should be examined periodically, because rashes most often appear in the armpits and groin.
With primary manifestations of urticaria in children, you should not rely on chance. You should undergo a full examination with him and identify the allergen2,3,5.
3. Diagnosis of rashes
Idiopathic urticaria can only be diagnosed by an allergist.
.
To do this, he prescribes a series of examinations, the purpose of which is to identify the connection of skin manifestations with specific factors and causes, the elimination of which could prevent the development or exacerbation of urticaria. The patient undergoes the following tests:
- general clinical blood test;
- biochemistry;
- HIV testing;
- blood for the Wasserman reaction;
- general urine analysis;
- blood and feces to identify parasites and helminths.
An important diagnostic step is a conversation with the patient
, during which the possible dependence of skin rashes on food, chemicals, stress, heredity, and medications taken is clarified.
Sometimes it is recommended to keep a symptomatic diary
, where each exacerbation of urticaria is recorded. In this case, the patient should try to remember any previous factors that could affect the state of the body, and also write them down. Sometimes only such records allow us to trace a certain pattern.
If a significant period of careful observation does not give a clear picture, there are no chronic diseases and exacerbations are unsystematic, then a diagnosis of “idiopathic allergy” is made.
About our clinic Chistye Prudy metro station Medintercom page!
Diet for urticaria
During the treatment of urticaria caused by food intolerance, it is necessary to avoid eating foods that stimulate the release of histamine. These include:
- coffee, chocolate, honey;
- citrus fruits, nuts;
- products containing dyes, emulsifiers, preservatives;
- milk, chicken eggs;
- baking, mayonnaise, mushrooms, peas;
- chicken, spices, vinegar;
- soybeans, beans, pineapples and some others.
Strong tea, coffee and alcohol should also be avoided. Procedures such as freezing, cooking, and peeling help to slightly reduce the allergenicity of products.
The basis of the diet for allergic urticaria should be porridge cooked in water, vegetarian and cereal soups, baked apples, olive oil, compotes, kefir.
If the patient does not know what foods he has an allergic reaction to in the form of urticaria, he can act as follows:
- After eliminating the symptoms of the disease, do not eat anything for one day.
- From the second day, start eating one product at a time. At the same time, keep a food diary and monitor your condition.
When treating urticaria, it is important to drink a lot - at least two to three liters of water per day. This helps remove allergens from the body faster.
Methods of treatment with traditional methods
The following methods will help relieve itching, soothe the skin and speed up the healing of blisters.
Honey and horseradish:
- Mix honey and horseradish juice in a 1:1 ratio.
- Take the resulting mixture 1 tsp. 3 times a day.
Mint tincture:
- Pour 20 grams of boiling water over it. mint, leave for several hours.
- Strain and take 3 tbsp. l. in a day.
Mint decoction for lotions:
- Pour 30 gr. fresh nettle leaves 2 tbsp. water.
- Bring to a boil and simmer over low heat for 2 minutes.
- Leave for one hour, strain.
- Soak gauze in the infusion and apply to the sore spot several times a day.
hives in a child photo
Where is it localized?
Urticaria, the symptoms of which are difficult to miss, can affect a variety of areas of the body, but is most often localized on the hands: on the fingers and the backs of the hands.
Blisters can also often be observed in the flexures of joints and fat folds. Sometimes the rash is localized on the legs, buttocks, back and abdomen. The most troublesome thing is hives on the face. The skin here is especially sensitive, so itching and burning are felt most acutely. Added to all the unpleasant sensations is the fact that the rash on the face significantly spoils the appearance, and, unlike other parts of the body, it is impossible to hide the face. The use of foundation, powder and other concealing agents is undesirable, since the rash may worsen from contact with certain cosmetic components.
Causes of urticaria
Acute, new-onset or chronic induced urticaria may be a reaction to a viral infection, medication, food, exercise, intense sunlight, contact with animals, cosmetics, chemicals (such as latex or nickel), or may be caused by other causes.
Acute urticaria may be one of the manifestations of a parasitic infection. But since, according to WHO, parasite infections are not widespread in our region, when deciding whether to schedule an examination, it is necessary to take into account risk factors and other manifestations of infection (visiting regions with a high risk of becoming infected, eating raw fish or meat, the presence of gastrointestinal complaints). -intestinal tract, blood eosinophilia and others).
Most cases of chronic urticaria have no external causes.
Under the influence of external factors or without external causes, histamine and other substances are released from mast cells, swelling and itching of the skin begins, and rashes appear. Isolation can be caused by different types of immunological reactions. These may be allergic reactions, reactions caused by the influence of complement or immune complexes. Chronic urticaria is usually associated with autoimmune reactions, but there is no reliable test to accurately determine this.
Advantages of NEARMEDIC clinics
The NEARMEDIC network of clinics will provide you with effective assistance because:
- any clinic has certified adult and pediatric allergists on staff who will conduct a preliminary examination, prescribe laboratory tests and provide professional treatment;
- our Diagnostic Center provides laboratory services of guaranteed quality, which is confirmed by the appropriate certificate;
- The Laboratory Diagnostics Center is equipped with the most modern equipment for conducting all types of examinations and analyses;
- Any data about the patient obtained during the examination and treatment is confidential and is not transferred to other persons.
Allergists have extensive experience in successfully treating acute and chronic allergic diseases. If symptoms appear, please contact one of the network clinics in a timely manner using a general telephone number or through the call back form on the website.