The article was checked by rheumatologist Borodin O.O. , is for general informational purposes only and does not replace specialist advice. For recommendations on diagnosis and treatment, consultation with a doctor is necessary.
- At the Yauza Clinical Hospital, laboratory (coagulogram, increased levels of the enzyme antistreptolysin-O, IgA) and instrumental (biopsy) research methods are used to diagnose hemorrhagic vasculitis (Henoch-Schönlein disease, purpura).
- Based on the results of the examination, as well as taking into account the clinical picture of the disease, the rheumatologist will develop an individual treatment regimen for the patient, if necessary, using innovative methods of extracorporeal hemocorrection.
- 140 cases per 1 million population - incidence rate of hemorrhagic vasculitis
- More than 60% of cases of hepatitis in adults are accompanied by involvement of the joints, 50% of the kidneys, and 65% of the digestive tract.
- In 95% of cases, timely treatment of Henoch-Schenelein disease contributes to the patient’s complete recovery
sign up for a consultation
About the development of the disease
Hemorrhagic vasculitis or Schenelein-Henoch disease is a disease in which autoimmune damage to small arteries occurs - they become fragile, their permeability increases, which causes impaired microcirculation, microthrombosis, multiple small hemorrhages (hemorrhages) as in the skin (hemorrhagic rashes on the skin and mucous membranes) , and in internal organs (gastrointestinal tract, kidneys, joints).
Most often the disease develops in childhood (6-7 years), but can also affect adults. Boys get sick 1.5 times more often than girls.
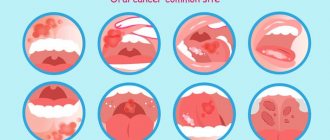
Typical localization of hemorrhagic rash
Photo
The most common place for hemorrhagic rashes to occur is the legs.
However, the rash can also appear on other areas, for example, as shown in the picture below, on the face:
Photo
The rash, when it appears on the legs, is usually localized not on the front surface, and has a fairly symmetrical pattern, as can be seen in the photo:
Photo
But there are often cases when a rash on the body appears on the thighs or buttocks:
Causes
The exact cause of hemorrhagic vasculitis (HV) has not yet been clarified, however, most scientists are inclined to the multi-etiological theory of the development of pathology. The leading factors provoking the development of the disease are:
- viral and bacterial infections,
- chronic infections,
- food or drug allergies,
- vaccines.
The mentioned reasons provoke a malfunction of the immune system, which begins to produce pathogenic immune complexes (IgA) that affect the inner lining of small vessels and contribute to the development of inflammation and microthrombosis.
Pigment
Pigment spots on the skin are spots that appear as a result of an increase or decrease in the amount of melanin pigment. In case of increased pigmentation, the spots are called hyperpigmented, in case of lack of pigment or its absence, depigmented or hypopigmented.
Hyperpigmented spots on the skin are divided into:
- congenital (these include birthmarks, lentigo);
- acquired (freckles, chloasma).
Depigmented spots are divided into:
- congenital (for example, albinism);
- acquired (vitiligo, leucoderma).
Secondary depigmentation can occur in patients with psoriasis, eczema, rosea or pityriasis versicolor at the site of the primary painful rash. These rashes turn pale against the background of tanned areas of the skin because in the area of inflammation, the ability of melanocytes to produce pigment is weakened. Such areas of depigmentation are called secondary leukoderma, or pseudoleukoderma.
Symptoms of hemorrhagic vasculitis
There are several forms of hepatitis B:
- Skin or simple : characterized by the appearance of a specific itchy rash on the lower extremities and buttocks (small pinpoint hemorrhages that rise above the skin and do not disappear with pressure). Over time, the red rash darkens and disappears, leaving areas of increased pigmentation.
- Joint: patients complain of pain in the area of large joints (knees, elbows, hips), their swelling and dysfunction.
- Abdominal : nausea and vomiting, severe abdominal pain (often cramping), possible intestinal bleeding, development of intestinal gangrene (due to thrombosis).
- Renal : urine becomes pink or red due to the admixture of red blood cells, its quantity decreases, protein appears in tests, which are signs of the development of glomerulonephritis and the threat of developing chronic renal failure.
- Fulminant : characterized by the development of DIC syndrome and high blood loss.
Often the disease begins with an increase in body temperature to 38-390C, and patients also note general weakness and increased fatigue. Characteristic wave-like course of the disease.
Skin rashes in children: rashes, exanthemas, enanthemas
Rashes on the skin (exanthema, exanthema ) and mucous membranes (enanthema, enanthema ) can occur not only with viral and bacterial infections, but also with diseases of a non-infectious nature.
It is important to decide whether these changes represent a primary injury to the child's skin or whether the clinical signs have changed due to secondary factors (infection, trauma, or treatment). Examination by a pediatric dermatologist Moscow - Markushka clinic.
Elements of rashes in a child, children. Primary and secondary elements
There are primary and secondary elements of rashes. Primary elements are classified as roseola, spot, papule, nodule, wheal, vesicle, vesicle, hemorrhage. Secondary elements include pigmentation and depigmentation, scale, crust, erosion, crack, abrasion, ulcer, scar, cicatricial atrophy, lichenification, vegetation.
Primary elements of rashes in a child, children: roseola, spot, erythema, hemorrhage, pinpoint hemorrhages - petechiae, papule, tubercle, node, blister, vesicle, bubble
Roseola is a pale pink or red speck ranging in size from 1 to 5 mm. The shape is round or irregular, the edges are clear or blurred, does not protrude above the skin level, disappears when the skin is pressed and stretched. Roseola occurs in many infectious diseases, especially typhoid fever. Multiple roseola 1-2 mm in size are usually described as a pinpoint rash (with scarlet fever), in the process of resolution they become covered with scales or disappear without a trace.
The spot (makula) has the same color as roseola, size - from 5 to 20 mm, does not protrude above the skin level. The shape is most often incorrect. The spot disappears when pressure is applied to the skin and appears again after the pressure is removed. Multiple spots ranging in size from 5 to 10 mm are described as a small-spotted rash (for example, with rubella - a child is vaccinated against rubella at the Markushka children's clinic). Spots 10-20 mm in size form a large-spotted rash (for example, with measles, allergies - examined by a pediatric allergist in Moscow, Markushka clinic).
Erythema is large areas of hyperemic skin that are red, purple-red, or purple in color. It occurs as a result of the fusion of large spots formed by the dilation of blood vessels not only of the papillary layer of the skin, but also of the subpapillary vascular plexus. Spots larger than 20 mm that tend to coalesce should be considered erythema. Erythema is most typical for erysipelas, thermal, and ultraviolet burns .
Hemorrhage (haemorrhagia) is bleeding into the skin as a result of destruction of skin vessels. It looks like dots or spots of various sizes and shapes and does not disappear when the skin is stretched. The color is initially red, purple or violet, then, as the hemorrhage resolves, it becomes yellow-green and finally yellow (formation of hemosiderin during the breakdown of red blood cells). Color changes are clearly visible in larger hemorrhages.
Pinpoint hemorrhages are called petechiae (petechia). Multiple round hemorrhages measuring 2 to 5 mm are described as purpura . Irregular hemorrhages measuring more than 5 mm are called ecchymoses . Hemorrhages may overlap with other elements of the rash. In such cases, they speak of petechial transformation of roseolas, spots, papules. As a rule, this is observed in severe cases of the disease. Hemorrhagic rashes are detected with typhus (often in combination with roseola - roseola-petechial rash), hemorrhagic fevers, and sepsis. Hemorrhagic elements of irregular shape on a dense basis (stellate rash) are characteristic of meningococcemia and pneumococcal sepsis. Minor hemorrhages can also have a non-infectious origin (capillary toxicosis, toxic-allergic vasculitis, vitamin deficiency C, etc.).
Papule (papula) is an element of the rash that rises above the level of the skin, which is often determined by touch. It has a flat or dome-shaped surface, size - from 1 to 20 mm. The shape and color are the same as those of roseolas and spots. Papules often leave behind pigmentation and flaking of the skin. Papules that merge with each other form plaques, and when the latter merge, areas appear that are located on large areas of the skin, the size of a palm or more. Often, during a routine clinical examination of a child, it is very difficult or even completely impossible to distinguish roseola from papules. On the other hand, the same sick child can simultaneously have roseola, papules (typhoid fever, paratyphoid fever, infectious mononucleosis), papules and spots (measles - child measles vaccination, children's medical).
A tubercle (tuberkulum) is a limited, dense, cavityless formation protruding above the surface of the skin with a diameter of 1-2 to 5-10 mm. The tubercles are formed as a result of the accumulation of a specific inflammatory infiltrate in the dermis. Clinically, the tubercle is similar to a papule, but differs from it in that when palpating the tubercle, a dense infiltrate in the skin is always clearly visible. In addition, tubercles, unlike papules, undergo necrosis during reverse development, often form ulcers and leave behind a scar or cicatricial atrophy of the skin. The tubercles are most typical of cutaneous leishmaniasis, leprosy and tuberculous skin lesions, tertiary and late congenital syphilis.
A node (nodus) is a cavityless, limited compaction that goes deep into the skin, often standing above the skin level. The size of the knots ranges from a hazelnut to a chicken egg and more. They are formed as a result of the accumulation of cellular infiltrate in the subcutaneous tissue and the dermis itself. Inflammatory nodules have a soft or doughy consistency, unclear boundaries, and the skin over them is red. Nodules that appear as a result of specific inflammation (colliquatic tuberculosis, syphilitic gumma) have a dense consistency, are sharply demarcated from the surrounding tissues, and are prone to decay and ulceration with subsequent scarring.
A blister (urtica) is an acutely inflammatory, cavity-free element slightly elevated above the skin level, measuring from 2-3 to 10-15 cm or more, has a round or oval shape, and is often accompanied by itching. Color - from white to pale pink or light red. The blister usually forms quickly and disappears quickly, leaving no trace behind. It occurs as a result of limited acute inflammatory swelling of the papillary layer of the skin and simultaneous expansion of the capillaries. The appearance of urticarial elements is characteristic of allergic reactions of various origins (drug, food, cold allergies), including those of an infectious nature. Sometimes occurs in the pre-icteric period of hepatitis B (vaccination of a child against hepatitis in the Markushka children's clinic).
A vesicle (vesicula) is a cavity element measuring from 1 to 5 mm, representing a detachment of the epidermis. Usually the bubbles are filled with transparent, cloudy or bloody contents, they can shrink and give a transparent or brown crust. If the cover of the bubble is opened, then erosion is formed - a wet surface of pink or red color limited by the size of the bubble. The bubbles do not leave any scars on the skin. If a large number of leukocytes accumulate in a vesicle, it turns into an abscess - a pustule. Inflammatory changes are noted at the base and around the vesicle. Pustules are divided into single-chamber (chickenpox) and multi-chamber (natural smallpox). A group of blisters located on inflamed skin is called herpes. Vesicles are characteristic of herpes and enterovirus infections, chickenpox and natural pox. Chickenpox vaccination - Markushka Children's Clinic.
Bubble (bulla) is a cavity element with a diameter of up to 3-5 cm, located in the upper layers of the epidermis and under the epidermis. The contents of the blisters can be serous, bloody, or purulent. They can collapse, forming a crust, or open up, forming an erosive surface that turns into unstable pigmentation. The bubble occurs more often against the background of an erythematous spot, less often - against the background of unchanged skin (neonatal pemphigoid). The elements can be located both inside the epidermis, in the styloid layer (pemphigus vulgaris), and under the epidermis (multiform exudative erythema, dermatosis herpetiformis). It is observed with bullous form of erysipelas, sometimes with chicken pox, thermal burns.
Secondary elements of rashes in a child, children: hyperpigmentation, depigmentation, scales, erosion, abrasion, ulcer, cracks, tears, crust, scar, lichenification, vegetation
Secondary morphological elements are formed as a result of the evolution of the primary elements of the rash .
Hyperpigmentation (hyperpigmentatio) is a change in skin color as a result of an increase in melanin in it or the deposition of hemosiderin of primary elements.
Depigmentation (depigmentatio) occurs as a result of a decrease in the melanin content in the skin, observed after the disappearance of a nodule, tubercle - resolution of spotty-flaky (pityriasis versicolor, eczematoids) and papular (psoriasis) elements.
Scale (sguama) is an accumulation of rejected cells of the stratum corneum, sometimes the underlying layers of the epidermis. Scales occur on primary morphological elements - papules (psoriasis, syphilis), tubercles, after the resolution of blisters (eczema), etc.
Erosion (erosio) is a skin defect within the epidermis as a result of the opening of a vesicle, blister, or abscess, repeating their shape and size. When vesicles and pustules merge, erosions have scalloped edges. Erosion can also occur as a result of maceration of the skin in the area of folds or during maceration of other elements of the rash, most often papules. When erosion heals, there is no scar left; usually there is only temporary pigmentation.
An abrasion (excoriatio) is a violation of the integrity of the skin that occurs as a result of scratching, scratching, or other damage. Abrasions can be superficial - within the epidermis, sometimes involving the papillary dermis, and heal without a scar. Deeper abrasions, involving the deeper layers of the dermis, leave behind a scar. Abrasions are characterized by a tendency to become infected.
An ulcer (ulcus) is a deep skin defect that reaches the dermis, subcutaneous fat, fascia, muscles, and bones. It occurs as a result of the breakdown of the tissue of the primary element (tubercle, node, ecthyma). Its size is from 1 mm to the size of a coin or palm and more; the shape can be round, oval, linear, oblong, irregular. The surrounding tissue is either inflamed (edema, hyperemia) or infiltrated. Ulcers always heal with the formation of scars.
Cracks, tears (fissura, rhagades) - linear damage to the skin in the form of its rupture, resulting from excessive dryness due to loss of elasticity due to inflammatory infiltration or overstretching of the skin. Cracks can be located within the epidermis and dermis. They are usually localized in the corners of the mouth, interdigital folds, on the palms, soles, above the joints, and in the anus. A superficial crack after healing leaves no traces. After healing of deep cracks, linear scars remain.
A crust (crusla) is formed on the skin as a result of drying of the discharge of a weeping surface (vesicle, vesicle, abscess, ulcer, erosion). The crusts can have different colors (with serous exudate, transparent with a yellowish tint; with purulent exudate, yellow, greenish or brown; with hemorrhagic exudate, brown or black) and shape (layered, oyster-like, etc.).
A scar (cicatrix) is the formation of connective tissue at the site of a deep defect. Occurs after healing of deep skin defects at the site of ulcerated tubercles, deep pustules, nodes, deep burns, wounds. Scar formation is accompanied by the death of sebaceous and sweat glands, hair follicles, blood vessels and elastic fibers, and the disappearance of the skin pattern. Typically, scars are located below the skin level or are at its level, less often they rise above the skin level - hypertrophic scars.
Lichenification (lichenificatio) is a focus of increased skin pattern, accompanied by thickening and compaction, hyperpigmentation, and dryness. Foci of lichenification are most often localized in the neck, elbow and popliteal folds, wrist and ankle joints, inguinal folds, scrotum and occur in chronic dermatoses accompanied by itching (eczema, neurodermatitis).
Vegetation (vegetatio) is a papillary thickening of the skin that occurs as a result of the growth of the styloid layer of the epidermis and papillomatosis of the dermis during a long-term inflammatory process. More often it forms in the area of papular elements and ulcers. Vegetations can erode, bleed, and are prone to secondary infection.
Diagnosis of hemorrhagic vasculitis
At the Yauza Clinical Hospital, patients with suspected Henoch-Schönlein disease are prescribed the following set of examinations:
- general blood analysis;
- general urine analysis;
- coagulogram;
- determination of the level of antistreptolysin-O, IGA in peripheral blood;
- tissue biopsy of the affected organ or part of the body, followed by histological examination of the biopsy.
To make a diagnosis of hemorrhagic vasculitis, the patient must have two or more diagnostic criteria:
- specific rashes not associated with low platelet levels;
- manifestation of the disease before the age of 20 years;
- widespread abdominal pain that worsens after eating, intestinal bleeding;
- granulocytic infiltration of the walls of microvasculature vessels, which is confirmed histologically.
Diagnostic methods
Since in children the disease manifests itself with bright, acute symptoms from the very beginning, there are, as a rule, no problems with making a diagnosis. Diagnosis of hemorrhagic vasculitis in adults is much more difficult, especially in the absence of a characteristic rash at the onset of the disease. As a rule, it is based on laboratory tests, which include:
- blood tests - general, biochemical, coagulogram;
- urine examination for hematuria, proteinuria, cylindruria, Nechiporenko and Zimnitsky tests, biochemical analysis;
- stool test for the presence of blood.
An important stage of diagnosis, which allows us to establish the degree of damage to internal organs, is instrumental studies - ultrasound of the abdominal cavity and kidneys, ultrasound of the renal vessels, gastroscopy. In severe cases of the disease, a biopsy of the skin and kidneys is prescribed to determine the size of immunoglobulin deposits and the permeability of the vascular wall.
Therapeutic measures
At the Yauza Clinical Hospital, treatment of hemorrhagic vasculitis is aimed at achieving the following goals:
- elimination of clinical signs of pathology;
- reducing the risk of complications;
- preventing damage to vital organs;
- complete recovery of the patient or achievement of stable long-term remission.
To do this, our rheumatologist develops an individual treatment regimen for each patient, which includes:
- bed rest for at least 3 weeks;
- avoiding contact with allergens;
- diet therapy;
- prescribing enterosorbents, antihistamines, antispasmodics, hemostatic agents and antiplatelet agents;
- in some cases, the use of hormones and cytostatics is justified.
To reduce the destructive influence of circulating immune complexes and enhance the effectiveness of drug therapy, patients with hepatitis B undergo extracorporeal hemocorrection.
Treatment of purpura
To bring the skin condition back to normal, ordinary ointments or creams are not enough. Treatment of a hemorrhagic spot requires accurate diagnosis to exclude other diseases with similar symptoms.
Self-treatment of purpura with dubious means or with the help of traditional medicine does not give the expected result and can be dangerous for the body.
When you seek medical help at our medical and aesthetic center, you receive qualified assistance from experienced specialists. To diagnose pathology, we use modern laboratory tests.
Treatment of the disease includes a comprehensive selection of drugs, which may include antibiotics, hormonal therapy, antihistamines, anticoagulants, and drugs to support the immune system. The selection of medications is carried out on an individual basis, taking into account the patient’s health condition.
Our specialists will also develop a number of preventive measures to adhere to diet and daily routine in order to prevent recurrence of the disease in the future.