Urea is the end product of protein breakdown, which is excreted from the body of mammals to protect the body from nitrogen intoxication. It is found in the blood and in many body tissues, including skin cells. Urea makes the skin soft as it is a natural moisturizer. If there is not enough of it in the skin, the epidermis becomes dry and begins to peel off.
Among the active ingredients in cosmetics, urea is one of the most common. For the beauty industry, it is obtained artificially by synthesizing carbon monoxide and ammonia. Urea is a natural substance for the human body, and therefore has low allergenicity. Cosmetics with urea act quickly and effectively, having an immediate effect on the condition of the skin.
Silk foot cream with powder Silky Cream, 100 ml
Super Moisture foot cream, 100 ml
Intensive Moisture Cream with urea, 150 ml
Express moisturizing mist with urea 10% Moisture Mist, 150 ml
Super-hydration and regeneration face cream with 10% urea and snail mucin, 150 ml
Super-moisturizing and restoring face cream with urea 10% and prebiotics, 150 ml
Super moisturizing hand balm with urea (10%) Super Velvet Balm, 300 ml
Foam softener for removing calluses and corns with urea (20%) Liquid Pedicure, 200 ml
Renewing cream with PHA acids and urea (10%) Acid-renew Cream, 550 ml
Lifting cream with collagen and urea (10%) Moisture-Collagen Cream, 550 ml
Moisturizing cream with ceramides and urea (10%) Cera-moisture Cream, 550 ml
What effects do cosmetics with urea have?
- Powerful moisturizing and softening effect.
- Exfoliation of dead skin cells, fight against hyperkeratosis.
- Renewal - skin becomes smooth and looks younger.
- Light antiseptic, deodorizing and anti-inflammatory effect.
- Urea penetrates deep into the skin, so it is a good conductor for other active ingredients.
When purchasing products with urea, be sure to take into account its concentration - the intensity of the product’s impact depends on this.
Concentration up to 10% - light moisturizers.
Suitable for normal to slightly dry skin. Such creams are an excellent moisturizing product and are most often used to care for the face, hands and body. Help prevent peeling and make the skin more elastic.
Concentrations from 10 to 20% are products with a clear keratolytic and powerful moisturizing effect.
Capable of causing active exfoliation of dead skin cells. Necessary for those prone to hyperkeratosis, rough and dry skin, dry calluses and corns. Urea in a concentration of up to 15% is used in skin care products for the face, hands, feet and body, more than 15% - for the feet and for very dry skin of the hands.
Concentrations from 20% are strong keratolytic agents that are used as an SOS agent or used in a short course.
Urea in high concentration is a classic and indispensable component of salon pedicure products. This concentration is often used for intensive action in home care for problem feet: with very dry skin, peeling, severe hyperkeratosis, corns, calluses, cracks, and diabetic foot syndrome.
Topical use of urea in skin care: a review
Leonardo Celleno, Catholic University of the Sacred Heart, Rome, Italy, WILEY Dermatological Therapy, July 19, 2022, DOI: 10.1111/dth.12690
Impaired barrier function has been associated with a number of skin diseases, including xerosis, atopic dermatitis and psoriasis. Urea, a component of the skin's natural moisturizing factor, plays an important role in maintaining skin hydration and integrity. Several studies have examined the effects of urea in clinical settings. In this article, we summarize the available clinical evidence on the effects of urea in maintaining skin health and treating skin diseases. At lower doses (≤10%), topical urea preparations act as a skin moisturizer, while at higher concentrations (>10% urea), urea-based preparations have a keratolytic effect. (eg, Aquapiling (aquapiling.net)) Urea is also useful in combination therapy with anti-inflammatory and antifungal drugs due to its activity as a penetration enhancer.
KEYWORDS
atopic dermatitis, ichthyosis vulgaris, keratolytic agent, moisturizer, onychomycosis, psoriasis, topical urea, xerosis
The role of the skin is to protect the body from harmful environmental influences while maintaining appropriate mechanical properties, including elasticity. Healthy skin is characterized by effective control of water loss, allowing it to maintain a good level of hydration and therefore a strong physical and chemical barrier (Verdier-Sévrain & Bonté, 2007).
Urea is a polar, hygroscopic molecule produced endogenously by the human body and found naturally in the skin. Urea is formed from the metabolism of proteins and other organic nitrogen compounds and is excreted in urine and sweat (Kapuscinska & Nowak, 2014; Mosher, 1933). As one of the components of natural moisturizing factor (NMF), urea helps maintain healthy skin hydration levels. Despite the constant discovery of new ingredients and new skin care formulations, urea still remains one of the most useful molecules available to dermatologists due to its molecular and functional characteristics. In this article, we present a review of the clinical evidence supporting the use of urea to maintain skin integrity and treat diseases associated with skin barrier dysfunction.
The stratum corneum (SC), the outermost layer of the skin, protects the body from external agents and controls exchanges with the environment, especially transepithelial water loss (TEWL). The structural organization of the stratum corneum and the presence of hygroscopic molecules, collectively called NMF, allow the stratum corneum to retain water, thus keeping the epidermis hydrated and elastic. The stratum corneum consists of terminally differentiated keratinocytes called corneocytes, which are arranged in dense layers and are united by corneodesmosomes. Corneocytes are embedded in a hydrophobic lipid extracellular matrix, the keratinized cell envelope (Pouillot, Dayan, Polla, Polla, & Polla, 2008). Although the barrier created by the stratum corneum is similar in structure to a brick wall, it is more dynamic and complex in nature (Elias, 1983). In fact, the keratinized cell membrane surrounding the nondividing keratin-filled corneocytes represents an active environment consisting of enzymes involved in epidermal differentiation and NMF formation (Pouillot et al., 2008).
Adequate levels of hydration are necessary to maintain skin mechanical properties such as strength, flexibility, and elasticity (Mojumdar, Pham, Topgaard, & Sparr, 2017). In vivo, normal hydration levels range from 30–50% of the dry weight of the stratum corneum (Caspers, Lucassen, Carter, Bruining, & Puppels, 2001). Water found in the stratum corneum is mainly absorbed by corneocytes, which can increase their weight when swollen by up to 50% (Richter, Müller, Schwarz, Wepf, & Wiesendanger, 2001; Mojumdar et al., 2017). Under low relative humidity (RH) conditions, the stratum corneum is brittle and brittle, becoming more elastic as relative humidity increases (Mojumdar et al., 2017). Changes in relative humidity also alter the mobility of keratin filaments present in corneocytes, thereby supporting the role of water in keratin plasticization (Mojumdar et al., 2017).
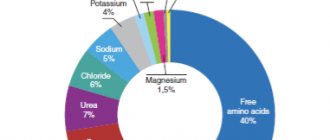
NMF is critical to maintaining a healthy stratum corneum as it plays an important role in skin hydration (Robinson, Visscher, Laruffa, & Wickett, 2010). A decrease in NMF levels causes water loss in the stratum corneum and reduces the elasticity of the epidermis (Verdier-Sévrain & Bonté, 2007). NMF consists of molecules that are formed from the breakdown of proteins or are secreted by the sebaceous and sweat glands. The detailed composition of NMF is depicted in Figure 1. Degradation of filaggrin, a keratin-aggregating protein of the keratinized cell membrane that is formed during keratinocyte differentiation (Simon et al., 1996; Kezic, Kammeyer, Calkoen, Fluhr, & Bos, 2009), results in the formation of hygroscopic amino acids and other by-products including urea (Björklund et al., 2014). In a healthy stratum corneum, urea corresponds to 7% NMF, a percentage that decreases with age (Verdier-Sévrain & Bonté, 2007).
NMF components (%)
Clockwise: free amino acids; pyrrolidonecarboxylic acid; lactate; Sahara; urea; chlorides; sodium; potassium; ammonia, uric acid, glucosamine, creatinine; calcium; phosphates; citrate and formate.
FIGURE 1 Chemical composition of NMF. Data from (Verdier-Sévrain & Bonté, 2007)
The moisturizing effects of urea have been studied in vivo for many years (Serup, 1992; Bettinger, Gloor, Gehring, & Wolf, 1995; Treffel & Gabard, 1995; Loden, 1996, 1997; Kuzmina, Hagströmer, & Emtestam, 2002); Grether-Beck, Mühlberg, Brenden, & Krutmann, 2008; Borelli, Bielfeldt, Borelli, Schaller, & Korting, 2011). Pan and colleagues analyzed these clinical data in 2013 (Pan, Heinecke, Bernardo, Tsui, & Levitt, 2013). Urea has been noted to reduce transepidermal water loss (Loden, 1996, 1997; Borelli et al., 2011), improve hydration (Borelli et al., 2011) and water retention (Treffel & Gabard, 1995). In addition, urea can increase the amount of free water under high humidity conditions (Bettinger et al., 1995) and act as a powerful skin moisturizer and exfoliant (Serup, 1992).
Of note is the fact that all of these clinical studies used topical cream, emulsion or foam formulations with a urea concentration of 10% or less. No adverse events were reported, confirming the safety of topical urea-based products.
Urea increases the water content of the stratum corneum, acting as a humectant but also by maintaining the fluidity of the stratum corneum (Albèr et al., 2014; Mojumdar et al., 2017). By measuring corneometry, Albèr et al. found that urea promoted skin hydration even when used in a formulation with reduced water activity (Albèr et al., 2014). A subsequent study examined the molecular characteristics of keratin and macroscopic properties of the stratum corneum (SC) after the addition of urea to dehydrated SCs and corneocytes and found that the changes were similar to those occurring with increasing relative humidity in the absence of urea (Mojumdar et al., 2017) . These data support the hypothesis that urea acts as a natural endogenous humectant, replacing water under low-humidity conditions and maintaining fluid levels within the stratum corneum (Mojumdar et al., 2017). At higher concentrations (>10%) (eg Aquapiling (aquapiling.net)) urea has an emollient/keratolytic effect. The first evidence came from Swanbeck's studies in the 60s. These studies showed that preparations with high concentrations of urea could be used to treat ichthyosis and other hyperkeratotic conditions (Swanbeck, 1968a, 1968b; Swanbeck & Rajka, 1970). Swanbeck suggested that at high concentrations, urea is able to dissolve keratin, promoting the destruction of hydrogen bonds. Further studies showed that urea can cause conformational changes in keratin, causing denaturation of the protein structure (Pan et al., 2013).
In addition to its moisturizing properties, preserving the fluidity of SK and promoting keratin denaturation, urea is also able to participate in the regulation of gene expression (Friedman, von Grote, & Meckfessel, 2016). In a study by Grether-Beck et al. indicates that urea induces the expression of epidermal genes (Grether-Beck et al., 2012). Although more research is needed to better understand the involvement of urea in the regulation of gene expression in SK, the active role of urea as an inducer of epidermal gene expression may explain the beneficial effects of urea in preserving skin barrier function.
Keratinization disorders are characterized by qualitative or quantitative changes in the structure of the stratum corneum. Urea, used alone or in combination therapy, improves the treatment of pathological conditions including xerosis, atopic dermatitis, ichthyosis vulgaris, psoriasis and onychomycosis (Pan et al., 2013).
Xerosis or dry skin may be the result of dehydration or changes in lipid production. Dehydrated skin, typical of older people, whose tissues lack water - thin, weak and fragile. Low sebum levels and abnormal lipid levels in the epidermis (as in atopic dermatitis) make the skin tender, opaque, red, and hypersensitive to external agents. In both cases, topical formulations containing urea play an important role in the treatment of diseases. When used in low doses (mostly <10%, one study used 40% urea), urea regulates transepidermal water loss (TEWL) and restores the ability of the stratum corneum to mobilize and maintain hydration (Pan et al., 2013; Danby et al., 2016). Moisturizers containing urea improve fissure healing in diabetic patients (Federici, Federici, & Milani, 2015; Gin et al., 2017). Open heel cracks allow bacteria to enter and can lead to infections and further complications. Additionally, a skin care routine that includes a moisturizing step stops the progression of dry skin diseases, including epidermal hyperproliferation and inflammation (Friedman, von Grote, & Meckfessel, 2016).
From top to bottom, left to right: topical urea formulations; ≤10% urea, moisturizing effect, positive effect on xerosis, AD, IV, psoriasis; ≥10% urea, keratolytic effect, positive effect on psoriasis, onychomycosis; useful in quality; monotherapy; combination therapy, urea – enhances the penetration of corticosteroids, salicylic acid and antifungal drugs.
FIGURE 2 Overview of known effects of topical urea formulations in clinical settings. AD, topical dermatitis; IV, ichthyosis vulgaris
Skin barrier dysfunction has been associated with an increased risk of developing atopic dermatitis (AD) (Egawa & Kabashima, 2018). A weakened skin barrier makes it easier for allergens and other external agents to penetrate and predisposes the body to inflammation. If skin inflammation persists, barrier function is further compromised (Egawa & Kabashima, 2018). AD is the most common inflammatory skin disease, affecting up to 30% of children worldwide (Bieber, 2008). AD is a cutaneous manifestation of a genetic predisposition to allergies and is characterized by highly itchy and recurrent skin lesions on dry skin (Egawa & Kabashima, 2018). Adequate hydration of the stratum corneum appears to be critical in preventing AD, as the use of moisturizers in neonates reduces the prevalence of the disease (Horimukai et al., 2014; Simpson et al., 2014).
Several clinical trials have examined the clinical effects of topical urea formulations in AD (Pan et al., 2013). At a concentration of 10%, urea has been found to improve skin hydration and reduce transepidermal water loss (TEWL) in patients with AD (Sasaki, Tadaki, & Tagami, 1989). However, two recent studies suggest that urea increases skin hydration in AD without reducing TEWL (Hoppe et al., 2015; Ahmad Nasrollahi et al., 2018). These conflicting results can be explained by the low concentration of urea used in the formulations used (only 5%).
Clinical benefit of urea in AD has been observed when used alone and in combination with hydrocortisone or betamethasone-17 valerate (Bohnsack, Tausch, Gassmuller, & Rippke, 1997; Wilhelm, Scholermann, & Bohnsack, 1998; Loden et al., 2002; Wirén et al. al., 2009; Pan et al., 2013). It should be noted that combination therapy with urea was more effective than treatment with hydrocortisone or betamethasone-17-valerate alone (Pan et al., 2013). A recent Cochrane review confirmed that for AD, treatment with moisturizers and topical corticosteroids is more effective than treatment with topical corticosteroids alone (Van Zuuren, Fedorowicz, & Arents, 2017). A systematic review confirmed the beneficial effects of moisturizers on AD but warned of the need for more focused studies that would allow direct comparisons of moisturizers (Lindh & Bradley, 2015). Meanwhile, available evidence supports the use of urea-containing moisturizers as first-line therapy for AD (Lindh & Bradley, 2015).
Ichthyosis vulgaris (IV) is a genetic disorder with a prevalence of 1:300 caused by loss-of-function mutations in the filaggrin gene (FLG) (Brown & McLean, 2012). IV is characterized by flaky, dry skin with symmetrical white or gray scales. Peeling occurs due to the absence of filaggrin protein in the stratum corneum, which causes low cellular regeneration of the stratum corneum and chronic accumulation of keratin. A recent systematic review concluded that urea-containing drugs should be used as first-line therapy for ichthyosis vulgaris (Lindh & Bradley, 2015). Maintenance therapy using 10% urea is noninferior to therapy containing 1% hydrocortisone, 2% salicylic acid, or paraffin moisturizers (Pan et al., 2013).
Psoriasis is a chronic inflammatory skin disease with a worldwide prevalence of 2% (Parisi, Symmons, Griffiths, & Ashcroft, 2013). Psoriasis is characterized by the development of erythematous scaly plaques that result from increased keratinocyte proliferation and altered epidermal differentiation (Zhang et al., 2009). Clinical trials have been conducted to study the effects of urea on psoriatic skin (Pan et al., 2013). One study found that, when used at a concentration of 10%, urea reduced transepidermal water loss (TEWL) and increased stratum corneum hydration (Sasaki, Tadaki, & Tagami, 1989). Subsequently, Hagemann and Proksch also found that urea induces epidermal differentiation (Hagemann & Proksch, 1996). When used at concentrations ranging from 10 to 40%, alone or in combination with bifonazole or dithranol, most studies reported improvement in desquamation and clinical status in patients with psoriasis (Pan et al., 2013). (for example, Aquapiling (aquapiling.net))
At a concentration of 40%, urea shows clinical effects in the treatment of fungal nail infections such as onychomycosis (Pan et al., 2013). Topical treatment with fluconazole 1% and urea 40% is more effective than fluconazole alone in the treatment of onychomycosis (Bassiri-Jahromi, Ehsani, Mirshams-Shahshahani, & Jamshidi, 2012). Urea enhances the penetration of the antifungal agent and thus enhances the therapeutic effect (Pan et al., 2013). (for example, Cream-paste for corns Aquapiling (aquapiling.net))
Urea can be considered a penetration enhancer due to its ability to facilitate the transport of molecular flow through the nail and skin (Trommer & Neubert, 2006). These molecules include the aforementioned antifungal drugs, as well as other compounds used in the treatment of skin diseases, such as corticosteroids (Trommer & Neubert, 2006). An earlier study by Ayres and Hooper examined the potentiating effects of urea on skin penetration of cortisol (Ayres & Hooper, 1978). The authors observed that a topical formulation containing 1.0% cortisol and 10% urea delivered eight times more cortisol to the skin than a topical cream used as a control (1.0% cortisol cream mixed with water). Subsequent studies showed that urea enhances the penetration of hydrocortisone, progesterone and leuprolide through the subcutaneous tissue (Trommer & Neubert, 2006). It is noteworthy that in an in vitro study examining transcutaneous diffusion of progesterone, urea increased progesterone penetration by 2.5-fold (Valenta & Wedenig, 1997).
The mechanism by which urea increases the permeability of the stratum corneum is not fully understood, but it is thought to be related to the ability to increase the water content absorbed by corneocytes, which is a direct consequence of its high water-binding capacity (Mueller et al., 2016). At higher doses, the keratolytic action of urea may also play a role in enhancing drug penetration (Trommer & Neubert, 2006). Because of its recognized action as a chemical penetration enhancer, urea should be used in conjunction with topical corticosteroids, salicylic acid, or antifungals to improve drug delivery and treatment outcomes.
Urea is a well-known moisturizer and keratolytic agent. Urea has been used safely for over a century to support skin health and treat a range of skin conditions. Clinical studies have confirmed the positive effect of urea in diseases associated with skin barrier dysfunction. When used in different concentrations, urea has different effects (Fig. 2). Lower concentrations of urea (≤10%) are associated with a moisturizing effect, whereas higher concentrations (>10%) have an emollient/keratolytic effect. As a skin penetration enhancer, urea facilitates the crossing of the skin barrier by other molecules and thus improves the action of drugs used in combination therapy. Topical formulations containing urea are available in a variety of concentrations and provide clinicians with a wide range of alternatives to enhance the treatment of skin conditions and improve patient well-being.
Medical writing and editing support was provided by Raquel Carvalhosa, Ph.D., and . Financial support for the compilation and editing of medical texts was provided by.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ORCID Leonardo Celleno https://orcid.org/0000-0002-7129-198X
REFERENCES
Ahmad Nasrollahi, S., Ayatollahi, A., Yazdanparast, T., Samadi, A., Hosseini, H., Shamsipour, M., … Firooz, A. (2018). Comparison of linoleic acid-containing water-in-oil emulsion with urea-containing water-in-oil emulsion in the treatment of atopic dermatitis: A randomized clinical trial. Clinical Cosmetic and Investigational Dermatology, 11, 21–28. https://doi.org/10.2147/CCID.S145561 Albèr, C., Buraczewska-Norin, I., Kocherbitov, V., Saleem, S., Lodén, M., & Engblom, J. (2014). Effects of water activity and low molecular weight humectants on skin permeability and hydration dynamics—a double-blind, randomized and controlled study. International Journal of Cosmetic Science, 36(5), 412–418. https://doi.org/10.1111/ics.12136 Ayres, P. J., & Hooper, G. (1978). Assessment of the skin penetration properties of different carrier vehicles for topically applied cortisol. British Journal of Dermatology, 99(3), 307–317. https://doi.org/10.1111/j. 1365-2133.1978.tb02002.x Bassiri-Jahromi, S., Ehsani, A.H., Mirshams-Shahshahani, M., & Jamshidi, B. (2012). A evaluation comparative of combination therapy of fluconazole 1% and urea 40% compared with fluconazole 1% alone in a nail lacquer for treatment of onychomycosis: Therapeutic trial. Journal of Dermatological Treatment, 23(6), 453–456. https://doi. org/10.3109/09546634.2011.588191 Bettinger, J., Gloor, M., Gehring, W., & Wolf, W. (1995). Influence of emulsions with and without urea on water-binding capacity of the stratum corneum. Journal of the Society of Cosmetic Chemists, 46(5), 247–254. Bieber, T. (2008). Atopic dermatitis. New England Journal of Medicine, 358(14), 1483–1494. https://doi.org/10.1056/NEJMra074081 Björklund, S., Andersson, J. M., Pham, Q. D., Nowacka, A., Topgaard, D., & Sparr, E. (2014). Stratum corneum molecular mobility in the presence of natural moisturizers. Soft Matter, 10(25), 4535–4546. https://doi. org/10.1039/C4SM00137K Bohnsack, K., Tausch, I., Gassmuller, J., & Rippke, F. (1997). Efficacy on the symptom “dry skin” and long-term dermal tolerance of Laceran lotion 10% urea in patients with atopic dermatitis. Zeitschrift für Hautkrankheiten, 72, 34–39. Borelli, C., Bielfeldt, S., Borelli, S., Schaller, M., & Korting, H. C. (2011). Cream or foam in pedal skin care: Towards the ideal vehicle for urea used against dry skin. International Journal of Cosmetic Science, 33(1), 37–43. https://doi.org/10.1111/j.1468-2494.2010.00576.x Brown, S. J., & McLean, W. H. I. (2012). One remarkable molecule: filaggrin. The Journal of Investigative Dermatology, 132(3 Pt 2), 751–762. https://doi.org/10.1038/jid.2011.393 Caspers, P. J., Lucassen, G. W., Carter, E. A., Bruining, H. A., & Puppels, G. J. (2001). In vivo confocal Raman microspectroscopy of the skin: Noninvasive determination of molecular concentration profiles. The Journal of Investigative Dermatology, 116(3), 434–442. https://doi. org/10.1046/j.1523-1747.2001.01258.x Danby, S. G., Brown, K., Higgs-Bayliss, T., Chittock, J., Albenali, L., & Cork, M. J. (2016). The effect of an emollient containing urea, ceramide NP, and lactate on skin barrier structure and function in older people with dry skin. Skin Pharmacology and Physiology, 29(3), 135–147. https://doi.org/10.1159/000445955 Egawa, G., & Kabashima, K. (2018). Barrier dysfunction in the skin allergy. Allergology International, 67(1), 3–11. https://doi.org/10.1016/j.alit. 2017.10.002 Elias, P. M. (1983). Epidermal lipids, barrier function, and desquamation. The Journal of Investigative Dermatology, 80(Suppl), 44s–49s. Federici, A., Federici, G., & Milani, M. (2015). Use of a urea, arginine and carnosine cream versus a standard emollient glycerol cream for treatment of severe xerosis of the feet in patients with type 2 diabetes: A randomized, 8 month, assessor-blinded, controlled trial. Current Medical Research and Opinion, 31(6), 1063–1069. https://doi.org/10. 1185/03007995.2015.1037731 Friedman, A. J., von Grote, E. C., & Meckfessel, M. H. (2016). Urea: A clinically oriented overview from bench to bedside. Journal of Drugs in Dermatology: JDD, 15(5), 633–639. Gin, H., Rorive, M., Gautier, S., Condomines, M., Saint Aroman, M., & Garrigue, E. (2017). Treatment by a moisturizer of xerosis and cracks of the feet in men and women with diabetes: A randomized, double-blind, placebo-controlled study. Diabetic Medicine, 34(9), 1309–1317. https://doi.org/10.1111/dme.13402 Grether-Beck, S., Felsner, I., Brenden, H., Kohne, Z., Majora, M., Marini, A., … Krutmann, J. (2012). Urea uptake enhances barrier function and antimicrobial defense in humans by regulating epidermal gene expression. Journal of Investigative Dermatology, 132(6), 1561–1572. https://doi. org/10.1038/jid.2012.42 Grether-Beck, S., Mühlberg, K., Brenden, H., & Krutmann, J. (2008). Urea plus ceramides and vitamins: Improving the efficacy of a topical urea preparation by addition of ceramides and vitamins. Der Hautarzt; Zeitschrift Fur Dermatologie, Venerologie, Und Verwandte Gebiete, 59(9), 717–718, 720–723. https://doi.org/10.1007/s00105-008-1594-z Hagemann, I., & Proksch, E. (1996). Topical treatment by urea reduces epidermal hyperproliferation and induces differentiation in psoriasis. Acta Dermato-Venereologica, 76(5), 353–356. Hoppe, T., Winge, M. C. G., Bradley, M., Nordenskjöld, M., Vahlquist, A., Törmä, H., & Berne, B. (2015). Moisturizing treatment of patients with atopic dermatitis and ichthyosis vulgaris improves dry skin, but has a modest effect on gene expression regardless of FLG genotype. Journal of the European Academy of Dermatology and Venereology, 29(1), 174–177. https://doi.org/10.1111/jdv.12333 Horimukai, K., Morita, K., Narita, M., Kondo, M., Kitazawa, H., Nozaki, M., … Ohya, Y. (2014 ). Application of moisturizer to neonates prevents development of atopic dermatitis. The Journal of Allergy and Clinical Immunology, 134(4), 824–830.e6. https://doi.org/10.1016/j.jaci.2014.07.060 Kapuscinska, A., & Nowak, I. (2014). The use of urea and its derivatives in the cosmetics industry. CHEMIK, 68(2), 91–98. Kezic, S., Kammeyer, A., Calkoen, F., Fluhr, J. W., & Bos, J. D. (2009). Natural moisturizing factor components in the stratum corneum as biomarkers of filaggrin genotype: Evaluation of minimally invasive methods. British Journal of Dermatology, 161(5), 1098–1104. https:// doi.org/10.1111/j.1365-2133.2009.09342.x Kuzmina, N., Hagströmer, L., & Emtestam, L. (2002). Urea and sodium chloride in moisturisers for skin of the elderly—a comparative, double-blind, randomized study. Skin Pharmacology and Applied Skin Physiology, 15(3), 166–174. https://doi.org/10.1159/000063545 Lindh, J. D., & Bradley, M. (2015). Clinical effectiveness of moisturizers in atopic dermatitis and related disorders: A systematic review. American Journal of Clinical Dermatology, 16(5), 341–359. https://doi.org/10. 1007/s40257-015-0146-4 Loden, M. (1996). Urea-containing moisturizers influence barrier properties of normal skin. Archives of Dermatological Research, 288(2), 103–107. Loden, M. (1997). Barrier recovery and influence of irritant stimuli in skin treated with a moisturizing cream. Contact Dermatitis, 36(5), 256–260. Loden, M., Andersson, A.-C., Anderson, C., Bergbrant, I.-M., Frödin, T., Ohman, H., … Lindberg, M. (2002). A double-blind study comparing the effect of glycerin and urea on dry, eczematous skin in atopic patients. Acta Dermato-Venereologica, 82(1), 45–47. Mojumdar, E. H., Pham, Q. D., Topgaard, D., & Sparr, E. (2017). Skin hydration: Interplay between molecular dynamics, structure and water uptake in the stratum corneum. Scientific Reports, 7(1), 15712. https:// doi.org/10.1038/s41598-017-15921-5 Mosher, H. H. (1933). Simultaneous study of constituents of urine and perspiration. Journal of Biological Chemistry, 99, 781. Mueller, J., Oliveira, J. S. L., Barker, R., Trapp, M., Schroeter, A., Brezesinski, G., & Neubert, R. H. H. (2016). The effect of urea and taurine as hydrophilic penetration enhancers on stratum corneum lipid models. Biochimica et Biophysica Acta (BBA) - Biomembranes, 1858(9), 2006–2018. https://doi.org/10.1016/j.bbamem.2016.05.010 Pan, M., Heinecke, G., Bernardo, S., Tsui, C., & Levitt, J. (2013). Urea: A comprehensive review of the clinical literature. Dermatology Online Journal, 19(11), 20392. Parisi, R., Symmons, D. P. M., Griffiths, C. E. M., & Ashcroft, D. M. (2013). Global epidemiology of psoriasis: A systematic review of incidence and prevalence. Journal of Investigative Dermatology, 133(2), 377–385. https://doi.org/10.1038/jid.2012.339 Pouillot, A., Dayan, N., Polla, A. S., Polla, L. L., & Polla, B. S. (2008). The stratum corneum: A double paradox. Journal of Cosmetic Dermatology, 7(2), 143–148. https://doi.org/10.1111/j.1473-2165.2008.00379.x Richter, T., Müller, J. H., Schwarz, U. D., Wepf, R., & Wiesendanger, R. (2001). Investigation of the swelling of human skin cells in liquid media by tapping mode scanning force microscopy. Applied Physics A, 72(S1), S125–S128. https://doi.org/10.1007/s003390100750 Robinson, M., Visscher, M., Laruffa, A., & Wickett, R. (2010). Natural moisturizing factors (NMF) in the stratum corneum (SC). I. Effects of lipid extraction and soaking. Journal of Cosmetic Science, 61(1), 13–22. Sasaki, Y., Tadaki, T., & Tagami, H. (1989). The effects of topical application of urea cream on the function of pathological stratum corneum. Acta Dermatol-Kyoto, 84(4), 581–586. Serup, J. (1992). A three-hour test for rapid comparison of effects of moisturizers and active constituents (urea). Measurement of hydration, scaling and skin surface lipidization by noninvasive techniques. Acta Dermato-Venereologica. Supplementum, 177, 29–33. Simon, M., Haftek, M., Sebbag, M., MontéZin, M., Girbal-Neuhauser, E., Schmitt, D., & Serre, G. (1996). Evidence that filaggrin is a component of cornified cell envelopes in human plantar epidermis. Biochemical Journal, 317(1), 173–177. https://doi.org/10.1042/bj3170173 Simpson, E. L., Chalmers, J. R., Hanifin, J. M., Thomas, K. S., Cork, M. J., McLean, W. H. I., … Williams, H. C. (2014). Emollient enhancement of the skin barrier from birth offers effective atopic dermatitis prevention. Journal of Allergy and Clinical Immunology, 134(4), 818–823. https:// doi.org/10.1016/j.jaci.2014.08.005 Swanbeck, G. (1968a). A new treatment of ichthyosis and other hyperkeratotic conditions. Acta Dermato-Venereologica, 48(2), 123–127. Swanbeck, G. (1968b). Carbamide cream for dry and hyperkeratotic skin. Läkartidningen, 65(22), 2286–2290. Swanbeck, G., & Rajka, G. (1970). Antipruritic effect of urea solutions. An experimental and clinical study. Acta Dermato-Venereologica, 50(3), 225–227. Treffel, P., & Gabard, B. (1995). Stratum corneum dynamic function measurements after moisturizer or irritant application. Archives of Dermatological Research, 287(5), 474–479. Trommer, H., & Neubert, R. H. (2006). Overcoming the stratum corneum: The modulation of skin penetration. A review. Skin Pharmacology and Physiology, 19(2), 106–121. https://doi.org/10.1159/000091978 Valenta, C., & Wedenig, S. (1997). Effects of penetration enhancers on the in-vitro percutaneous absorption of progesterone. Journal of Pharmacy and Pharmacology, 49(10), 955–959. https://doi.org/10.1111/j.2042-7158. 1997.tb06023.x Van Zuuren, E. J., Fedorowicz, Z., & Arents, B. W. M. (2017). Emollients and moisturizers for eczema: Abridged Cochrane systematic review including GRADE assessments. British Journal of Dermatology, 177(5), 1256–1271. https://doi.org/10.1111/bjd.15602 Verdier-Sévrain, S., & Bonté, F. (2007). Skin hydration: A review on its molecular mechanisms. Journal of Cosmetic Dermatology, 6(2), 75–82. https://doi.org/10.1111/j.1473-2165.2007.00300.x Wilhelm, K. P., Scholermann, A., & Bohnsack, K. (1998). Efficacy and tolerance of a topical preparation containing 10% urea in patients with atopic dermatitis. Aktuelle Dermatologie, 24, 26–30. Wirén, K., Nohlgård, C., Nyberg, F., Holm, L., Svensson, M., Johannesson, A., … Lodén, M. (2009). Treatment with a barrier-strengthening moisturizing cream delays relapse of atopic dermatitis: A prospective and randomized controlled clinical trial. Journal of the European Academy of Dermatology and Venereology, 23(11), 1267–1272. https://doi.org/10. 1111/j.1468-3083.2009.03303.x Zhang, X.-J., Huang, W., Yang, S., Sun, L.-D., Zhang, F.-Y., Zhu, Q.- X., ... Liu, J.-J. (2009). Psoriasis genome-wide association study identifies susceptibility variants within LCE gene cluster at 1q21. Nature Genetics, 41(2), 205–210. https://doi.org/10.1038/ng.31
Products with urea for the body
Products with a medium concentration of urea can be applied to the skin of the body to increase its elasticity, firmness and hydration. They are especially indispensable for areas such as elbows and knees. The ARAVIA Professional range includes 3 products with a 10% urea concentration, which are ideal for body skin and solve various aesthetic problems.
- Moisturizing cream with ceramides and urea restores water balance and prevents moisture loss. The formula instantly eliminates dryness and flaking, enhances the protective function and activates the skin regeneration process. Vitamin E in the product has an antioxidant effect. Suitable for both young and mature skin.
- Cream with urea and collagen is intended for dry, dehydrated skin with signs of age-related changes. Its formula provides noticeable lifting and correction of wrinkles, enhances protective functions and retains moisture in the upper layers of the epidermis.
- Cream with urea and PHA acids has a mild keratolytic effect, moisturizes the skin and restores its radiance, restores the protective barrier and prevents transepidermal moisture loss. Indicated for all skin types. It is an excellent post-procedure product due to its exfoliating and regenerating properties that help the skin recover after hair removal or hardware procedures.
Pharmacological properties of the drug Urea
When applied topically, it has a resolving, keratolytic and keratoplastic effect, and has bacteriostatic and fungistatic properties. Local application of urea in the form of a cream does not lead to its absorption into the systemic circulation and an increase in nitrogen content in the body. When taken orally or intravenously, due to the osmotic mechanism, it has a diuretic effect, dehydrating and hypotensive effect, and reduces intraocular pressure. It is not metabolized in the human body and undergoes glomerular filtration in large quantities (50–60%); not reabsorbed.
Products with urea for the face
The optimal amount of urea in facial skin products is 10%. In this concentration, urea performs two actions at once: it intensively moisturizes and has a keratolytic effect. This ensures restoration of water balance and reliable retention of moisture in the stratum corneum for a long time, regeneration and renewal of the skin, and better access for other active components.
Facial cosmetics with urea ARAVIA Professional is a whole range of products that solve many problems:
- Mist “Express Moisturizing”;
- intensively moisturizing cream;
- cream with prebiotics for recovery;
- cream with snail mucin for regeneration.
Each product contains valuable components, the effect of which is enhanced by urea. Indeed, in addition to hydration, the skin needs protection from environmental influences, regeneration, reduction of wrinkles and slowing down the aging process.
The best cream for corns with urea
The Professional SUPER MOISTURE composition from Arabia is sold with a dispenser, which saves its consumption. The ointment has a light texture and is quickly absorbed without leaving an unpleasant shine. It works effectively and the results last a long time.
Characteristics
- amount of urea – 10%;
- dispenser – yes;
- product level – professional;
- manufacturer - Arabia.
pros
- Available in 2 versions - large and small volume;
- softens the surface of the feet, eliminates corns;
- The recipe is specially selected for effective foot care.
Minuses
Not found.
Some consumers also use Arabia ointment for the face. The result of such use can lead to negative consequences.
Products with urea for feet
Foot creams with urea can not only effectively and quickly cope with dryness, cracks and calluses, but also have a deodorizing and antiseptic effect on the skin of the feet. Regular use helps prevent the appearance of dry, keratinized skin, cracks, corns, and makes the skin moisturized, soft and smooth. It is better to use foot products at night and wear special pedicure socks or regular cotton socks.
The ARAVIA Professional assortment includes several creams with urea for feet: super-moisturizing cream, cream with PHA acids and silk cream with powder, as well as a softening foam for removing calluses and corns, which should be used during the pedicure procedure.
Similar drugs:
- Celandine grass (Chelidonii majoris herba) Vegetable raw materials
- Tamsulid Capsule
- Diacarb Oral tablets
- Epletor Oral tablets
- Britomar Oral tablets
- Verospiron Oral tablets
- Hypothiazid Oral tablets
- Lespenephryl Oral solution
- Lipril (Liprilum) Oral tablets
- Horsetail (Equisetum arvense) Vegetable raw materials
** The Drug Directory is intended for informational purposes only. For more complete information, please refer to the manufacturer's instructions. Do not self-medicate; Before starting to use the drug Urea, you should consult a doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal. Any information on the site does not replace medical advice and cannot serve as a guarantee of the positive effect of the drug.
Are you interested in the drug Urea? Do you want to know more detailed information or do you need a doctor's examination? Or do you need an inspection? You can make an appointment with a doctor - the Euro lab is always at your service! The best doctors will examine you, advise you, provide the necessary assistance and make a diagnosis. You can also call a doctor at home . Euro lab clinic is open for you around the clock.
** Attention! The information presented in this medication guide is intended for medical professionals and should not be used as a basis for self-medication. The description of the drug Urea is provided for informational purposes and is not intended for prescribing treatment without the participation of a doctor. Patients need to consult a specialist!
If you are interested in any other drugs and medications, their descriptions and instructions for use, information about the composition and form of release, indications for use and side effects, methods of use, prices and reviews of drugs, or you have any other questions and suggestions - write to us, we will definitely try to help you.
What you need to remember about cosmetics with urea
- The main function of urea in cosmetics is powerful moisturizing.
- At a concentration of 10% or more, urea begins to work as a keratolytic.
- 10% concentration is ideal for face and body care products, 15% for feet and hands, 20% for problem feet. Products containing urea in a concentration of more than 20% can only be recommended by a professional.
- Products with urea should not be used for acne, mechanical damage to the skin and skin infections.
- Urea is a good conductor for other active ingredients.
- The results of products containing urea will be better if applied to slightly steamed and damp skin - this will retain moisture under a thin occlusive film of the cream.
How does urea work in cosmetics?
Urea is used to improve the condition of dry skin. Getting on its surface as part of a cream for the face, hands or feet, urea draws water from the deep layers and “locks” it in the upper keratinized layer. As a result, peeling and a feeling of tightness disappear, the texture on the face and hands is smoothed, and wrinkles are reduced. And the feet get rid of rough “crust” and corns.
This component also serves as a conductor for other ingredients deep into the tissues - it helps the absorption of moisturizing, nourishing and regenerating substances.