Vulvar neoplasms are a pathological condition of uncontrolled cell division, in which there is a proliferation of various types of tissue on the external genitalia.
Benign tumors of the vulva are divided into the following types:
- Myoma is a formation whose structure is formed by muscle fibers. It is characterized by mobility and a dense elastic consistency. It is most often localized deep in the muscles of the labia majora.
- Fibroma has mature connective tissue fibers in its structure. Often has a stalk or base. It is characterized by slow growth and heterogeneous consistency.
- Vulvar papilloma (condyloma) is a consequence of the presence of the human papilloma virus in the body. Formed from cells of connective and epithelial tissues. It often has a dark brown or whitish color, a wide base or knife, and is characterized by papillary growth. It is usually localized at the threshold of the vagina or labia majora. Has a serious risk of malignancy.
- Lipoma is formed from adipose tissue cells. Most often it has a round shape and a pronounced capsule. It is characterized by a soft consistency and low mobility. It is usually localized on the labia majora or pubis.
- Lymphagioma is formed by cells of lymphoid tissue and is a small nodule. It has a bluish tint and soft consistency.
- Vulvar hemangioma is a vascular neoplasm of a reddish or bluish color. Its danger lies in the high risk of germination in the tissue of internal organs - the vagina and uterus.
Causes and risk factors for vulvar cancer
Currently, scientists know two mechanisms for the occurrence of vulvar cancer. In young women (especially smokers), tumors associated with infection with the human papillomavirus are most common. Probably, by penetrating a cell, the pathogen can cause changes in genes that lead to the production of abnormal proteins and, as a result, uncontrolled cell proliferation.
Women over 55 years of age most often do not have HPV infection, but they do have a mutation in the p53 gene, which plays an important role in preventing cancer.
In addition to human papillomavirus infection, other risk factors for vulvar cancer are known:
- Age . Women under 50 account for less than 20% of cases, and women over 70 account for more than 50%.
- Smoking . Traditionally, exposure to tobacco smoke has been associated with an increased risk of lung cancer. But in fact, smoking increases the risk of many cancers.
- HIV infection . The immunodeficiency virus weakens the body's defenses and increases the risk of HPV infection.
- Vulvar intraepithelial neoplasia . It is a precancerous disease. Abnormal cells appear in the vulva area, initially they are in the superficial layers of the skin, but over time they can transform into cancer.
- Diagnosed with cervical cancer . There is an increased risk of vulvar cancer.
Why can’t tumors on the genitals be ignored?
Class Clinic
Practicing gynecologist-oncologist Irina Vladimirovna Shekhovtsova spoke about what neoplasms on the external genitalia are dangerous, what to do if they appear and how to easily remove them.
What neoplasms on the female genital organs do you most often encounter?
Due to the specifics of my work, these are most often diseases of the vulva, anal area, and cervix. One of the most dangerous and scary diseases that you have to deal with is vulvar cancer. Fortunately, such localization of cancer is a fairly rare case, accounting for 2-8% of all diseases affecting the external genitalia. The main thing is that its development can be easily prevented by consulting a doctor in time - when the first signs appear, and this can be almost any neoplasm on the vulva.
What signs of vulvar cancer can a woman detect herself?
I would like to immediately note that it is impossible to suspect vulvar cancer on your own; for this you need to visit a doctor. Symptoms of vulvar cancer, especially in the initial stages, are similar to viral and bacterial inflammation - itching, burning of the external genitalia. The appearance of condylomas is typical, the woman believes that it is a “skin horn”, a dense nodule, “just a compaction”, it happens that such symptoms do not cause concern. It happens that a woman comes to a gynecologist, but he is not alert for cancer and does not diagnose cancer. Next, a dense tumor develops, against the background of the tumor a bleeding ulcer appears, it is very specific, it has uneven dense edges, a necrotic bottom. Women try to treat these ulcers on their own and also do not turn to a specialist, since at this stage of the disease there is no pain. In our country, women go to the gynecologist when something hurts.
What happens if you don’t see a doctor in the initial stages, what are the later signs of the disease?
In such cases, pain begins and is difficult to ignore. The tumor moves from one labia to another, so-called “kissing ulcers” appear. The lymph nodes are affected, the tumor can spread to the vagina, urethra, etc. As a rule, in such cases a diagnosis of vulvar cancer is made.
Any tumor, including this one, begins with an underlying disease and has a precancerous form. There is no cancer without precancer and underlying disease. And our task is to diagnose as early as possible.
Are there any predisposing factors for developing vulvar cancer?
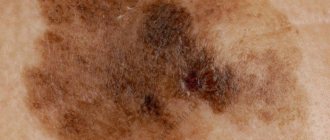
Yes, of course - this is low immunity and diabetes, often insulin-dependent. A risk factor is infection with the human papillomavirus (types 16, 18 and others, there are more than 70 of them, which can provoke the development of cancer). In addition, obesity, tobacco smoking is a very serious factor, promiscuity in sexual relations, non-compliance with personal hygiene standards, crourosis (wrinkling of the labia majora and minora, itching, skin resembles parchment paper) and leukoplakia (signs are the same as crourosis). Dark spots – pigmented nevi – should also alert you. If a dark spot appears on the vulva, which the patient may call a mole, this is an alarm bell, in such cases it is necessary to immediately contact a gynecologist.
Are women who smoke at risk?
Yes, definitely. Women often think that smoking can only cause lung cancer, but this is not true. One of the most powerful factors contributing to the development of both vulvar and cervical cancer is the carcinogens contained in tobacco mixtures. In addition to nicotine, tobacco smoke contains ions of radioactive metals such as cesium, polonium, radium-226 and radium-228, and more than 50 other compounds that can cause cancer. Through the lungs, these substances penetrate the circulatory system and slowly affect the entire body, including the female genital organs.
What diagnostic methods are used to distinguish vulvar cancer from other diseases?
To conduct the study, a small piece of tissue is taken and sent to a morphologist, and the morphologist, in turn, gives a conclusion whether there are malignant cells or not. I would like to note that diseases of the vulva cannot be treated without a preliminary histological examination, without establishing the true causes of the neoplasm and nosology.
In women of what age is this disease more common?
It is cancer that occurs more often in older women, 70 years and older. For some time I worked with this particular age group: women in deep menopause who do not take care of themselves, do not take care of their health and ignore recommendations for the prevention of this disease. There have been a few cases in younger women, over 50 years of age. But in such cases it was about early diagnosis. Such women visit the gynecologist more often, and the gynecologist may diagnose vulvar cancer earlier.
How good is the prognosis with early diagnosis?
In such cases, we can talk about radical and more effective treatment; it is clear that in such a situation a favorable outcome is more likely.
Accordingly, any neoplasms should alert a woman, and in such cases it makes sense to consult a doctor?
Oncological vigilance has never harmed anyone. Even when I was studying, teachers said that a doctor should always look for something bad. It is better to overdiagnose and scare the patient than to miss the disease. I would like to note that in my practice, women with vulvar cancer come late when there is metastasis to the regional lymph nodes, and in such cases the treatment is very difficult, often patients die within a few months. For this disease, surgical treatment involves severe mutilating operations, and reconstructive plastic surgery cannot offer anything, since a huge flap of skin with lymph nodes and subcutaneous fat is removed.
Tell us about tumors that are not malignant.
We have already touched on this topic a little. Condylomas, small papillary growths of the mucous membranes of the genital organs, and papillomas are very common. The main signs are typical for almost all neoplasms: compaction, swelling, inflammation, itching and burning. This applies to both the vulva and vagina.
How are these tumors removed?
Very easy to remove. One of the most effective methods is radio wave. With a special device “Surgitron”, which is equipped in our clinic, it is possible to remove condylomas without the formation of a scar and a weeping surface. The device actually dries out the tumor. Previously, we used electrocoagulators, but this was complicated by a lot of unpleasant sensations; healing took several weeks. There is also laser removal, but with this method histological examination of the tissue is impossible. In addition, it is still possible to remove it using the classical surgical method, but in such cases cosmetic stitches are applied and a slight scar is likely to form.
Make an appointment with Irina Vladimirovna Shekhovtsova on the website or by phone (4012) 33-44-55.
Classification of vulvar cancer
The most common type of vulvar cancer is keratinizing squamous cell carcinoma . As a rule, it develops in older women (over 55 years old). Less common are warty and basaloid (usually in young women), superficial squamous cell carcinomas.
In 8% of cases, malignant tumors of the vulva are represented by adenocarcinomas , which originate from glandular cells. Typically, they develop in the Bartholin glands . These glands are located in the thickness of the labia majora; they moisturize the vagina during sexual intercourse. Tumors of the Bartholin glands are often mistaken for cysts. Sometimes adenocarcinomas develop from cells of the sweat glands, which are located in the area of the external female genitalia.
, basal cell carcinomas can be found in the vulva area .
In 6% of cases, melanomas are found in the vulva area - malignant tumors that originate from cells that produce the pigment melanin. This localization is not entirely typical for melanoma; more often it occurs in open areas of the skin exposed to sunlight.
Classification of vulvar cancer by stages:
- Stage 1 : at stage 1, a tumor that grows within the vulva and does not affect neighboring organs or lymph nodes.
- Stage 2 : In stage 2, the tumor has grown into adjacent structures, such as the urethra, vagina, and anus.
- Stage 3 : Stage 3 is a tumor in which cancer cells have spread to the lymph nodes.
- Stage 4 : with stage 4 vulvar cancer, the damage to the lymph nodes is more pronounced compared to stage 3, tumor growth is observed in the upper part of the urethra, vagina, bladder, rectum, pelvic bones, and the presence of distant metastases.
The stage of the tumor determines treatment approaches and further prognosis.
Find out the exact cost of treatment
Symptoms of benign tumors of the vulva
Until the formation increases in size sufficiently, the woman may not notice it. As they grow, they protrude outward, stretching the adjacent tissues. The result is discomfort:
- sensation of a foreign body in the perineal area;
- discomfort during sexual intercourse;
- inconvenience when moving.
If the tumor is damaged, symptoms such as:
- inflammation;
- suppuration;
- the appearance of ulcers;
- contact bleeding;
- urinary disturbance.
The latter is due to compression of the urethra by the growing formation.
Developing neoplasms of the vulva usually rise in the form of a swelling above the skin. If blood circulation is disrupted or necrosis begins, the woman begins to experience pain.
Symptoms of vulvar cancer
Precancerous changes and early stages of vulvar cancer may have no symptoms. When the tumor grows deeper and cancer cells begin to spread to the lymph nodes, almost all women experience some symptoms:
- An area of skin in the vulva that differs from the surrounding healthy tissue: it may be lighter or darker, reddish or pink.
- A lump, plaque, wart, or ulcer appears on the skin.
- Itching, burning, and pain occur.
- Many women are concerned about bleeding from the vagina outside of menstruation.
Most often, these symptoms are not caused by cancer. But there is always a small chance that it is cancer.
Adenocarcinoma, which develops from the Bartholin gland, appears as a mass in the labia that can be felt. A cyst manifests itself with similar symptoms.
Types of benign tumors of the vulva
As already noted, vulvar tumors can be either benign or malignant. Let's consider what types of benign tumors of the vulva are known to modern gynecology.
- Vulvar fibroids. It is a neoplasm, the structure of which is formed by muscle fibers. There are two types of it:
- rhabdomyoma - fibroid formed by striated fibers;
- leiomyoma - fibroid consisting of smooth muscle fibers.
Among the main characteristics of this type of neoplasm, it is worth highlighting:
- lack of connection with surrounding tissues;
- mobility;
- dense elastic consistency.
Most often, fibroids are found deep in the muscles of the labia majora.
- Vulvar fibroma. It is a formation of mature fibrous connective tissue structures. In some cases, it is represented by bundles of collagen fibrils. Distinctive characteristics of vulvar fibroma: absence of adhesions with surrounding tissues;
- presence of a leg or base;
- slow growth;
- consistency, determined by the degree of compaction of the cytoplasm and the location of collagen bundles.
Typically, fibroma is found deep in the muscles of the labia majora. In some cases, it is localized in front of the vagina.
- dark brown (in some cases whitish);
Papilloma is localized, as a rule, in the vestibule of the vagina or on the labia majora. Its danger lies in the high risk of degeneration into a malignant tumor after spreading to the vaginal mucosa.
- round form;
Lipoma is most often located on the labia majora or pubis.
- bluish tint;
In most cases, lymphagioma is localized in the labia majora.
- yellowish-white color;
Myxoma is usually found in the subcutaneous layer of the pubis or labia majora. This disease is more often diagnosed in postmenopausal women.
- pinkish, yellowish or brown tint;
Hydroadenoma occurs in the area of the labia majora or pubis.
Diagnosis of vulvar cancer
The main method for diagnosing vulvar cancer is biopsy. Examining a tissue sample under a microscope helps to accurately distinguish benign from malignant tumors. In order to understand where to take tissue from, the doctor examines the vulva using a colposcope and treats the skin with a solution of acetic acid or toluidine blue: as a result, pathological foci become more visible.
According to indications (if the tumor is large and there is a suspicion that it has spread beyond the vulva), other diagnostic methods are prescribed:
- Endoscopic examination of the bladder and rectum.
- CT and MRI help to detect foci of tumor growth in the lymph nodes and various organs.
- A chest x-ray is performed to look for metastases in the chest.
- PET scanning is an effective method for searching for distant metastases.
Bartholinitis
It is also a cyst formed due to a blockage of the Bartholin gland. It is necessary to open the cyst before the process of infection and breakthrough begins. This procedure occurs simply on an outpatient basis under local anesthesia. If measures are not taken in time, the inflammatory process can spread to the internal genital organs and lead to serious complications.
Heratsi Medical Center provides paid medical assistance in the removal of papillomas, condylomas, warts and lipomas, as well as the opening of cystic formations of various etiologies.
In our clinic, specialists work only with extensive experience, constantly improving their qualifications, are the authors of scientific works, and have an academic degree. When removing, a Fotek radio knife is used, which is highly accurate and narrows the area of impact as much as possible.
The cost of services can be viewed in the “Price” section or by calling the 24-hour hotline.
Surgical treatment of vulvar cancer
Surgery is the main treatment for vulvar cancer. During the operation, the doctor tries to completely remove the tumor tissue, while maintaining the aesthetic appearance of the genital organs, normal evacuation of urine and stool (this is especially important when the tumor is close to the urethra and anus). Depending on the stage, one of the following surgical options is used:
- Local excision of the tumor. Possibly in the early stages. The surgeon excises the tumor and approximately 1.3 cm of surrounding tissue and subcutaneous fat. The removed tissue is sent to a laboratory for microscopy. No tumor cells should be found at the edges of the incision (negative resection margin) - this will indicate that the tumor has been completely removed, and most likely there are no more cancer cells left in the body.
- Vulvectomy . The surgeon removes all or most of the vulva. There are different options for vulvectomy. In some cases, after surgery, it is possible to maintain the normal appearance of the genital organs; in some women, it is subsequently necessary to resort to reconstructive plastic surgery.
- Evisceration (exenteration) of the pelvis is the most complex and traumatic operation; it is performed if the cancer has spread to the pelvic organs. The bladder, lower part of the colon and rectum, and the uterus along with the cervix and vagina are removed. The volume of intervention depends on where the tumor has managed to grow.
- Removal of lymph nodes . Previously, it was always carried out - just in case, since the surgeon could not know for sure whether the tumor cells had spread to the nearest lymph nodes. Currently, it is possible to conduct a sentinel biopsy - a study of the lymph node, which is the first on the path of lymph outflow from the tumor. If there are no cancer cells in it, then it makes no sense to remove the remaining lymph nodes.
Sometimes, if there is a high risk of relapse after surgery, surgical treatment is combined with a course of radiation therapy and chemotherapy.
Write to an oncologist
Lipomas
Lipomas are formations in the subcutaneous fat layer. Their origin is still not fully understood. There is a possibility of a genetic, hereditary predisposition, but this process cannot be predicted. The size of lipomas ranges from 1 to 15 cm. They do not cause any unpleasant sensations: itching, pain, but they cause inconvenience and cosmetic negatives. They pose a threat to health only if they are damaged by clothing or other mechanical means, which will lead to inflammation.
When treating lipomas up to 3 cm, drug therapy is provided. For larger sizes, lipomas are removed surgically using a radio knife.
Radiation therapy for vulvar cancer
Radiation therapy is used for vulvar cancer in the following cases:
- Before surgery in combination with chemotherapy. This helps to reduce the tumor and convert inoperable cancer into operable one.
- After surgery to prevent relapse.
- Radiation therapy can be used as the only treatment for inguinal and pelvic lymph nodes.
- It is used alone or in combination with chemotherapy to treat women who are contraindicated for surgery.
Classification of pathology
Oncologists distinguish several types of vulvar cancer based on the histological structure of atypical cells. These include:
- melanoma;
- adenocarcinoma;
- Paget's cancer;
- basal cell carcinoma;
- sarcoma;
- squamous cell carcinoma.
The latter is detected in 85% of patients suffering from malignant pathologies of the vulva. The growth pattern of tumors allows oncologists to distinguish exophytic, nodular, ulcerative and infiltrative-edematous tumors.
The use of NNM criteria gives doctors the opportunity to assess the prevalence of the pathological process in a woman’s body (T means a primary tumor without metastases, N - signs of metastasis to regional lymph nodes, M - metastases in distant organs).
Prognosis for vulvar cancer
How long do people live with vulvar cancer?
Even if treatment is successful and remission occurs, the woman remains at risk of cancer recurrence in the future. Therefore, all patients require long-term observation, over several years. Prognosis is assessed by 5-year survival rate, an indicator that shows the percentage of women surviving 5 years after diagnosis. This indicator depends on the stage of the cancer and how much it has spread beyond the vulva:
- For local cancer that is located within the vulva (corresponding to stages I and II), the 5-year survival rate is 86%.
- For regional cancer, when tumor cells have spread to the lymph nodes and neighboring organs (corresponding to stages III and IVA) - 54%.
- For advanced cancer, when there are distant metastases (corresponding to stage IVB) - 16%.
Prognosis for benign tumors of the vulva
Benign neoplasms of the vulva can pose a danger only if they become malignant. However, this happens quite infrequently. Thus, they do not entail a great risk to life and health.
Recurrence of neoplasms is possible, especially when it comes to papillomas. To prevent this, antiviral treatment should be carried out after removal.
In addition, there is a risk of injury during the operation.
Can vulvar cancer be prevented?
The main measures to prevent vulvar cancer are to prevent infection with the human papillomavirus. It is necessary to limit the number of sexual partners (ideally there should be one), use condoms. The vaccine effectively protects against dangerous strains of HPV.
Since vulvar cancer is more common among women who smoke, quitting the bad habit is an effective preventive measure.
Even if a woman leads an absolutely “correct” lifestyle, this does not guarantee that she will not get sick. Therefore, early diagnosis is important and you need to regularly visit a gynecologist.
Diagnosis of benign tumors of the vulva
Only a gynecologist can make an appropriate diagnosis and determine the type of tumor. Considering that they can develop asymptomatically, only regular examinations by a specialist can track the disease at an early stage.
Diagnosis begins with collecting anamnesis. The doctor finds out:
- patient complaints (discomfort, pain, discharge);
- time of their appearance;
- intensity of their manifestation;
- presence of past gynecological diseases;
- presence of pregnancies, abortions, childbirth and operations;
- picture of menstrual function (cycle stability, pain, profuseness).
Next comes a gynecological examination, which necessarily includes a bimanual examination. In addition to standard gynecological procedures, you may need:
- transvaginal ultrasound;
- vulvoscopy - examination of the external genitalia using a microscope (in some cases, non-contact);
- vaginal examination;
- colposcopy or vaginoscopy - examination of the vagina and the part of the cervix close to it.
These methods make it possible to verify whether the tumor has spread from the external genitalia to the internal organs, and if this has happened, then by how much.
If the doctor decides that the tumor is at risk of degenerating from benign to malignant, he will take a fragment of it and conduct a histological examination. In this case, the help of not an ordinary gynecologist, but a gynecologist-oncologist is required.
Prices for treatment of vulvar cancer at Euroonco
The cost of treatment for vulvar cancer depends on the stage of the tumor, the extent of surgery, and whether it needs to be supplemented with chemotherapy, radiation therapy, and other types of treatment. At Euroonko you can get care at the level of leading Western oncology centers, but at a lower price.
Appointment with an oncologist-gynecologist - 6,900 rubles. Photodynamic therapy - from 170 rubles (calculated depending on the patient’s weight).
Book a consultation 24 hours a day
+7+7+78
Symptoms of pathology
Symptoms of early stage vulvar cancer are nonspecific. Patients feel itching and the skin is moderately irritated. Symptoms are almost unnoticeable during the day and intensify at night. As the tumor focus grows and lymph outflow is impaired, ulcerations and weeping appear on the mucous membrane and skin. The vulva swells, a violation of the integrity of its cover leads to the formation of bloody discharge. Purulent contents form when a secondary infection occurs.
Gradually, the pain syndrome becomes more intense. The most severe pain occurs when the clitoris is affected and adjacent tissues are invaded. The disintegration of the primary focus provokes massive bleeding and a specific smell appears. The patient suffers from urinary retention and intestinal obstruction. Swelling of the pubis and lower extremities appears.
Lymphatic vessels are the main routes of metastasis of vulvar cancer. The pathological process affects the inguinal lymph nodes, then moves to the iliac and hypogastric. Patients complain of fatigue, weakness, and decreased performance.
Swelling of the penis and testicles.
Swelling of the genital organs can be caused by both completely harmless factors (passionate sex, tight underwear, allergies, poor hygiene) and serious reasons. Therefore, if the swelling does not subside within a day or additional symptoms appear (itching, burning, redness, discharge, rash, inability to open the foreskin), you should consult a specialist.
Why does the penis and/or testicles swell?
Various reasons can cause swelling of the penis and testicles:
Balanitis, posthitis, balanoposthitis.
Balanitis (inflammatory disease of the head of the penis) and posthitis (inflammatory process of the foreskin) are usually inseparable, which is why they are combined under the common term “balanoposthitis.” In a man, erosions form on the head of the penis and in the area of the foreskin, pain, swelling, and hardening of the inguinal lymph nodes are possible.
Cavernite.
Pathological processes in the cavernous bodies cause swelling of the shaft of the penis.
Phimosis.
Due to the narrowing of the foreskin, the head of the penis is not fully released, which leads to inflammation and swelling.
Paraphimosis.
Pinching the head of the penis by the foreskin causes redness and swelling of the organ, and pain when urinating. In the absence of timely medical care, tissue necrosis is possible.
Thrombophlebitis.
As a result of inflammation of the dorsal vein, the penis swells and the temperature rises sharply. Physical activity and movement cause pain.
Allergy.
Itching and swelling of the penis can be caused by synthetic underwear, poor-quality lubricants, condoms, and long-term use of antibiotics.
Microtraumas.
The slightest bruise can provoke swelling of the penis and the appearance of a hematoma, which is explained by the increased sensitivity of the organ. Sometimes the cause of microtrauma can be a strong impact on the penis during sexual intercourse or masturbation, or wearing too tight underwear.
Infections.
Sexually transmitted diseases (trichomoniasis, chlamydia, gonorrhea, syphilis) often cause swelling of the genital organs. With syphilis, a growing compaction also becomes noticeable, and the general condition worsens. Swelling of the penis is also possible with systemic infections (tuberculosis).
Tumor.
The cause of swelling can be a malignant neoplasm, but swelling of the entire trunk is extremely rare.
Diagnosis of bartholinitis
Acute bartholinitis and Bartholin gland cyst do not cause any difficulties in diagnosis.
In acute bartholinitis and pseudoabcess of the Bartholin gland, all the classic signs of inflammation are present: pain, tumor formation and local (local) increase in temperature.
A certain difficulty arises when making a decision to treat conservatively (medically) or operate.
In other words, it is necessary to answer the question: is the inflammatory process widespread, or has a PSEUDO-ABCESS already formed in the form of a cavity with purulent contents.
| The success of treatment and aesthetic comfort depend on accurate diagnosis! Accurate diagnosis and treatment of bartholinitis WITHOUT ANTIBIOTICS, opening of the Bartholin gland WITHOUT PAIN, on the same day of treatment, with the Surgitron device is one of the popular areas of practical activity of the Women's Health Clinic. |
Make an appointment with a gynecologist
| 3D photo of a left Bartholin gland cyst in a 28-year-old woman | |
| 3D photo of a cyst in the right large gland of the vaginal vestibule of a 16-year-old girl |
Pay attention to the excellent quality of the photographs, testifying to the expert class of our devices.