Lumps, nodules, tubercles and other lumps on a woman’s outer labia are almost always a pathological phenomenon that requires emergency medical attention. Even if the neoplasms seem benign to you, without causing acute discomfort and pain.
Most common reasons
- Such phenomena can be detected in childhood and be congenital. In this case, it is advisable for parents to check their blood for syphilis, since most often changes in the genital organs in infants indicate its presence.
- In addition, the tubercles may be a sign of abnormal development of the labia, congenital defects of the urethra and other features that do not have an infectious or viral etiology. However, this is more of a special case than a healthy phenomenon.
- We should not forget that neoplasms in the genital area can become a sign of tumor processes in the body.
- In addition, nodular fragments may indicate the development of HPV (human papillomavirus). This disease in a certain percentage of cases leads to cervical cancer.
Our doctors will help you accurately determine the etiology of your genital tubercles.
Such deviations are not a reason to be embarrassed and ignore medical help.
Leave your phone number. The clinic administrator will call you back.
Make an appointment
The doctor's consultation
1290 rub.
If the tubercles appear suddenly and can be easily felt under the skin or mucous membrane, immediately contact a specialist for advice and all necessary tests. Perhaps it is the early intervention of a specialist that will help you avoid terrible irreversible consequences.
Bartholinitis
Very often, bumps on the labia appear due to inflammation of the Bartholin glands. They are localized at the entrance to the vagina and are located in the subcutaneous fatty tissue of the labia majora. The Bartholin gland synthesizes a mucous secretion that forms in the vagina on the eve of sexual intercourse. Blockage of the excretory ducts of these glands leads to an inflammatory process in the organ, resulting in neoplasms in the form of small bumps. This disease often occurs in women who do not pay due attention to personal hygiene.
How do symptoms develop?
- The specificity of the disease is such that symptoms do not appear immediately;
- 1-2 weeks after the onset of the inflammatory process, a seal forms on the inside of the labia majora;
- The ball begins to hurt and cause discomfort, especially when wearing tight underwear;
- The large lips swell, there is a burning sensation and pain in the perineum;
- Suppuration and effusion of exudate are possible, but more often this does not happen.
Bartholinitis does not require specific treatment, however, in its complete absence, women experience frequent relapses of the inflammatory process. At the same time, a new disease begins - a Bartholin gland cyst. In this case, surgical treatment is used, since alternative therapeutic methods become powerless. If the lump begins to suppurate during bartholinitis, there is a sharp deterioration in general well-being, pain during sexual intercourse, and an increase in body temperature up to 40 degrees. It should be emphasized that bartholinitis during pregnancy can provoke spontaneous abortion.
If you have been diagnosed with bartholinitis, our experienced specialists will select a course of gentle antibiotic treatment for you or use surgical tactics to excise the cyst. Do not forget to maintain your health after treatment, maintain good personal hygiene and use contraceptives when changing partners. Know that bartholinitis can also develop due to parasitism of pathogenic microorganisms in your individual microflora. Often the disease is a consequence of trichomoniasis, gonorrhea and chlamydia.
Diseases of the Bartholin glands
Causes of inflammatory processes and risk factors for the development of other pathologies:
- Failure to comply with personal hygiene rules (especially during menstruation).
- Any local microtraumas (scratching, epilation of deep bikini, sexual intercourse with dry vulva).
- Wearing tight underwear.
- Too active sex life, ignoring barrier contraception.
- The presence of foci of persistent infection in the body (caries, pyelonephritis).
- Impaired functioning of the immune system, lack of vitamins.
- Surgical interventions on the genitourinary area (for example, abortion).
Pathologies of this place occur, first of all, when the exit of one or both ducts is blocked, which prevents the release of mucus to the outside with the development of inflammation - bartholinitis. These cases are often associated with sexually transmitted infections (STIs) or other bacterial pathogens such as E. coli and enterococci. Bacteria that normally inhabit our skin, such as staphylococci and streptococci, may also be a cause. Other risk factors include hypothermia, the presence of foci of chronic infection in the body (adnexitis, tonsillitis, caries, etc.).
The two most common complications arising from this problem are cyst and gland abscess.
Benign and malignant tumors of this location are very rare and account for approximately 1% of all vulvar tumors. But they still exist for this reason - after all, the gland consists of columnar epithelium, and the ducts are lined with multilayered squamous epithelium and transitional cell epithelium. Therefore, adenocarcinomas, squamous cell carcinoma and, less commonly, transitional cell carcinoma can arise from the Bartholin gland in women. Most primary adenocarcinomas of the vulva arise in these glands.
The average age at diagnosis is 55-57 years. 10-15% of patients had a history of inflammation of Bartholin's gland. Human papillomavirus (HPV in women) has been identified as a major contributor to the development of squamous cell carcinoma of this organ.
Tumor formations
Lumps in the groin area and labia can be a sign of a tumor process in the body. Fortunately, genital tumors are often benign.
- Fibroma is a neoplasm of benign etiology, which is localized in the connective tissue, less often in the fascia of the parametric tissue. As a rule, it is located on the labia majora. Treatment of the tumor is exclusively surgical. Our doctors effectively treat this disease, guaranteeing a further favorable prognosis.
- Fibromyoma is a tumor that does not entail tissue destruction and metastasis (also benign). It is formed from muscle fibers and appears as a lump on the labia majora. Surgical excision is mandatory.
- Lipoma is a more severe tumor that does not have a malignant etiology. It is formed from adipose tissue and is located near the vulva. It is a nodule or several overgrown small neoplasms. Located on a dense, stable leg. The size of the nodule is usually small, but tends to grow. Such a tumor is always accessible during a traditional examination without additional diagnostic procedures. You may also be able to detect a lipoma by feeling your genitals or washing your face. If the disease is not treated, various complications are possible: hemorrhage, infection, swelling and even tissue necrosis. Our surgeons excise the lipoma and prescribe further supportive therapy.
- Hidradenoma is a rare type of tumor in the genital area. It develops due to the active activity of the sweat glands and some other abnormalities. In the case of this disease, hardening in the form of nodules forms on the labia, sometimes they are localized over the entire area of the organ or are single. Hidradenoma must be treated in a timely manner, otherwise it may develop into a malignant tumor.
- Oncology. (Cancer or sarcoma of the vagina, cancer of the vulva). It appears in the form of nodes and dense tubercles in the genital area. If benign tumors practically do not cause additional symptoms, oncology is always accompanied by copious discharge of pus or mucus with a pungent odor, bleeding, and diffuse infiltrates. Unfortunately, in this case, no one can give an unambiguous favorable prognosis, even with timely treatment.
Causes of atheroma on the lips
Normal functioning of the body includes the periodic release of excess sebum to the surface of the skin through special ducts of the sebaceous glands. Atheroma occurs when these ducts become blocked. Various reasons can lead to this. The main reasons for the appearance of atheromas on the lips are:
- Violation of hormonal functions;
- Constant use of low-quality cosmetics and foundation;
- High oily skin;
- Problems with the functioning of the sebaceous glands;
- Injuries on the face (small wounds, cracks or split lips).
The problem with atheroma on the lip lies in its location. It is constantly open to environmental factors, is more susceptible to injury, and also interferes with normal communication and eating.
Having identified a tumor on the lip, you should immediately consult a doctor for a diagnosis, since an initially harmless and painless atheroma can later lead to consequences more serious than simple discomfort. It, unlike lipoma, is dangerous because it is prone to infection and inflammation.
Useful information about visiting a surgeon at the clinic:
- How to prepare for a surgeon's appointment
- What diseases does the surgeon treat?
- Calling a surgeon to your home
- Surgical care in the clinic
- Surgical care at home
- What symptoms should you contact a surgeon for?
- Treatment of surgical diseases
- Treatment of intestinal pathologies
- Treatment of skin surgical pathologies
- Treatment of bedsores and necrosis
- Treatment of parasitic diseases
- Treatment of inflammatory processes of soft tissues
- Treatment of diseases of the musculoskeletal system
- Diagnosis of surgical diseases
Therapy in our clinic
If you notice lumps on your genitals, we recommend that you do not hesitate to contact our qualified specialists. You will be examined by our gynecologists, after which, if necessary, they will be referred to a surgeon. We will carry out the appropriate treatment, choosing the best option for you. We always strive to choose gentle techniques, but if this is not possible, our surgeon will eliminate your tumor quickly, painlessly, with a guarantee of no complications.
Many years of practice and extensive experience of our specialists allow us to vouch for the health of each patient. We recommend that you consult a doctor in a timely manner to avoid serious complications and relapses of the disease.
Features of atheroma
Atheroma is a small capsule filled with fat. Atheromas are often confused with lipomas (both have the same name among the people - wen), but there are significant differences between them. Lipomas arise due to deformation of adipose tissue, while the cause of atheromas is clogging of the sebaceous glands.
It is quite difficult to distinguish a lipoma from an atheroma by appearance alone. For a correct diagnosis, you need the help of a specialist who will examine, prescribe the necessary tests, and based on this determine the nature of the tumor.
The distinctive features of atheroma include the immobility of tissue under the neoplasm, as well as a black dot at its apex. A black dot is evidence of a clogged duct of the sebaceous gland, from which fat cannot be removed and therefore accumulates under the skin. As a result, a kind of capsule is formed, the dimensions of which can vary from 5 mm to 5 cm.
What symptoms do you see a surgeon for:
- Presence of hernial protrusion
- Daggering pains in the abdomen
- Bloating
- Pain in the right hypochondrium
- Bitterness in the mouth
- Nausea
- Presence of neoplasms on the skin
- Swelling and redness of the skin
- Bone fractures and bruises
- Wounds of any location
- Vomit
- Enlarged and painful lymph nodes
VASCULAR FORMATIONS
Angiokeratoma
Angiokeratoma of Fordyce manifests as multiple, well-defined, bluish-black papules on the skin of the scrotum [Figure 7a]. They are often clinically mistaken for genital nevus, blue nevus and melanoma. Various sources indicate that 20% of angiokeratomas were misdiagnosed as melanoma [32]. Dermoscopy clearly shows pronounced reddish-dark blue lacunae with a blue-white veil [Figure 7B] [33].
Lymphangiectasia of the vulva
Acquired lymphedema and lymphangiectasia of the vulva usually occur due to damage to the lymph nodes that occur after trauma, infection, malignancy, surgery, radiation, etc. Clinically, they present as flesh-colored papules or transparent vesicles with a diffuse erythematous background. Piercing the lesion may release clear fluid. Dermoscopy reveals clearly defined, round-oval reddish lacunae with whitish septa and numerous small pinpoint lacunae. This is similar to the manifestations of lymphangioma. Dermatoscopy is relevant when lesions are sometimes confused with warts or molluscum contagiosum [34].
BENIGN LOCATIONS
Seborrheic keratosis
Pigmented seborrheic keratosis, like its cutaneous counterpart, shows features such as polypoid structures, marrow-like structures, and finger-like structures on dermoscopy. Comedo-like structures, which are keratin-filled invaginations, are not observed in genital seborrheic keratosis due to constant friction. Milium-like cysts are usually visible because they are located intraepidermally [11,19].
Verruciform xanthoma
These are rare tumors composed of lipid macrophages that present clinically as yellowish plaques and nodules with a papillomatous surface in the anogenital areas. Dermoscopy reveals numerous yellowish papules with centrally located spiny vessels [20,21].
PRE-CANCEROR FORMATIONS
Extramammary Paget's disease
Extramammary Paget's disease is clinically characterized by erythematous plaques with oozing, ulcerated, and scaly nodules and focal hyperpigmentation. Areas of hypopigmentation can also be seen (Fig. 6a). Dermoscopy of extramammary Paget's disease reveals milky red areas, vascular structures, superficial scales, ulcers, pigment network, shiny white lines and white structureless areas [Fig. 6b]. Common vascular structures are stippled vessels and glomerular vessels [22]. Paget's disease is often mistaken for melanoma due to features such as irregular pigmented globules, white negative pigment network, and structureless blue-gray areas [23].
Erythroplasia Keira
It is the genital counterpart of Bowen's disease and has similar dermoscopic features. Glomeruloid vessels are characteristic, located in clusters or diffusely, which can be used to differentiate Queyre's erythroplasia from other causes of chronic balanitis. In addition, linear vessels and brown dots can be seen [24]. Dermoscopic features in pigmented Bowen's disease include pigmented streaks combined with other features such as comedo-like structures [25].
Vulvar intraepithelial neoplasia
This is a common cause of genital itching. About 15% of vulvar intraepithelial neoplasias are pigmented. Typical findings are milky white or pink areas associated with punctate or glomerular vessels and papillomatous structures. In the pigmented version, brownish dots with clearly defined boundaries and brain-like structures are visible [26].
INFLAMMATORY DISEASES
Balanitis Zuna
In this condition, well-defined reddish plaques are visible on the skin of the glans or the inner side of the foreskin [Figure 8a]. Dermoscopy reveals uniform reddish-orange areas with curved vessels [Figure 8b] [24]. The orange areas correspond to hemosiderin deposition, and the curved vessels represent vascular proliferation. Other types of vascular structures include crescentic vessels and convoluted, cupped, linear and stippled vessels [35].
Candidal balanitis
Candida balanitis is characterized by curdled-like structures, which are colonies of fungi, as well as linear vessels [24].
Psoriatic balanitis
Clinically, multiple erythematous papules and plaques are detected. Dermoscopy reveals uniformly distributed, dilated and dotted vessels on an erythematous background [36].
Lichen planus
Thick, linear and irregular hairpin-shaped vessels are distributed diffusely according to the localization of lichen planus plaques. The Wickham grid is clearly visible against an intense red background [5].
Lichen sclerosus
White, ivory-colored atrophic plaques are visible on the skin of the glans and labia minora, disrupting the normal architecture of the skin of the anogenital area [Figure 9a]. Dermoscopy reveals white structures that appear pinkish, consistent with sclerosis on histopathology [36]. The gray-blue dots are arranged in a pattern of scattered pepper, which corresponds to melanophages of the skin. Characteristic features are a marked decrease in the number of vessels and the presence of polymorphic vascular patterns [Figure 9b] [5]. Purple-red globules and spots are visible especially in women, consistent with blood stains due to excessive scratching.
CONCLUSIONS
Dermatoscopy has become important in the diagnosis of non-pigmented dermatoses and for differentiating benign lesions from equivocal and malignant lesions [1, 28]. Many dermatologists in modern practice have included dermatoscopy in their routine work. Although this does not eliminate the need for biopsy, the technique avoids unnecessary biopsies of benign lesions. It also helps us carefully select the biopsy site for suspicious or atypical pigmented lesions.
MALIGNANT EDUCATIONS
Melanoma
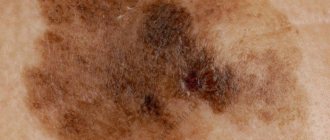
Vulvar melanomas account for 1-3% of all melanomas observed in women. They are often found in older women and present as flat or raised pigmented lesions that are often larger than 7 mm in size. Non-pigmented variants have also been described. Multiple colors and a multicomponent structure pattern characterize the dermoscopic picture of mucosal melanoma [11, 27]. The presence of blue, gray and white colors with or without structureless areas had 100% sensitivity for diagnosing melanoma [28]. Reticular depigmentation and a network of fine whitish lines are valuable in the diagnosis of early vulvar melanoma [10]. In non-pigmented melanoma, dermoscopy reveals whitish, skin-colored papules with polymorphic vessels [29]. Asymmetry, multicomponent patterns, blue-white veil, and the presence of vessels should raise suspicion of malignancy and be confirmed by histopathology [30].
Basal cell carcinoma
Dermoscopy of genital BCC is similar to cutaneous BCC, consisting of bluish-gray ovoid globules, whitish homogeneous areas, and tree-like vessels. Non-pigmented lesions are difficult to diagnose because... they can mimic inflammatory diseases. In this case, clearly visible tree-like vessels help make the diagnosis [31].