Dermatovenerologist
Khasanova
Alina Rashidovna
9 years experience
Make an appointment
Ringworm (microsporia) is a disease manifested as a fungal infection of the skin, nail plates and hair follicles. The pathogen is a mold fungus of the genus Microsporum. Its colonies form in keratinized substrates. Microsporia remains a relatively common disease - dermatologists identify 60-75 cases for every hundred thousand Moscow residents. The pathology has a pronounced seasonality. The peak incidence occurs at the end of summer and beginning of autumn - the period of breeding of offspring in cats and other animals.
Routes of infection
The causative agent of microsporia enters the body when a healthy person comes into contact with a carrier of the disease. An alternative way is to interact with objects covered with fungal spores. Ringworm is most often detected in children aged 5-10 years; in boys, microsporia is diagnosed five times more often than in girls. The pathology almost does not affect adults due to the presence of organic acids in their hair structure, which suppress the growth of fungal mycelium.
The reasons for the development of ringworm are microtraumas of the skin and its dryness. Spores get into cracks, scratches or open calluses. Healthy skin becomes an insurmountable barrier to fungus. The pathogen does not survive contact with personal hygiene products - thorough hand washing after contact with spore carriers eliminates the possibility of infection.
The risk group includes people who regularly come into contact with the ground and wild animals. The active growth of the fungus is facilitated by disturbances in the functioning of the sebaceous glands due to changes in the chemical composition of their secretions. Microsporum spores can remain viable for three months when left in open ground.
Prevention of ringworm
- Isolation of the patient to prevent the spread of the disease.
Considering the fact that ringworm is very contagious, patients are subject to isolation until complete recovery and are allowed into the children's group only after three negative tests for fungi.
- Maintaining hygiene.
This implies the separate use of personal hygiene items: combs, elastic bands and hair clips, washcloths, towels, as well as hats and bed and underwear (T-shirts, pajamas, socks, slippers). Thorough hand washing is necessary after the child interacts with animals, especially those living on the street;
- Carrying out disinfection in places of detection, treatment of the patient (at home, in children's institutions, as well as in hospitals).
- Control over disinfection in public places (baths and saunas, swimming pools, sports complexes, hotels and hostels).
- A sick child is prohibited from visiting child care institutions (kindergarten, school, camp, club), as well as swimming pools, baths and saunas, until complete recovery.
- All persons in contact with the patient are examined daily by a medical professional for the first three days. Further examination is carried out 1 or 2 times a week, for 21 days. At the same time, the skin and hair on the head are examined.
- After the patient recovers, all objects with which he came into contact are disinfected.
Symptoms of pathology
Symptoms of ringworm appear 4-6 weeks after the patient becomes infected. A red spot appears on a smooth area of skin of a child or adult. It rises above the surface and has smooth boundaries. Over time, the size of the lesion increases. The surface becomes covered with nodules, blisters and scabs. The spots develop into rings that can intersect or merge with each other. The diameter of skin formations ranges from 5 to 30 millimeters.
Signs of ringworm include an acute inflammatory reaction. It often develops in children and girls. The lesions begin to peel off intensively. Patients suffering from dermatitis do not immediately identify symptoms of microsporia. Areas of active fungal growth may appear as inflammatory skin lesions.
A common manifestation of ringworm in a child is damage to the scalp. This symptom affects patients aged 5-12 years. Older children experience changes in the chemical composition of sebum. Its elements become dangerous for the microsporia pathogen.
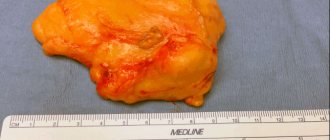
The suppurative type of ringworm is characterized by the appearance of soft nodules on the patient’s skin. The nodes are dotted with numerous abscesses. When they are compressed, purulent contents are released.
Are you experiencing symptoms of ringworm?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Treatment of lichen in children and prevention of relapses
Treatment of lichen in children should be carried out exclusively under the supervision of a dermatologist. Experienced specialists at your Clinic today treat this disease with a 10% discount if you submit an application online.
The choice of treatment regimen depends on the type of lichen and the severity of the manifestations. The approach to treatment is complex; the choice of ointment is based on test data and individual tolerance to the drug. The doctor selects medications in such a way as to eliminate all signs of the disease as quickly as possible, while making sure that the lichen does not return again. Therapy methods:
- Antifungal (mycotic) drugs for external use. These are various ointments, lotions, solutions, aerosols, sprays, creams for application to affected areas. Depending on whether the lichen is found on the skin or hair, the form of the medicine is prescribed so that it is convenient to use. The mechanism of action is antifungal, inhibits the growth of fungi. Ointments include a certain percentage of the active substance, for example, miconazole, terbinafine, clotrimazole, ketoconazole, etc. There are dozens of types of drugs, and the doctor will help you choose the optimal substance, form and dose.
- Oral medications allow you to quickly get rid of the symptoms of the disease, improve sleep, and eliminate peeling and itching.
- Anti-inflammatory and antibacterial agents - in case of inflammation or infection in the scratched wound.
- Vitamins of group B, C.
Today it’s easy to get rid of lichen; the main thing is to make the correct diagnosis and follow all the specialist’s recommendations. Your doctor will tell you how to treat lichen in a child most effectively. He is the one who will select a comprehensive therapy that is suitable for your child. The peculiarity of treating children is to select the correct dosage - it is difficult to do this on your own, especially if the disease appears in an infant. The spots can be very itchy, so children may develop sore spots on their scalps. At night it is difficult to fight this, but during the day you need to try to distract the child with drawing, modeling and other interesting activities, use ointments and sprays that relieve itching. Lotions of solutions of iodine, silver nitrate, and ichthyol will help reduce the manifestations of inflammation, especially in the suppurative form. Treatment of lichen in children occurs mainly at home, but if there is a high temperature and the child’s condition is quite serious, in the hospital. Therapy takes 1-2 weeks, with an infiltrative-suppurative form – slightly longer.
Diagnostic measures
Diagnosis and treatment of ringworm are carried out by a dermatologist. The doctor examines the patient and identifies typical manifestations of microsporia. Examination of skin scrapings under a microscope reveals fungal mycelium and changes in the structure of hair and skin. Differential diagnosis makes it possible to exclude trichophytosis from the patient’s history, which has similar manifestations upon microscopy of the patient’s biomaterials.
Microflora culture appears to be a more informative diagnostic technique. Laboratory staff determine the type and genus of fungi. Based on the laboratory report, the dermatologist selects drugs that will cure the patient.
Luminescent examination makes it possible to identify pathological lesions on the skin of the patient and those living with him. This diagnostic method is based on the green glow of the fungal mycelium under the influence of a gas-discharge light source.
Diagnostics
It is not difficult to make a primary diagnosis if you know what ringworm looks like. To clarify the diagnosis use:
- analysis of clinical data;
- results of luminescent analysis;
- microscopic studies;
- sowing material.
In some cases, the source of infection is difficult to determine, since the incubation period ranges from 2 to 45 days. Symptoms may appear on the head, neck, arms, legs, including the palms, soles of the feet, groin areas and folds. Fungal infection causes itching, discomfort in the area of inflammation, and creates psychological discomfort.
Treatment
The combination of drugs prescribed to the patient depends on the severity of damage to the skin, nail plates and hair follicles. Antifungal therapy may be local or general. In the first case, a child or adult needs to use creams and ointments that suppress the activity of the microsporia pathogen. Drugs in this group are not recommended for use by girls during pregnancy and lactation. Topical sprays are effective in treating large areas of ringworm. Modern formulations do not leave stains on the skin and are not absorbed into the fabric of clothing.
A severe inflammatory reaction is treated with a combination of antifungal and hormonal drugs. Patients will have to apply ointment applications to the affected areas. After this, the skin is treated with iodine solutions. The oral tablet intake schedule is formed by a dermatologist based on the clinical picture of the pathology.
The addition of a secondary infection to microsporia involves the use of drugs based on betamethasone, gentamicin or clotrimazole.
Reasons for development
The main causes of ringworm are contact with the pathogen:
- A child aged 4–11 years whose sweat reaction is predominantly alkaline.
- A child or adult with reduced immunity, the presence of scratches, scabs, microtraumas that can become infected.
Most often the carrier is an animal, less often a person. Infection also occurs through objects or personal belongings on which infected hairs, hairs or skin scales remain. Infection is possible through undisinfected hairdressing tools, through soil on which the causative agent of the disease can persist for up to 3 months, during processing of hay. According to statistics, up to 70–80% of cases of the disease occur as a result of contact with stray young cats and kittens.
Preventive measures
Prevention of ringworm is based on regular medical examinations of children attending preschool educational institutions. Parents should talk to their children about the inadmissibility of contact with stray animals. An important preventive measure is compliance with personal hygiene rules by patients of all age groups.
When purchasing pets, you must visit a veterinarian. The doctor will examine the cat or dog and give recommendations on how to eliminate any health problems with the pet. Following your veterinarian's advice will help prevent microscopic outbreaks within your family.
Symptoms
Ringworm on the face and body appears in the form of pink or red circles raised 1-3 mm above the surface of the skin. The lesions are characterized by clear boundaries, while pale areas of skin with red dots are visible inside. These spots quickly increase in size. Their number is growing over time.
The skin inside the lesions becomes covered with a white crust, which peels and itches. Ringworm on the scalp is characterized by split hair and hair loss. As the number of lesions increases, they begin to connect and overlap each other. Ringworm on the body occurs with increased symptoms when the pathogen gets inside existing lesions, and new fungal rings form in them.
Sources
- Anderson KR: Treatment with dapsone in pityriasis versicolor vesicularis rosea, 1971;
- Andrews GK: Skin Diseases 1954;
- AranjoT. et al.: Human Herpesviruses 6 and 7, 2002;
- Bernhardt R.: Skin diseases: 1922;
- Bjornberg A, Hellgren L: Pityriasis rosea. Statistical, clinical and laboratory research, 1962;
- Buckley K: Rash resembling pityriasis rosea in a patient receiving omeprazole, 1996;
- Gutowski W.: Attempt to treat Gibert's pink dandruff with bismuth and penicillin, 1950;
- Kempf W. et al.: Pityriasis rosea is not associated with human herpes virus, 1999;
- Parson JM et al: Update on pityriasis rosea, 1986;
- Sharma PK, Yadav TP: Erythromycin for pityriasis rosea, 2000;
- Wass I.: Treatment of pityriasis rosea with nonspecific substances, 1948.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
How do you know if pityriasis rosea is going away?
After a course of therapy, the spots disappear without scarring. In place of the plaques, clean skin remains, possibly lighter. Over time, the color evens out. In patients with atypical lichen, ulcers may form.
Complications during self-medication:
- infection of affected areas with bacteria;
- suppuration, ulcers;
- hyperpigmentation.
Hyperpigmentation
To prevent this development of the disease, at the first symptoms of pityriasis rosea, it is recommended to make an appointment with a dermatologist.
Measures to prevent the disease
Since there can be many causes of lichen infection, it is impossible to completely exclude the possibility of the disease. However, compliance with preventive measures will reduce the risks. Prevention of lichen includes:
- timely treatment of acute respiratory diseases;
- compliance with hygiene procedures;
- taking a vitamin complex;
- increasing the level of immunity;
- use of shampoos with antifungal gels;
- hardening of the body;
- providing quality oral care, treatment of caries, gums and throat diseases;
- proper nutrition;
- avoiding contact with people infected with the fungus;
- vaccination of pets and periodic examinations at a veterinary clinic;
- giving up bad habits (smoking, alcoholism);
- preventing hypothermia of the body.
When diagnosing a chronic form of lichen, it is recommended to periodically visit a dermatologist’s office in order to identify possible foci of the disease.
Diagnostic methods for determining the type of lichen
The main ways to determine fungus are the following:
- visual examination of the patient, where the color, shape and location of the rash are determined;
- collection of complaints and analysis of symptoms.
Each species is determined by different methods. First of all, a sick patient should seek advice from a dermatovenerologist.
Shingles is difficult to determine by simple visual inspection, so additional diagnostic procedures will be required:
- searching for the presence of antibodies to viral pathogens;
- bubble content analysis;
- using the hybridization method to determine the genome of the virus.
If pityriasis is suspected, the doctor will send the patient for blood and urine tests, and will also conduct a microscopic examination of the scales to exclude the diagnosis of syphilis. Pityriasis can be diagnosed better than other types of disease through visual examination.
Lichen versicolor can be identified by the results obtained from the following procedures:
- Examination of the lesion site with a Wood's ultraviolet lamp. The doctor “examines” the fungal spores, which turn yellow or brown.
- At the appointment, the doctor drops a few drops of iodine onto the affected area of the skin and immediately wipes it with a cotton swab moistened with alcohol. If it is a multi-colored fungus, the skin will turn brown.
- Taking a sample by scraping the skin for microscopic examination in a laboratory.
To diagnose lichen planus, the patient will be referred for general blood and urine tests, as well as a skin sample for histological examination.
Trichophytosis can be determined using the following methods:
- “X-raying” of the skin using a Wood's ultraviolet lamp. This form of fungus will turn green.
- Submission of biochemical blood and urine tests.
- Determining the degree of sensitivity of the pathogen to selected antibiotics by inoculating the sample taken on nutrient media.
- Taking a sample by scraping the skin for microscopic examination in a laboratory.
What is pityriasis rosea and why is it called pink dandruff?
The content of the article
Pink dandruff (Pityriasis rosea - PR) is an acute inflammatory disease of unknown etiology, characterized by the appearance of skin rashes mainly on the torso and limbs. It is an erythematous, scaly disease. The disease occurs seasonally. The etiology is most likely viral. The most likely factor is herpes virus type 7 (HHV7).
Most cases (75%) involve people aged 10 to 35 years, although there have been reports of cases diagnosed in a 3-month-old infant and in an 83-year-old man. The disease occurs throughout the world without any particular racial predilection.
Pityriasis rosea is a disease for which patients visit a dermatologist with a frequency of up to 2% of all visits per year. Occurs mainly in spring and autumn; in summer the level of symptoms decreases significantly.
The disease affects more women than men in a 2:1 ratio. The duration of the disease is 6 to 8 weeks, but is highly variable.
Correct treatment of pink dandruff in Gibert's disease
Treatment of pityriasis rosea is primarily based on the diagnostic results and recommendations of the dermatologist based on his knowledge and experience. Independent attempts to cure pathology usually lead to the appearance of accompanying symptoms, sometimes very dangerous.
Considering the symptoms, the dermatologist prescribes:
- ointments with corticosteroids acting in several directions - relieve skin tightness and accelerate the healing of the rash;
- antiallergic - antihistamines - relieve itching;
- immunomodulators – stimulate natural immunity;
- antiseptic solutions – prevent secondary infection;
- dandruff softening ointments.
During treatment, the dermatologist recommends:
- Avoid hot water procedures and swimming. Showering with a soft sponge is allowed;
- Wear loose, natural underwear. Synthetics do not allow the skin to breathe, exacerbating symptoms;
- Eliminate allergens: eggs, chocolate, red fruits.
- Reduce fried, flour, smoked foods;
- Do not use cosmetics.
Many names - one face. Symptoms of pityriasis rosea
The first description of the disease as "ringed roseola" dates back to 1798. Uch. Robert William defined the disease as irregularly shaped spots consisting of small thin scales that never coalesce into scabs and are not accompanied by redness or signs of inflammation.
Other names for this disease: erythema annulatum, tonsurans maculosus, Herba, roseola squamosa (Nicolas, Chapard), pink lichen (Wilson), pityriasis versicolor (Horand), pseudoexanthemata nitoexanthemata, roseola furfuracea herpetiformis (Behrend) - mainly determined the morphological features and variability individual spots.
Pityriasis rosea
Only in 1860, the French physician Camille Melchior Gibert gave the name, which lasted almost 150 years. He wrote: “There is only one thing that can be described under the name of pityriasis rosea, and the characteristic features of this pathology are: small, branched spots, very faintly colored, no larger than a fingernail, numerous and tightly fitting ... the disease usually lasts up to 6 weeks or 2 months... in young people... ". Pityriasis means "bran" or "fine husk" and rosea translates to "pink".
The symptoms of pink dandruff are indeed quite characteristic. First, a heraldic lesion (the so-called mother plate) appears on the skin, most often on the torso. Usually it is several centimeters of red or dark pink erythema, covered with scales inside.
After a few days (and sometimes weeks), much smaller skin lesions of similar morphology are seeded. The rash occurs symmetrically, mainly on the torso and neck. There are no changes in the mucous membrane. Usually the skin lesions do not cause itching.
Possible variations of the rash:
- urticarial form of RL – blisters appear instead of plaques;
- vesicular form of RP - rashes in the form of small bubbles with clear or cloudy liquids;
- papular form of RL – protruding, cavity-free formations.
What consequences can lichen cause?
The most common and harmless type of lichen is pink. The course of the disease passes without complications.
Shingles can cause the following complications:
- inflammatory process in the membrane of the spinal cord and brain;
- partial or complete loss of vision;
- dysfunction of the musculoskeletal system;
- viruses that infect the respiratory organs and liver;
- postherpetic neuralgia.
Ringworm and versicolor often provoke the appearance of a secondary infection, which complicates the treatment process. In most cases, antibiotics are necessary. In addition, trichophytosis often leaves bald patches at the site of the fungal infection, which can remain forever.
A flat red fungus contributes to the manifestation of bacterial infections and the development of an inflammatory process in the patient’s oral cavity.
More often than others, the following categories of patients suffer from various types of lichen:
- pregnant and lactating women;
- people who do not care about their health and do not observe personal hygiene rules;
- children;
- pet owners;
- people with a low level of protective properties of the body.