Author
: Grachev Ilya Illarionovich
Editor
: Efremov Mikhail Mikhailovich
Date of publication: 09/25/2018 Date of update: 06/08/2020
Very often, the manifestations of psoriasis on the skin of the hands are local in nature, without spreading to the surrounding tissues. With this course, many patients do not pay attention to the rash and do not rush to consult a doctor. But in vain, because in the presence of provoking factors, a “fire” can break out instantly in the form of severe complications, the treatment of which is far from as simple as single psoriatic plaques. Doctors at the Moscow Paramita clinic are well aware of how and how to treat psoriasis on the hands. From this article you can learn how this disease is treated at the initial stage and in severe cases.
Why does psoriasis start on the hands?
Psoriasis on the hands in the form of single regular plaques is only a seemingly local pathological process. In fact, even 1-2 elements of the rash indicate the presence of a chronic inflammatory skin disease. Medicine has not yet been able to unravel all the mysteries of this disease. The exact causes of psoriasis have not been identified. It is only known that the pathological process is based on burdened heredity and immune disorders.
Currently, the genes responsible for the hereditary transmission of predisposition to psoriasis, including on the hands, are being identified and studied. Under the influence of genes, a change in metabolism occurs and a decrease in the content of enzymes that destroy substances involved in inflammatory reactions.
Immunity is also impaired, which leads to a multiple acceleration of cell division in the surface layers of the skin. The cells do not have time to mature when new underlying cells push them to the surface. This is another cause of psoriasis on the hands.
Psoriasis of any localization can spread throughout the body, so do not delay treatment.
See how easily the disease can be cured in 10-12 sessions.
Such changes lead to the appearance of characteristic symptoms of the disease. What does psoriasis look like on the hands? Initially, a scaly spot appears on the hands, sometimes on other parts of the body, which quickly turns into a papule with a raised inflammatory base. The papules grow and merge, forming huge plaques.
But not all genetically predisposed people develop the disease. The reason is the lack of exposure (or minor exposure) to provoking factors. If you avoid these factors, you may never get sick, even if both parents have psoriasis.
Diagnostics
Diagnosis of trophic ulcers on the hands consists of carefully collecting data on the development of the underlying disease. Upon examination, the doctor determines the nature of the ulcerative defect, linking it with the cause of its development. After this, laboratory and instrumental research methods are carried out. Laboratory methods include a complete blood count. It is used to determine the presence of blood diseases (anemia), the presence of inflammation (the level of leukocytes and erythrocyte sedimentation rate increases), the presence of an oncological focus (young and mature forms of blood cells). In addition to a general blood test, microbiological cultures are performed on various media. This is necessary to determine the infectious pathogen and prescribe appropriate antimicrobial drugs. Also, in the presence of immunological pathologies, an enzyme-linked immunosorbent assay is performed. It is used to determine the presence of foreign particles. Instrumental methods include: ultrasound diagnostics and computed tomography. With their help, blood flow in the vessels, the presence of pathological neoplasms and areas of ischemia are determined.
Factors that provoke the onset of psoriasis on the hands
Factors that contribute to the development of hand psoriasis are divided into general and local. Common factors include:
- sedentary lifestyle, overweight, obesity;
- hormonal imbalances; the hormonal system is one and a failure in one link will certainly lead to numerous disorders in the body, including metabolic and immune disorders;
- improper irregular nutrition, consumption of large amounts of high-calorie food, meat, sweets;
- bad habits – smoking, alcohol abuse;
- prolonged stress, high mental and physical stress;
- What matters are long-term chronic diseases and foci of infection that contribute to the development of intoxication, under the influence of which metabolism is disrupted.
Red spots on the skin after stress
Diagnosis of skin diseases
Very often, psoriasis on the hands is provoked by the following local factors:
- constant mechanical injury to the skin of the hands - abrasions, scratches, wounds;
- frequent exposure of the skin to various chemicals: household chemicals, industrial hazards, etc.;
- constant exposure to the cold - this leads to spasm of small blood vessels and disruption of skin nutrition; therefore, disruption of metabolic processes is only a matter of time;
- any skin infections - bacterial, fungal, viral.
Venous trophic ulcers. Basic principles of treatment.
Definition. A trophic ulcer of venous etiology is a defect of the skin and underlying tissues of the leg, resulting from a chronic disorder of venous outflow and not healing within six weeks.
Epidemiology
Venous ulcers are found in 1-3% of the adult population of Russia. The total number of patients with a history or currently suffering from venous ulcers of the lower extremities of venous etiology reaches 6% of the population. These data need to be clarified through targeted epidemiological studies.
Etiology and pathogenesis
The main nosological causes of the development of venous trophic ulcers are varicose and post-thrombotic disease, less often - congenital arteriovenous malformations.
Among the pathogenetic mechanisms, dynamic venous hypertension, venous edema and microcirculatory disorders with the development of microangiopathy, as well as molecular cellular mechanisms (macrophage reactions, activation of metalloproteinases, etc.), play a key role. Valvular insufficiency of perforating veins is an important, but not the only factor leading to the development of trophic skin disorders. This is evidenced by venous ulcers that develop in the absence of low venovenous discharge.
Classification
Closed trophic ulcers are classified as C5, open ulcers are classified as C6 clinical classes according to the CEAP classification.
Additionally, classifications describing the depth of the ulcer and its area can be used.
According to depth they are distinguished:
- I degree – superficial ulcer (erosion) within the dermis;
- II degree – ulcer reaching the subcutaneous tissue;
- III degree - an ulcer that penetrates into the fascia or subfascial structures (muscles, tendons, ligaments, bones), into the cavity of the articular capsule or joint.
By area they are distinguished:
- small, up to 5 cm2 in area;
- medium – from 5 to 20 cm2;
- extensive (giant) - over 50 cm2.
Features of clinical diagnosis
- Clinical examination with a thorough assessment of complaints and medical history.
- Identification of comorbid diseases affecting the course of trophic ulcers (diabetes mellitus, metabolic disorders, obesity, atherosclerosis, etc.).
- Assessment of vascular status with mandatory determination of pulsation in the arteries of the foot.
- Assessment of local status : in the vast majority of cases, venous ulcers are located on the inner surface of the lower third of the leg, less often they involve other surfaces of the leg or are circular in nature. A venous ulcer is a chronic wound, which is characterized by a combination of signs of all three phases of the wound process. However, from the point of view of choosing tactics for local treatment of a trophic ulcer, it is necessary to assess what phenomena prevail at the moment. The first phase of the wound process (inflammation) is characterized by the presence of necrosis and purulent discharge. Against this background, individual areas of the ulcer may be covered with fibrin, as well as flaccid and pale granulations. The edges of the ulcer and the surrounding tissue are compacted. The second phase of the wound process is characterized by the presence of bright granulation tissue. Active epithelization and scar formation are characteristic of phase III.
- Determination of the state of the peri-ulceral zone , which is characterized by the presence of hyperpigmentation, induration, lipodermosclerosis, and less commonly the phenomena of eczema and dermatitis.
Instrumental diagnostics
- Doppler ultrasound with ankle-brachial index measurement. A decrease in this indicator below 0.8 or an increase above 1.5 indicates the presence of serious concomitant arterial pathology.
- Ultrasound angioscanning when planning surgical intervention.
- X-ray contrast angiography or CT for suspected arteriovenous malformation.
Treatment of venous trophic ulcers
Treatment tactics
Treatment of trophic ulcers of venous etiology can be divided into two stages. The first stage involves closing the trophic ulcer using conservative measures. The second includes measures aimed at preventing relapse. This algorithm is successfully applied in 2/3 of patients. The indication for surgery for an active trophic ulcer is the ineffectiveness of adequate conservative treatment. In turn, the clear clinical effect of rational conservative treatment for 6 weeks allows us to recommend its continuation until the ulcer is completely closed.
Stage 1: closure of the trophic ulcer
Lifestyle correction.
- Diet. Limiting foods that contribute to fluid retention in the body (pickles, spicy seasonings, etc.). Preference should be given to vegetables and fruits high in vitamin C and bioflavonoids. It is advisable to expand the diet to include fish and poultry to ensure that the body receives easily digestible proteins. Attention must be paid to the prevention of constipation, which can increase venous hypervolemia of the lower extremities.
- Mode. Patients with venous trophic ulcers should not stand or sit for long periods of time. If the patient’s professional activity does not allow one to exclude prolonged static loads or exposure to high or low temperatures, it is necessary to be released from work until the trophic ulcer is completely closed or examined by the VTEK. During the night, the patient is recommended to keep his legs in an elevated position (15–20 cm above the level of the body).
Pharmacotherapy.
Antibacterial drugs . Indications for antibacterial therapy are signs of acute infectious inflammation of the soft tissues surrounding the trophic ulcer, or a high degree of bacterial contamination of 107 or more microbial bodies per gram of tissue. Ideally, culture is required to identify the microbial flora and determine its sensitivity to a specific antibiotic. It is also possible to prescribe drugs empirically, taking into account the most likely strains of microorganisms growing in venous trophic ulcers. Protected penicillins (ampiox, amoxiclav) can be first-line drugs. The use of 1-2nd generation cephalosporins (cephalexin, cefaclor, cefuroxime), as well as tetracyclines (doxycycline) is less preferable due to their isolated gram-positive spectrum of action. If high activity of Pseudomonas aeruginosa is suspected, carbenicillin, ticarcillin, azlocillin or piperacillin are used.
The persistent course of the microbial inflammatory process in the conditions of complex treatment of a trophic ulcer serves as an indication for microbiological culture with subsequent correction of the ongoing antibacterial therapy. Isolation of multiresistant strains determines the need for parenteral use of reserve group antibiotics (vancomycin, 3rd-4th generation cephalosporins, carbapenems) until the symptoms of acute cellulitis are completely resolved (on average 7-10 days). The presence of fungal flora in a trophic ulcer is an indication for the administration of fluconazole at a dose of 50–100 mg per day.
Phlebotropic drugs. RCTs and meta-analysis results show that MOFF (1000 mg per day) in combination with compression therapy accelerates the healing of venous trophic ulcers with an area of up to 10 cm² in up to 6 months. For other FLPs, there is no reliable data regarding their effectiveness in venous ulcers.
Local treatment of venous trophic ulcers.
Local therapy is a key stage in the treatment of trophic ulcers of venous etiology. The choice of specific therapeutic agents depends on the characteristics of the wound process, the condition of the tissues surrounding the trophic ulcer, and the limb as a whole.
Toilet trophic ulcer. When treating a trophic ulcer, jet washing of its surface with a sterile saline solution heated to 37°C can be considered optimal. The use of concentrated antiseptics (povidone iodine, hydrogen peroxide, miramistin, sodium hypochloride, etc.) traditionally used for acute wounds should be avoided. In conditions of trophic ulcers, they not only destroy microorganisms, but also have a cytotoxic effect, damaging granulation tissue. High-pressure lavage, including vortex therapy, is undesirable, as it promotes the penetration of microorganisms into the tissue and damages the microvasculature. Surgical debridement or debridement is performed when there is a large amount of necrotic tissue and fibrin. At the same time, during the procedure one should not strive to expose the bottom of the trophic ulcer.
Wound coverings. Local physicochemical conditions have a significant influence on the normal course of reparative processes in the area of the ulcer. On the one hand, excess humidity causes the death of epithelial cells. On the other hand, lack of moisture leads to drying out and slows down the epithelization process. Severe disturbances in the gas composition and acidity of the environment also adversely affect the functional cellular activity, and in certain cases create conditions for the activation of pathogenic microflora. It has been proven that a moist environment is necessary for wound self-cleaning, proliferation and migration of epithelial cells. With a sufficient amount of fluid in the extracellular matrix, looser fibrous tissue is formed with the subsequent formation of a less rough, but more durable scar.
The greatest prospects in the treatment of trophic ulcers of venous etiology are associated with the use of new generation wound coverings. The main objectives of such dressings are:
- irreversibly remove detritus, microbial particles and excess exudate;
- protect from mechanical influences, chemical irritation and
secondary infection;
- keep the ulcer surface moist,
preventing it from drying out and forming a dry scab;
- help increase the reparative resources of local tissues;
- maintain microcirculation and oxygenation of the edges of the ulcer;
- have a beneficial effect on the surrounding skin, protect it from maceration,
allergies and dermatitis;
- stay on the wound and be removed painlessly and atraumatically;
- retain their properties when combined with elastic compression in
over a long period of time (a day or more);
- be easy to use and comfortable for the patient.
The so-called interactive dressings have all of the above properties to the greatest extent (Table 8). These are bandages of complex pathogenetically targeted action, capable of creating and maintaining in the pathological focus for a long period of time an optimal wound environment for healing with a balanced level of humidity and sorption of wound exudate and, as a result, ensuring timely cleansing and normalization of reparative and regenerative processes in the wound. Interactive dressings, as a rule, have low adhesion to the wound surface and are able to maintain a constant gas composition and pH level of tissues.
Table 8. Modern dressings used for the treatment of venous trophic ulcers.
| Groups of dressings | Wound process phase | Degree exudation | Functional properties |
| Super-absorbing titels | 1 — 2 | Wounds with moderate or severe exudation | Absorb liquid, promote rapid wound cleansing, stimulate proliferation processes, and have low adhesion. Protects against recurrent and secondary infection. Pairs well with elastic compression. |
| Sponge- thin bandages | Vapor permeable. Actively absorb liquid, maintaining a balanced, moist environment. Clean the ulcer surface from fibrin. Stimulate granulation, protect the skin from maceration. Hydrophilic sponges protected by a hydroactive gel layer allow for local treatment from the moment of cleansing to complete epithelization of the ulcer. Pairs well with elastic compression. | ||
| Algi- natural headbands | Irreversibly binds fluid, maintaining a balanced moist environment and promoting wound cleansing, drainage and hemostasis. Stimulates the growth and development of granulation tissue. Do not interfere with microcirculation and oxygenation of the edges of the ulcer. Require additional use of secondary dressing and fixation means. | ||
| Hydro- gels | 2 — 3 | Minimal exudation wounds | They create and maintain a moist environment for a long time and are transparent. Moderately absorb and clean, reduce pain, non-adhesive. |
| Hydro- colloids | 2 | Wounds with small or medium exudation | Vapor permeable. Partially permeable to air. Absorb liquid, stimulate granulation and epithelization, protect against secondary infection. |
| Atraumatic mesh dressings | All phases | Well permeable, easily modeled on wounds of complex configuration. They do not stick to the wound, protect granulations, but require the additional use of a secondary dressing and fixation means. |
The choice of one or another dressing requires mandatory consideration of the phase of the wound process and the degree of exudation. Thus, dressings, the use of which is rational in the inflammation phase, due to the structure of their material, are capable of inactivating wound exudate, promoting the irreversible elimination of microorganisms, toxins and tissue detritus, while stimulating the process of rejection of necrotic tissue. In turn, coatings used in the treatment of “clean” healing ulcers maintain the necessary humidity and aeration, reliably protect against mechanical damage and secondary contamination, and stimulate reparative processes.
Atraumaticity and safety are the most important properties of modern interactive dressings. Non-traumatic means that the coating can be easily removed due to the low degree of adhesion to the wound surface. Safety means the absence of mechanical and chemical irritation, as well as hypoallergenicity. An additional advantage is their modeling ability, which allows closing a wound defect of any shape in various parts of the body. Many wound dressings are self-adhesive or have an additional self-adhesive edge treated with a hypoallergenic adhesive. Such dressings should only be used in patients with normal skin sensitivity in the absence of dermatitis and/or eczema. Modern interactive dressings are produced in ready-made sterile packaging, with markings that ensure ease of use.
Superabsorbents are capable of absorbing and irreversibly sorbing wound discharge. They are a multilayer pad that contains as an active substance a granular polyacrylate superabsorbent that has a high degree of affinity for wound fluid proteins. The saline solution, which soaks the wound covering continuously for 24 hours, is released into the wound and replaced by exudate, providing wound dialysis and microbial decontamination. Moisturizing necrosis helps to soften it, make it easier to reject and clean the wound. Currently, further improvement of the “washing-absorption” mechanism, reducing adhesive properties and creating conditions for complete irreversible inactivation of absorbed microflora through the introduction of the antiseptic polyhexamethylene biguanide (PHMB) into the absorption element makes it possible to increase the intervals between dressings to 72 hours without the threat of re-infection of the ulcer.
Alginates are produced from seaweed. They are based on the calcium salt of alginate acid, as well as polymer chains of mannuronic and hyaluronic acids. Alginate dressings are placed in the wound dry. Upon contact with blood and wound secretions, due to the swelling of the fibers, they turn into a hygroscopic non-adhesive gel that fills the wound. In this case, microorganisms and toxins are reliably bound in the gel structure. As a result, wounds are quickly cleansed and a microclimate favorable for healing is created. A prerequisite for the use of calcium alginate-based dressings is the presence of fluid in the wound. The dressing is used in all phases of the wound process with moderate and severe exudation up to complete epithelization. Calcium alginate has hemostatic properties and can be used to treat deep and/or bleeding ulcers. Contraindications to the use of calcium alginate-based dressings are dry necrotic scab and the presence in the wound of elements that are not a source of granulation tissue growth (abundance of open tendons, joint capsules, periosteum, etc.).
Sponge dressings consist of synthetic spongy materials, the therapeutic effect of which is based on the effect of vertical capillarity and low adhesion. They are able to create a balanced environment on the wound surface, stimulate the growth of granulation tissue and isolate the ulcer from secondary infection. Used in the treatment of trophic ulcers with abundant exudation in the first and second phases of the wound process. The advantage is that the structure of the material allows them to be combined with elastic compression without reducing the sorption properties of the wound covering. The indication for changing the dressing is its complete saturation with exudate, manifested by leakage of liquid or deformation of the outer layer of the coating.
Currently, hydrophilic sponge dressings protected by a hydroactive atraumatic coating have been developed and introduced into the domestic market. A mesh atraumatic hydrogel coating with an initial 35% moisture content, which is the contact layer of the dressing, can significantly reduce the adhesion of the sponge to the wound surface and effectively moisturize even a dry ulcerative surface. The prolonged release of fluid with such a dressing allows you to ensure the necessary balance of moisture and sorption from the moment the ulcer is cleansed of detritus until its complete epithelialization. The bandage also does not lose its properties if elastic compression is used and can remain on the wound for an average of 3-5 days.
Hydrocolloids are used in the 2nd phase of the wound process. Upon contact with wound exudate, the colloidal component swells and turns into a gel. The main advantages of these coatings include good fixation to the wound surface, high atraumaticity, and easy modeling of the shape of both the limb and the ulcerative defect. The disadvantage of hydrocolloids is their opacity, which makes it difficult to visually monitor the condition of the wound defect. The saturation of hydrocolloids and loss of sorption activity is indicated by the deformation of the bandage in the form of a bubble and a change in its color. When changing the dressing (on average every 2-3 days), the remainder is removed from the wound surface with a damp swab. Low sorption capacity, as well as insufficient permeability to gases and water, limits the use of hydrocolloids in severe exudative processes.
Hydrogel dressings are a ready-made sorption gel fixed on a transparent semi-permeable membrane containing up to 60% water and possessing moderate sorption activity. The gel maintains a constant shape and keeps the wound moist while absorbing excess secretions. These coatings are used to rehydrate dry necrotic scab or stimulate epithelization of granulating ulcerative defects. Hydrogel-based dressings do not stick to the wound, which makes them highly atraumatic. The outer surface of the coating is impermeable to microorganisms and water and at the same time transparent. The last factor makes it possible to visually monitor and record the condition of a trophic ulcer without removing the bandage. The indication for changing the coating is its cloudiness and loss of transparency.
Atraumatic mesh dressings are made on the basis of a neutral hypoallergenic hydrophobic ointment mass or Peruvian balsam. They have an antiseptic effect and stimulate tissue repair. The advantage of atraumatic mesh dressings is the ability not to stick to the wound and not to interfere with the outflow of excess wound fluid. Along with being atraumatic, this factor protects the coatings from drying out and prevents the formation of scar contractures. Silver-containing atraumatic dressings have a more significant antimicrobial effect. Upon contact with the wound surface, there is a slow, uniform release of active silver particles, which have a wide spectrum of antimicrobial activity. The service life of such a dressing, subject to moderate exudation, is 7 days. Atraumatic dressings are used to cover donor sites during autodermoplasty of trophic ulcers.
Additional methods of local treatment of venous trophic ulcers. Additional methods of local therapeutic effects on the area of a trophic ulcer include laser irradiation, vacuum treatment of the wound, its biological sanitation and treatment in a controlled abacterial environment.
Laser radiation. The use of laser radiation is rational in the first phase of the wound process. When treating an infected wound, its surface layers are evaporated to form a thin-walled, sterile scab. These processes are accompanied by a significant decrease in the degree of microbial contamination of the ulcer. The greatest therapeutic effect of laser radiation was obtained when affecting trophic ulcers of a small area.
Vacuum treatment of trophic ulcers . Vacuuming is one of the methods of sanitation of chronic wounds, which can also be applied to trophic ulcers of venous etiology. The main pathogenetic aspects of vacuuming are the removal of weakly fixed non-viable tissues, a significant reduction in the degree of bacterial contamination of tissues and stimulation of reparative processes. Improving stationary and mobile devices that provide prolonged vacuum exposure, equipping them with a dialogue program and an emergency warning system, makes it possible to solve the problem of treating chronic wounds at a completely new level.
Biological rehabilitation of trophic ulcers . Currently, there is renewed interest in the method of cleansing purulent-necrotic ulcers using green fly larvae (Larval therapy). Specially grown larvae, when placed in a wound, have a cleansing effect through the release of powerful proteases. Under their influence, devitalized tissues undergo necrolysis, become amorphous and are absorbed by the larvae. The main problem of biological sanitation of trophic ulcers is the ambiguous ethical and aesthetic perception of the method by doctors and patients.
Treatment of trophic ulcers in a controlled abacterial environment. The method of bandage-free treatment of extensive purulent wounds in a controlled abacterial environment is based on the principle of gnotobiological isolation. The area of ulcerative defects is isolated from the external environment in a transparent plastic chamber and a stream of sterile air is constantly supplied to it, creating an optimal environment for wound healing. The disadvantage of the method is its cumbersomeness, the possibility of performing it only in a hospital setting, as well as a significant reduction in the quality of life of the patient who is forced to observe strict bed rest for a long time.
Compression therapy is a necessary component of the treatment of venous trophic ulcers and the prevention of their recurrence. In case of an open ulcer with symptoms of venous edema, cellulite and exudation, preference is given to multilayer bandages formed from bandages of limited extensibility. To prevent relapse, medical compression stockings are usually used.
Algorithm for local treatment of venous trophic ulcers
Ist phase of the wound process. A large amount of necrotic masses and fibrin is an indication for the use of wound dressings from the superabsorbent group in combination with a multilayer compression bandage. The dressing is changed daily. For high or moderate exudation, it is recommended to use sponge, alginate or atraumatic dressings with antiseptic properties in combination with secondary sorption dressings. The antibacterial properties of drainage and sorption dressings can be enhanced by the additional use of atraumatic silver-containing coatings. Wound coverings and compression bandages are applied for at least 24 hours. If the swelling subsides quickly, then the bandage is changed daily, regardless of the type of interactive bandage.
II phase of the wound process. For high or moderate exudation, sponge dressings are used. If the skin surrounding the ulcer is hypersensitive, sponge dressings with a fixing contour should be avoided. At low and medium levels of exudation, in the second phase of the wound process, hydrophilic sponges protected by a hydroactive gel layer or hydroactive occlusive dressings are used, which best stimulate the healing of a chronic wound. Only with a minimal level of exudation in the second phase of the wound process can one abandon the use of wound occlusion in favor of atraumatic dressings, which can be considered as the treatment of choice in the treatment of chronic wounds in conditions of moderate or low exudation with sensitive skin surrounding the ulcer. For normal skin sensitivity, the preferred local treatment option in the second phase is hydrocolloid dressings, which best stimulate the formation of granulations.
In conditions of an actively granulating trophic ulcer, both in the presence of edema and in its absence, compression therapy can be carried out using a multilayer bandage, including special bandages impregnated with zinc oxide and glycerin.
III phase of the wound process. During the epithelialization stage, the algorithm for local therapeutic effects on venous ulcers is somewhat simplified due to a significant reduction in the severity of exudative processes. For normal skin, it is possible to continue treatment with sponge dressings with a hydroactive layer, as well as local application of thin-layer hydrocolloid and hydrogel dressings. For sensitive skin, the optimal treatment option is hydrogel coatings without a fixing contour or hydroactive atraumatic dressings. As a rule, at this stage of the pathological process, swelling of the limb is insignificant, which makes it possible to widely use medical compression hosiery. If swelling of the limb persists, multi-day compression bandages are used.
Surgery
Obtaining a clear clinical effect from conservative therapy for 6 weeks, consisting in reducing the area and depth of the trophic ulcer, improving the trophism of surrounding tissues, eliminating edema and pain, allows us to recommend its continuation until the complete closure of the trophic ulcer. With an active trophic ulcer, the indication for surgery is the ineffectiveness of adequate conservative treatment.
All types of surgical interventions performed in patients with trophic ulcers can be divided into two groups. In the first case, the task of the surgical treatment is to eliminate pathological regional venous hypervolemia, in the second - plastic closure of the trophic ulcer.
Operations on the superficial venous system
For varicose veins with high venovenous discharge, a crossectomy is performed followed by stripping of the great saphenous vein on the thigh. Extended phlebectomy on the lower leg, which is fraught with purulent-necrotic complications, should be avoided. In high-risk patients, as well as as a means of eliminating residual varicose veins, phlebosclerosing treatment, laser and radiofrequency coagulation are used.
Interventions on perforating veins
To eliminate horizontal reflux, endoscopic dissection of perforating veins is used, as well as their scleroobliteration or thermal coagulation under ultrasound control.
Deep vein interventions
Surgical interventions on the deep venous system (plasty of venous valves, shunt operations) in patients with trophic ulcers are performed in an extremely limited group of patients in case of failure of all other treatment methods.
Skin grafting
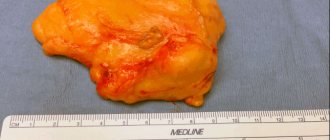
A large area of trophic ulcer sometimes requires surgical repair of the tissue defect. For this purpose, autodermoplasty with a split skin flap is used, both as an independent method and in combination with intervention on the saphenous and perforating veins.
As a rule, the anterolateral surface of the thigh is used as a donor area. A skin flap with a thickness of 0.5 – 0.8 mm is collected using a mechanical, or less commonly, a manual dermatome. After application of donor skin over the entire area of the trophic ulcer, the wound surface is covered with a non-adhesive bandage and a compression bandage is applied for 3 to 5 days. In order to close the donor area, it is most rational to use atraumatic mesh bandages.
Symptoms of psoriasis on the hands
The disease can begin and progress differently depending on the form. Symptoms of psoriasis on the hands can also vary.
Vulgar form
This is the most common form. On the hands, the skin of the extensor area of the joints, as well as the forearms, wrists, dorsum of the hands, and fingers are usually affected. In the area of the elbows, so-called standby plaques appear on both sides, which can remain in the same state for years without progressing. On the back of the hands, the disease progresses more often, since the skin in these areas is constantly exposed to various influences. Psoriasis often appears on the fingers. In case of damage to the little fingers and thumbs, the risk of injury to psoriatic elements increases.
The first signs of psoriasis on the hands are the appearance of one or more scaly spots, which quickly turn into papules with a raised inflammatory base. If you scratch the top of such a papule, a number of characteristic symptoms appear:
- type of stearin drop - multiple white flakes;
- if you scrape off all the scales, a transparent film will be visible;
- Slightly scraping the film leads to the appearance of droplets of blood on it.
These symptoms are the hallmark of a psoriatic rash. In the future, the primary symptoms of the disease may progress, with the papules increasing in size, merging with each other and forming large plaques, and new elements appear. Possible damage to nails. Over time, the progression stops, after which the recovery process begins: the rash slowly turns pale and disappears.
Exudative form
This form of the disease is less common. The skin on the back of the hands is usually affected. Often this type of psoriasis also affects the fingers. Characterized by the appearance of swelling, exudate on the surface of the rash elements, severe itching and a constant feeling of discomfort. As a result, the scales stick together to form grayish-yellowish crusts on the surface of the papules on the skin of the hands and fingers. In this case, peeling is not very noticeable, but the risk of bacterial infection increases. What exudative psoriasis looks like on the hands can be seen in the photo:
Palm shape
Psoriasis on the palms can occur in the form of plaque-fan-shaped, horny and pustular forms.
The plaque-fan-shaped form is characterized by the formation at the initial stage of rash elements in the form of scaly papules, merging into large plaques. The rashes are localized mainly on the palms and fingers. It often recurs and is difficult to treat. The reason for this is the constant exposure to various external factors. The skin between the fingers is affected. They turn red, swell, and become covered with cracks and scales. Often such rashes spread to the fingertips and nail plates.
The horny form is manifested by dry skin, thickening on the palms, the appearance of cracks and dry calluses.
Psoriasis on the palms of the hands may look like pustules. This is the so-called Barber pustular psoriasis. Purulent blisters appear on the surface of the palms, which can merge with each other, forming purulent lakes. The contents of the pustules are sterile. Photo:
Treatment methods for psoriasis on the hands
How to treat psoriasis on the hands? This problem arises immediately after diagnosis. Experts recommend comprehensive treatment, which includes:
- changing lifestyle, daily routine;
- getting rid of bad habits;
- proper nutrition;
Lifestyle recommendations
Patients with psoriasis localized on the hands need to:
- regulate wakefulness and sleep patterns;
- engage in feasible sports; Activities such as outdoor running, swimming, tennis are welcome; avoid contact sports (wrestling);
- important: after playing sports, be sure to take a shower - sweat irritates the skin and can provoke an exacerbation of the pathological process;
- wash only with soft washcloths using hypoallergenic detergents;
- After a shower, apply moisturizer to your body;
- use underwear made from cotton fabrics;
- in the cold season, wear gloves (mittens) with flannel lining;
- Avoid contact with household chemicals and any other chemicals.
Drug therapy
Good to know
- Treatment of psoriasis on the head
- Treatment of psoriasis on the elbows
- Treatment of psoriasis on the legs
- Treatment of psoriasis on nails
- Treatment of psoriasis on the face
- Treatment of palmoplantar psoriasis
In mild cases, psoriasis on the hands is treated locally, using various external agents and procedures. Prescribed:
- keratolytics - medicinal ointments and creams that dissolve surface layers of dead epithelial cells (salicylic acid);
- emollients (tar-based psoriasis ointment);
- synthetic analogues of vitamin D (calcipotriol);
- synthetic analogues of vitamin A (retinoids);
- glucocorticosteroid (GCS) hormones - allow you to treat all forms of hand psoriasis;
- combination products that include GCS + salicylic acid (Diprosalik) or GCS and calcipotriol (Daivobet);
- creams and ointments with active zinc;
- medicinal baths with herbs (celandine, chamomile, calendula).
If the symptoms of psoriasis on the hands do not go away, the disease progresses, and general therapy must be prescribed. It should be carried out in a hospital setting:
- droppers with medicinal solutions that eliminate intoxication;
- injections of drugs that remove toxins (Unitiol, magnesium sulfate);
- desensitizing (eliminating allergies) and sedatives; 1st generation antihistamines (Suprastin, Tavegil) are most suitable;
- glucocorticoids - taken orally or by injection - have a pronounced anti-inflammatory and desensitizing effect, relieve itching;
- cytostatics - drugs that suppress too frequent division of epithelial cells;
- Immunosuppressants are medications that suppress the excessive sensitivity of the immune system.
Treatment of ulcers
Treatment of trophic ulcers should be carried out using complex methods: it is necessary not only to eliminate the local manifestation of the process, but also to fight the cause of the disease. For this purpose, surgical and medicinal methods are used. When microbial infection develops, detoxification therapy is carried out, which removes decay products of microbial cells and improves the patient’s condition. Great importance is attached to normalizing the work and rest regime and wearing special compression garments. Reviews about the treatment of trophic ulcers indicate the effectiveness of physiotherapeutic procedures.
In the multifunctional clinic "MedicCity" you will be able to offer full-fledged treatment using modern, unique equipment. So start your treatment now. After all, not only your health, the degree of your recovery, but also your life depends on how quickly you see a doctor!
Unique methods for treating psoriasis on the hands
The Moscow Paramita Clinic is a leader in the treatment of such a complex form of the disease as psoriasis on the hands. Experienced specialists who have undergone all the necessary training in the treatment of this disease try to take an individual approach to the treatment of each patient, using the most effective methods.
- PRP therapy is a method that has been used relatively recently, but has already gained well-deserved popularity, as it is very effective and safe; the method consists of enriching the patient’s blood taken from a vein with platelets and injecting it into the affected areas on the skin of the hands;
- autohemotherapy is a method that has been tested for decades: blood is taken from the patient’s vein and injected intramuscularly; excellent stimulating effect;
- herbal medicine – the use of medicinal plants using modern methods;
- reflexology – exposure to certain points on the body using various methods (acupuncture, massage, cauterization, etc.); exposure to one point or another has a reflex effect on the condition of the skin;
- vacuum therapy is one of the types of reflexology, when certain points and zones are affected using vacuum.
The clinic’s dermatologists prescribe complex therapy taking into account the patient’s age, general condition, the presence of certain concomitant diseases, as well as the nature of the course of psoriasis. As a result of this approach, the patient receives the necessary treatment for psoriasis in Moscow without side effects, which allows him to get rid of the symptoms of the disease for a long time.
To avoid relapses, it is necessary to eliminate the cause of the disease.
Read more about our unique method of treating psoriasis
Patients return to the clinic again and again for maintenance anti-relapse treatment and live for years without exacerbations. In the reviews, they note the high professionalism and attentive attitude of the doctors.
Sign up for a free initial appointment
Treatment
After identifying the main cause that led to the development of trophic ulcers on the hands, adequate therapeutic measures are selected. For antibacterial purposes, antibiotics are prescribed - Ceftriaxone, Amoxicillin, Tetracycline. Venarus and Detralex are used to strengthen blood vessels and restore impaired blood flow. For shallow/superficial ulcerative defects, the use of healing ointments is recommended for topical application. These include Zinc ointment, Argosulfan, Solcoseryl and Levomekol.
Surgical treatment consists of excision of the edges of the ulcer and rinsing with antiseptic drugs (Betadine, Furacillin). If purulent contents are present, drainage is installed.
Stages of hand psoriasis
The disease occurs in alternating phases of relapses and remissions. The course can be severe, moderate or mild. During an exacerbation, the disease goes through several stages. Psoriasis on the hands, stages:
- the initial stage of progression - a psoriatic rash appears, the symptoms of the disease quickly increase;
- stationary – no new elements appear, the rashes do not fade or become smaller;
- regressing - the rash turns pale, swelling subsides, all signs of exacerbation disappear, and gradually only white or brownish spots remain on the skin, which also disappear over time.
Any form of the disease, in the absence of adequate treatment, can be complicated by joint damage and erythroderma - inflammation of large areas of skin with severe swelling and redness.
Stages of development and symptoms
Severe pathological changes in the body never appear suddenly. A trophic ulcer develops gradually and is preceded by many symptoms that may remain unnoticed for a long time. In the very first stages of development, the disease looks more like a small dark spot in the ankle or lower leg area. Patients attribute minor pain to fatigue or prolonged walking.
It is important to begin treatment of trophic ulcers of the lower extremities of venous origin in the first stages of development.
- The initial stage of a trophic ulcer (pre-ulcer). The first prerequisites are associated with a burning and itching sensation in the calves and lower legs. The patient observes compaction on the legs, sometimes there are pronounced venous formations that are visible to the naked eye. Such symptoms usually go unnoticed because... The disease does not cause severe discomfort. Over time, the affected areas of the skin acquire a red or purple tint, and the spots usually merge into a single whole. The ulcers themselves are not observed, but everything is ready for their formation.
- Exudation stage. This stage of disease development lasts up to 14 days and is characterized by perifocal edema, inflammation and tissue necrosis in the center of the inflamed area. If the affected area of the leg was characterized by the presence of a large number of lymphatic vessels, then complications are possible: lymphagiitis, vein thrombosis. An unpleasant odor liquid is usually released from the wound, which indicates an accumulation of microbes. If the disease is not stopped, then persistent swelling and disability gradually develops.
- Granulation stage. In the next 2-3 weeks, the repair stage begins, that is, the wound is gradually cleansed of necrosis, the swelling subsides.
- Epithelization stage. This is a late stage of development, the surface is covered with epithelium where possible. The most severely affected areas become scarred.
Trophic ulcer is an insidious disease that does not cause severe discomfort to the patient for a long time, which is why patients come to the clinic at an advanced stage. You should not make an independent diagnosis and expect the disease to move to a new stage. Symptoms for each person can be individual, so it is better to immediately consult a doctor.
How to eat healthy
Nutrition is of particular importance as it affects metabolism, the disturbances of which underlie the disease. It is useless to treat psoriasis without following a diet. Important: in the patient’s diet, 70% should be products of plant origin and only 30% should be animal products. Recommended to use:
- any fruits and vegetables (fresh, boiled, stewed) except those prohibited;
- fresh juices; Citrus juices are especially useful; lemon juice can be used as a salad dressing;
- more clean water.
Limit consumption (no more than a few times a week):
- lean meat and fish;
- low-fat cottage cheese and fermented milk products;
- cereals;
- some fruits and berries: plums, currants, cranberries, blueberries.
Exclude from the diet:
- fat meat;
- fatty dairy products;
- sweets, baked goods;
- vegetables from the nightshade family: tomatoes, eggplants, hot and bell peppers;
- all spicy, sour, smoked, fried, canned foods;
- drinks: sweet soda, cocoa, strong coffee, tea, alcohol.
Treatment of psoriasis on the hands with folk remedies
Folk remedies are widely used in the treatment of psoriasis on the hands. Celandine is especially often used for this purpose. For example, a serum infused with celandine helps a lot.
You need to take a glass of crushed fresh celandine herb, wrap it in a cotton napkin, tie it, put it in a 5-liter glass jar, fill it with three liters of whey, add 200 g of sugar, 20 g of sour cream and leave in a warm place for 15 days: during this time the whey will ferment ; this serum should be filtered and taken 70 ml in the morning 30 minutes before meals; store in a cool place; perfectly removes toxic substances, cleanses the body, activates metabolism; the symptoms of the disease go away.
Prevention of psoriasis on the hands
Prevention of the disease includes patient compliance with recommendations on daily routine, skin care and nutrition.
Psoriasis on the hands is best treated in the early stages of the pathological process. It is impossible to completely cure this process, since under the influence of any factors a relapse may begin. But if maintenance treatment is carried out periodically, remission for a long time is quite possible. At the same time, the person lives life to the fullest and does not remember relapses.
Causes
The main reason for the development of such defects is not only vascular diseases. Often, trophic ulcers occur against the background of neoplasms localized in the axillary, subclavian and mediastinal lymph nodes. In addition, injuries of various types (stabbed, cut, chopped, bitten), infectious and inflammatory diseases (chickenpox, helminthic infestations), pathologies of the immune system, systemic connective tissue diseases (lupus erythematosus, vasculitis), sepsis cause aggravation of the skin syndrome and the development ulcerative defects on the hands.