Palmoplantar psoriasis in the photo with description
Photo 1. Provoking factors for psoriasis: obesity.
Photo 2. Provoking factors for psoriasis: smoking and alcohol.
Photo 3. Psoriasis on the palms.
Photo 4. Psoriasis on the soles of the feet.
Photo 5. Symptoms of palmar psoriasis: peeling and the appearance of a red crust.
Photo 6. Symptoms of palmar psoriasis: peeling of the nail plates.
Causes of palmoplantar psoriasis
In most cases, the palmoplantar form appears due to congenital or acquired characteristics of the immune system or is transmitted genetically. A combination of both factors is possible.
Without provoking factors, the disease may not manifest itself at all. Here are the main reasons that can give rise to the appearance of a rash:
- past infections (viral and bacterial);
- the presence of inflammatory processes in the body;
- a course of medications (arsenic-based, beta-blockers, oral contraceptives, etc.);
- drugs, smoking and alcohol abuse;
- overweight, metabolic disorders;
- pathologies of the heart and blood vessels;
- disturbances in the functioning of the endocrine system;
- severe or prolonged stress.
With psoriasis, the immune system too actively produces protective substances, the aggression of which is directed at its own tissues and cells. As a rule, these are T lymphocytes. Their activity provokes inflammation and excessive cell division. This is what causes the symptoms. The risk group includes people from 30 to 50 years old.
There are different degrees of pathology, which is especially evident on the hands. Therefore, in the case of psoriasis on the palms, photos of the initial stage may differ.
When should you contact your healthcare provider?
Call your healthcare provider if you experience any of the following.
- temperature 100.4°F (38°C) or higher;
- chills;
- symptoms do not go away or get worse;
- any of the following symptoms appear on the skin of your palms or soles: skin that is hard, warm, or hot to the touch;
- bright yellow or green discharge;
- bleeding.
- unpleasant odor from the palms and feet;
- increasing redness or swelling;
- increasing pain or discomfort;
to come back to the beginning
Symptoms of palmoplantar psoriasis
Standard clinical manifestations:
- inflamed areas of pink or red color with clearly defined boundaries;
- severe peeling on top of the rash (clearly visible in the photo of psoriasis on the palms of the hands);
- painful cracks in areas with rashes (not always the case);
- pustules (rash with purulent contents, characteristic of some types of psoriasis);
- intense itching and burning (does not appear in all patients).
The disease has different forms. Therefore, some symptoms may vary.
If you discover suspicious symptoms, you should contact a dermatologist as soon as possible. You should not diagnose yourself by studying photos of palmoplantar psoriasis.
Medicines that may cause a reaction
Hand-foot syndrome
The following medications may cause hand-foot syndrome.
- capecitabine (Xeloda®);
- Doxorubicin (Adriamycin®)
- Fluorouracil (5-FU®)
- Liposomal doxorubicin (Doxil®)
- Cytarabine (Cytosar-U®)
Palmoplantar skin reaction
The following medications may cause hand-foot reaction.
- Sorafenib (Nexavar®)
- Sunitinib (Sutent®)
- Cabozantinib (Cometriq®)
- Regorafenib (Stivarga®)
- Axitinib (Inlyta®)
- Pazopanib (Votrient®)
- Vandetanib (Caprelsa®)
- Vemurafenib (Zelboraf®)
- Dabrafenib (Tafinlar®)
to come back to the beginning
Types of palmoplantar psoriasis
There are two main types of palmoplantar psoriasis: ordinary and pustular (Barber type).
Ordinary psoriasis manifests itself as follows:
- In the area of the palms (often closer to the big toe and little finger) or soles (heel, lateral surface of the foot and area of the metatarsophalangeal joints), clearly defined, inflamed areas of reddish-yellow skin form. With severe exacerbation of the disease, the rash may occupy the entire palm or sole.
- in some cases, a large number of rough scales accumulate on the surface of the rash, forming deep and painful cracks
Pustular palmoplantar psoriasis (Barber psoriasis) is additionally characterized by the presence of pustules - intradermal accumulations of whitish-yellow pus. Purulent rashes can form both on top of plaques and on clean skin.
The pustular subtype develops quickly, is characterized by frequent relapses and is difficult to treat. Treatment for Barber psoriasis differs significantly from treatment for other subtypes.
How is psoriasis diagnosed in children?
The basis of diagnosis is a physical examination, clinical assessment of characteristic signs and changes on the skin.
At the appointment, the doctor evaluates:
- location, nature of the rash;
- presence of nail lesions in children due to psoriasis;
- presence of pain in bones and joints;
- the presence of weakness, increased fatigue, frequent respiratory infections;
- excess body weight, diabetes mellitus.
A family history is also collected: psoriasis is inherited by children, so the presence of the disease in one or both parents is an important factor.
If psoriasis is suspected, the doctor must conduct diagnostic tests:
The presence of the Koebner phenomenon
This phenomenon is characterized by the appearance of new rashes in the area of skin irritation. For example, in the area of scratches, burns, fresh tattoos.
Symptom of psoriatic triad
Consists of three specific sequential actions that are performed by the doctor during a face-to-face appointment.
- The stearin stain phenomenon is an increase in peeling after scraping, giving the surface of the papules a resemblance to a crushed drop of stearin.
- The phenomenon of terminal film is the appearance after complete removal of the scales of a wet, thin, shiny, translucent surface.
- The phenomenon of blood dew - after a short scraping of the element, small droplets of blood appear.
In severe forms of psoriasis in children, laboratory tests, general and biochemical blood and urine tests are recommended. This is necessary to assess the patient’s general condition and identify contraindications to systemic therapy.
If it is necessary to carry out differential diagnosis with other skin diseases, a pathological examination of biopsy material of the affected skin is recommended.
Treatment methods for palmoplantar psoriasis
Palmar and plantar psoriasis requires complex treatment using systemic medications, external agents and physiotherapeutic techniques. Since it is impossible to completely get rid of psoriasis, therapy aims to relieve symptoms and prolong remission.
Systemic treatment involves the use of active anti-inflammatory drugs from the group of immunosuppressants (methotrexate, cyclosporine, etc.) or retinoids (acitretin).
For psoriasis on the palms and back of the hands, external treatment includes:
- glucocorticosteroids (hormonal creams and ointments) - this group of drugs most effectively copes with the inflammatory process in the skin and requires mandatory medical supervision during the treatment period.
- vitamin D and its analogues;
- non-hormonal external preparations - products containing naphthalan, salicylic acid, urea, tar are suitable for use both during exacerbation of the disease and during remission. This group of drugs rarely causes side effects and can be used independently by patients.
- emollient creams;
In addition to medications, physiotherapy is actively used. Typically it includes the following procedures:
- exposure to UV rays (natural or hardware);
- PUVA therapy;
- excimer laser treatment;
Treatment methods are selected by a dermatologist, guided by the severity of the disease and the characteristics of the patient’s body. The key difficulty in selecting drugs is their compatibility and contraindications. In addition, for therapy to be effective, medications must be rotated in terms of their level of anti-inflammatory activity. Therefore, you cannot self-medicate.
Patients often visit a dermatologist with complaints of thickening, redness, dryness, peeling of the skin of the palms and soles, and painful cracks. A similar picture of palmoplantar lesions can be observed in a number of diseases, which requires the doctor to conduct a thorough differential diagnosis. It should be borne in mind that lesions on the skin of the palms and soles are most often a fragment of a general lesion of the skin, and sometimes the mucous membranes. This necessitates a general examination of the patient and compliance with all the rules for making a dermatological diagnosis: a thorough history taking, a general examination of the entire skin and visible mucous membranes, identification of eruptive elements, comparing them with those in the area of the palms and soles; palpation of lymph nodes. If it is difficult to visually determine the primary eruptive elements, it is necessary to use methods of additional clinical examination (palpation, diascopy, layer-by-layer scraping, probe symptoms, etc.) and laboratory diagnostics, including histological examination of biopsies of the affected skin.
Erythematosquamous lesions of the palmoplantar zone are most often observed with psoriasis, mycoses, chronic eczema, papular syphilide, and keratoderma.
Palmoplantar psoriasis
This form is common. Rashes on the palms and soles may be part of the overall common clinical picture of psoriasis. In such cases, the diagnosis is usually not difficult. However, in a number of patients, psoriasis can debut on the palms and soles, selectively relapsing for many years only in these locations. Recently, palmoplantar psoriasis has often begun to debut for the first time in women during menopause and menopause, clinically resembling acquired keratoderma.
There are 3 main clinical forms of palmoplantar psoriasis [1, 2]:
- typical papular-plaque;
- so-called horny, or “psoriatic calluses”;
- vesiculopustular.
Typical form of palmoplantar psoriasis
manifests itself as clearly demarcated dense, flat (almost not protruding above the surface), erythematosquamous papules from lenticular to plaque size. The surface of the rash is covered with abundant silvery-white scales, which, unlike other localizations of psoriasis, are difficult to separate. When scraped, the psoriatic triad is difficult to determine. This is explained by the physiological characteristics of the skin of the palmoplantar zone - a pronounced thickening of the epidermis due to physiological hyperkeratosis.
With this form of psoriasis, the rash often involves the marginal areas of the palms and soles, where it is easy to obtain the psoriatic triad and perform a diagnostic biopsy.
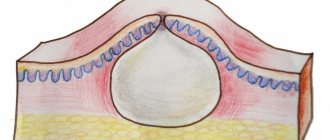
Severe infiltration and keratosis of the rashes lead to painful deep cracks in the skin of the palms and soles, decreased ability to work and overall quality of life. Palmoplantar fissures can become infected, creating conditions for recurrent erysipelas (Fig. 1).
Figure 1. Psoriasis of the palms and soles. Typical form.
“Horny” form of palmoplantar psoriasis
characterized by a predominance of foci of rounded keratoses without pronounced erythema. The lesions are dense to the touch, barely peel, have a yellowish color, and are covered with a dense horny mass. Lesions can vary in size from lenticular papules to large plaques. Lenticular-numular lesions may clinically resemble calluses (“psoriatic calluses”) and papular lesions of the palms and soles of secondary syphilis. Sometimes you can observe a fusion of large “horny” psoriatic papules, covering the entire area of the palms and soles, which clinically may resemble a squamous-hyperkeratotic form of mycosis, as well as keratoderma (Fig. 2).
Figure 2. Psoriasis of the palms.
Horny form. Vesicular-pustular form of palmoplantar psoriasis
(Barber type) is relatively rare. It can manifest itself as single vesiculopustules against a background of diffuse erythema, or as typical psoriatic papules and plaques, on the surface of which there are multiple tense superficial pustules with a diameter of 1-2 mm. Pustules can merge into larger cavity elements (so-called purulent lakes). As a rule, the rashes are symmetrical. On the palms, the tenor, hypotenor, and fingertips are affected, involving the area of the periungual bed (very similar to the Hallopeau acrodermatitis clinic). Single large lesions of the skin of the palms and soles may resemble Andrews bacterid (Fig. 3).
Figure 3. Pustular psoriasis of the soles.
Barber type. Microbiological and virological examination of the contents of pustules in palmoplantar psoriasis, Gallopo's acrodermatitis and Andrews bacteridus does not reveal any microflora. Pustules are sterile [3-5].
The histological picture of pustular psoriasis and Gallopo's acrodermatitis is identical: parakeratosis and pronounced acanthosis are observed in the epidermis, subcorneal spongiform Kogoi pustules are observed in the upper parts of the stratum spinosum, and an inflammatory infiltrate with a large number of neutrophils is observed in the dermis.
Differential diagnosis of palmoplantar psoriasis
Differential diagnosis is carried out with clinically similar psoriasiform conditions.
Squamous-hyperkeratotic forms of mycosis of the feet and palms.
As a rule, with this form of mycosis there is no intense inflammation. The clinical picture is dominated by hyperkeratosis, abundant diffuse peeling of the palms and soles. Cracks are most often observed along the edge of the heels. Often there is a change in the shape and color of the nail plates, marginal or total onycholysis, in other cases - hypertrophy of the nail plates up to onychogryphosis. In contrast to similar psoriatic changes in the nails, there are no telangiectasia of the nail bed and no visible areas of yellowing and deformation (“oil stain”) through areas of the intact nail around local areas of yellowing and deformation. When the lateral surfaces of the foot are affected, the process becomes erythematosquamous in nature and can imitate psoriasis (Fig. 4).
Figure 4. Mycosis of the foot.
Squamous-hyperkeratotic form. To confirm the diagnosis of mycosis, microscopic and cultural examination of skin scales should be performed. However, it must be remembered that in the area of the soles there may be typical and atypical forms of palmoplantar psoriasis, combined with mycosis [4]. In such cases, identification of psoriasis is difficult, especially if the patient does not have other clinical manifestations of psoriasis. In such cases, full-fledged antifungal therapy with external and systemic antifungal agents is advisable. In the case of initial mycosis, the clinical picture should resolve. If the causative agent of mycosis is eliminated (proven microscopically and culturally), but erythematosquamous changes in the skin and nail lesions remain, psoriasis should be suspected.
Eczema of the hands and feet.
Hand eczema usually occurs in patients with atopic status.
It can be acute or chronic. In the acute stage , on the back of the hands and feet,
the rashes are of a typical eczematous nature: against the background of edematous erythema, small vesicles appear, accompanied by itching. When scratching, multiple point erosions with abundant serous exudate are formed (the so-called Divergi wells). As the process becomes chronic, the clinical picture changes: infiltration and peeling of the affected skin areas increase. Against the background of lichenification, there may be cracks. Microvesicles are not visible clinically. The described clinical picture may resemble diffuse or papular-plaque skin lesions in psoriasis. However, when scraping in subacute cases, a symptom of pinpoint exudation can be observed; there are no symptoms of the psoriatic triad. It is very important to analyze the medical history, to find out the previous presence of bright erythema, edema and small blisters (Fig. 5).
Figure 5. Chronic eczema of the hands.
Psoriasiform lesion. Dyshidrotic form of eczema
is formed on the palms and soles more often in persons with a pronounced imbalance of the autonomic nervous system (increased sweating, persistent red dermographism, vascular lability) and with atopy [4]. Most patients associate the onset of the disease with severe stress. The clinical feature of this form of eczema is large (5-6 mm) cavity elements similar to blisters. In reality, they are fused multilocular spongiotic vesicles. Hyperemia and swelling are not clinically expressed. All this is explained by the thick stratum corneum on the palms and soles. Patients are bothered by intense itching and sometimes “tugging” pain. Cavity elements are preserved for a long time and do not open on their own (thick tire) (Fig. 6).
Figure 6. Dyshidrotic eczema of the hands.
Large tense vesicles. The lesion gradually spreads to the skin of the lateral surfaces of the fingers and to the back of the hands and feet. In this localization, eczematous rashes acquire a typical character: edematous erythema, microvesicles, erosions, crusts. Secondary suppuration of multilocular vesicles of the palmoplantar zone may clinically resemble pustular psoriasis of the palms and soles, as well as amicrobial pustulosis. Clinical differences of secondary suppuration of eczematous vesicles are an acute onset, an increase in pain, the appearance of lymphangitis and regional lymphadenitis, and an increase in body temperature. A variety of microbial flora is revealed in the purulent contents.
Microbial pustules.
This group includes diseases clinically similar to vesiculopustular psoriasis of the palms and soles [1, 2, 5].
Chronic acrodermatitis Gallopo
Most authors consider vesiculopustular palmar-plantar psoriasis (Barber type) as a variant of the course. However, some consider this disease to be independent. Etiology unknown. Clinically, there are 3 forms of this dermatosis: pustular, vesicular and erythematosquamous. The disease can begin at any age. Men get sick more often. The rashes begin on the terminal phalanges of the fingers, less often on the feet, gradually spreading to other areas of the skin of the palms and soles. In rare cases, the process can become generalized. The nail folds are sharply hyperemic, swollen, and infiltrated. Pus comes out from under them. Subsequently, pustules or vesicles appear on the skin of the entire surface of the nail phalanx, and gradually the cavity elements can dry out and become covered with crusty scales. The fingers are deformed, the terminal phalanges are sharply increased in size. The fingers are in a half-bent state.
The histological picture is identical to that of pustular psoriasis. Subcorneal pustules of Kogoi are sterile. The differential sign is the occurrence of skin atrophy after the lesions resolve.
Pustular bacterid of palms and soles of Andrews
, according to most authors, is an independent chronic skin disease caused by the presence of a focal infection in the body and the development of an allergy to it. The process begins in the center of the palms and soles, gradually spreading to the lateral surfaces. The first rash may be monolateral, gradually becoming symmetrical. Synchronicity of remissions and exacerbations of the disease in all foci is characteristic. The primary lesions are vesicles and pustules. Often, pinpoint hemorrhagic spots are clearly visible between the pustules. Characterized by intense itching and painful lesions. As the process subsides, the lesions become covered with dense scales.
Histologically, deep pustules containing polynuclear leukocytes and degenerated epithelial cells are found in the epidermis. Outside the pustules, there is no inflammatory infiltrate.
Sanitation of foci of chronic infection, as a rule, leads to regression of the bacterid.
Psoriasiform syphilide of the palms and soles.
It is a clinical type of secondary papular syphilide [6]. May have several options:
a) lenticular - flat papules the size of lentils, yellowish-red (copper) color, dense consistency, peeling begins from the center, gradually leaving a border of exfoliated stratum corneum along the edge (Biette's collar);
b) ring-shaped - papular elements are arranged in the form of rings and arcs;
c) horny - large papules and plaques, often on the arch of the feet, are covered with horny layers in the form of calluses with cracks and a peripheral zone of infiltration.
A general clinical examination of the patient, identification of other signs of secondary syphilis and the results of serodiagnosis allow a diagnosis to be made.
Keratoderma climacteric. It is more often diagnosed in women aged 45-55 years, much less often it can be observed in men aged about 60 years. The disease is a fragment of the menopausal syndrome [5] (Fig. 7).
Figure 7. Climacteric keratoderma of the soles. Clinically manifested by symmetrical diffuse or focal thickening of the stratum corneum of the skin of the palms and soles. The skin becomes dry and painful cracks appear. Patients often complain of itching. The course is undulating, with relative remissions and exacerbations. Skin symptoms are usually combined with various somatogenic and psychogenic disorders. As a rule, after the end of menopause, keratoderma regresses.
In clinically doubtful cases, a diagnostic biopsy should be performed. Histological examination of the biopsy specimen reveals hyperkeratosis and slight parakeratosis. Acanthosis, microabscesses and Kogoi pustules are absent. In the dermis, an infiltrate of lymphocytes, moderate expansion of capillaries, and degeneration of collagen and elastic fibers are noted.
Principles of treatment for palmoplantar psoriasis
The selection of the most effective and safe therapy for a patient with palmoplantar forms of psoriasis depends on many factors, which can be divided into objective and subjective.
Objective factors include the clinical form of plantar psoriasis, its severity, prevalence, and somatic status of the patient.
The doctor must also take into account subjective factors: gender, age, occupation, mental characteristics, intelligence, motivation for treatment, social circumstances.
The doctor has a choice of means and methods of systemic and external therapy for psoriasis. Unfortunately, none of the methods leads to a radical cure of the patient, since the methods correct individual fragments of the pathogenesis of psoriasis. Causative therapy has not currently been developed.
Traditionally, treatment for psoriasis begins with non-suppressive drug therapy (hyposensitizing and detoxifying agents).
Systemic therapy
psoriasis includes
drug therapy
in various combinations and regimens (glucocorticosteroid drugs - GCS, cyclosporine A, methotrexate, systemic retinoids, vitamin D3, anti-cytokine therapy). Unfortunately, these drugs give only a temporary positive result, they also give a large number of severe side effects and, accordingly, have many contraindications. In addition, many drugs from the listed groups have a high cost.
Photochemotherapy is used in systemic therapy
: Re-PUVA therapy (Retinoids + PUVA) and PUVA therapy (systemic and local). Phototherapy (UVB, natural insolation) is widely used. Photochemotherapy and even conventional insolation have a number of contraindications and side effects [3].
Due to the fact that palmoplantar psoriasis is most often a limited form of the disease and occurs during menopause in patients with somatic diseases, it is advisable to choose effective but non-toxic external therapy
. In our experience, the most pronounced therapeutic effect is obtained by the combined external use of topical corticosteroids and resolving agents.
According to European classifications, there are 7 classes of topical corticosteroids (see table)
depending on their anti-inflammatory activity (class 1 - drugs of maximum potency, class 7 - drugs of minimal potency). The severity of possible local side effects depends on the strength of the drug [7].
The physiological characteristics of the skin of the palmoplantar zone, primarily the thickness of the stratum corneum, allow the use of topical corticosteroids of medium and strong strength. The drug of choice may be mometasone furoate 0.1% ointment ( elokom
), mometasone furoate 0.1% with salicylic acid 5% (
elokom-S
), as well as Elokom cream. The priority in choosing these agents is explained by their high therapeutic activity combined with safety (low resorption coefficient). The treatment regimen is determined by the clinical form of palmoplantar psoriasis.
So, with the typical and horny form of the lesion
, especially in the presence of cracks, it is advisable to start therapy with indifferent fattening ointments in combination with warm baths.
Within 2-3 days, the cracks heal and the stratum corneum softens. Elokom
or
Elokom-S
ointment is applied once a day . The latter remedy is preferable, since the salicylic acid contained in the ointment acts as a weak keratolytic, clearing the surface of the plaques from horny deposits, and promotes the absorption of the ointment. Such therapy should be carried out for 10-15 days. If the patient's lesions have a pronounced infiltrate, time-tested resolving agents in the form of tar should be added to external therapy. In our country, wood tar (birch or pine) is traditionally used for these purposes; abroad, compositions with coal tar are used. The latter is considered more active, but has more pronounced carcinogenic properties.
Wood tar contains phenol, toluene, xylene, and resins. Tar preparations have an antimitotic, keratoplastic, anti-inflammatory, disinfectant effect, and in high concentrations and in pure form - a local irritant effect. It should be remembered that tar is a photosensitizer, i.e. increases skin sensitivity to ultraviolet rays.
However, the sharp specific odor and dark color limit the use of tar in dermatological practice. It should not be prescribed on the face, in the area of folds, as well as in the progressive stage of psoriasis, progressive erythroderma, pustular psoriasis, severe forms of acne, and kidney pathology.
When treating the typical and horny form of palmoplantar psoriasis in the stationary stage, it is advisable to alternate every other day with applications of pure tar for 15 minutes (placing the limb in a warm bath and then rinsing it off) and the next day with Elokom
or
elocom-S
. Usually the rash resolves after 2 weeks. In the future, the patient is recommended to use external indifferent obesity therapy for another 2-3 weeks.
In the treatment of vesiculopustular form
For palmoplantar psoriasis, we recommend prescribing only topical corticosteroids in the form of
Elokom
(in the progressive stage).
In the stationary stage, it is permissible to use ointment forms with potent corticosteroids ( elokom
). The choice of these drugs is due to their high efficiency and minimal resorption from the skin surface. Courses of therapy for a month do not lead to skin atrophy.
This external treatment regimen for palmoplantar psoriasis is available for self-treatment of the patient at home, effectively resolves the rash in 20-25 days, and can be repeated several times a year. We recommend it to patients in whom it is undesirable (due to various factors) to use active general therapy.
Complex therapy of palmoplantar psoriasis using Losterin cream
Dermatologists often prescribe classic cream or foot cream “Losterin” in complex therapy of the active stage of palmoplantar psoriasis, as well as to maintain the disease in remission. However, it can be freely purchased at a pharmacy or online. This is a local non-hormonal remedy. It does not contain aggressive and harmful components, as well as dyes and flavors. Therefore, “Losterin” is absolutely safe.
All products from the Losterin line have been tested in laboratories and confirmed their effectiveness. Doctors often recommend them due to the following advantages:
- ease of use (the drug can be used at home and while traveling without any problems).
- lack of addictive effect (the product can be used every day and for several courses);
- no side effects - the cream is well tolerated and does not cause allergic reactions
- complex effect on the symptoms of the disease - the drug reduces peeling on the surface of rashes, effectively copes with skin redness
- harmless composition;
Losterin gently fights inflammation and eliminates external symptoms.
How to treat psoriasis in a child?
A step-by-step therapeutic approach is recommended, based on the use of:
- local drugs;
- phototherapy;
- systemic therapy.
⠀
It is worth noting that most children have a mild form of the disease, which can be successfully treated with medications for external use.
⠀
- Treatment of psoriasis in persons under 18 years of age begins with the use of local hormonal agents of weak or moderate activity. Local therapy is used for limited manifestations or as an adjunct to phototherapy and systemic treatment for more severe, widespread processes. The consumption of the steroid drug should be dosed at the rate of “fingertip unit” and correspond to a strip squeezed out of the tube onto the terminal phalanx of the index finger of the hand. This dose is applied to a child's skin surface area equal to the area of two adult palms. It is worth noting that hormonal external agents are not recommended for babies in their first year of life to apply to the skin of the face, neck, and natural folds.
- The use of drugs based on calcipotriol. Children over 6 years of age are prescribed in combination with topical steroids.
- Preparations with zinc pyrithione are often prescribed for psoriasis on the scalp of a child and in the regressing stage of plaques on smooth skin. There are several dosage forms that are convenient to administer to children, such as aerosol or shampoo form.
- Topical calcineurin inhibitors are preferably applied to the skin of the face, neck, natural folds, i.e. in areas where the application of steroids is not recommended.
- Also, in cases of excessive peeling, products with salicylic acid are prescribed, because it has a good keratolytic effect. Sometimes products based on naftalan oil, ichthyol, and birch tar are used for treatment.
Prevention of palmoplantar psoriasis
Many of the signs of psoriasis on the palms are also common on the feet and soles. Therefore, therapy and prevention are similar.
Basic preventive measures:
- Take daily baths with the addition of natural esters, sea salt or mild baby soap without any additives. Instead of baths, you can do 20-minute baths for your feet and hands.
- Use of moisturizers. Especially after a shower or bath. The product is applied once a day. In advanced cases - twice a day.
- Use soft towels. In this case, the skin is not rubbed, but “blotted” by carefully applying a towel to it.
- Walks in the open air. It is important for people with psoriasis to get enough sunlight. However, moderation is important here. Too much sun will only make the situation worse. Therefore, it is worth consulting a doctor about this issue.
- Rejection of bad habits. Cigarettes, alcohol and lack of daily routine.
- Protection against infections. It is important to monitor your immunity and not have contact with sick people.
- No stress. Or working on changing the perception of negative situations.
These rules must be followed throughout your life. Then the manifestations of the disease will be minimal, and the periods of remission will be longer.
Cost of treatment
Initial appointment with a dermatologist (assessment of patient complaints, history taking, examination, preliminary diagnosis, consultation)
Primary appointment – visiting a doctor of a specific specialty for the first time. Make an appointment
1510 ₽ 2160 ₽
Repeated appointment with a dermatologist
Make an appointment
800 ₽
Treatment of mild psoriasis for 7 days (7 Dermalight procedures or 7 injections with our drugs + ointment from our components)
Make an appointment
4000 ₽
Treatment of moderate psoriasis for 7 days (3-6 droppers; 4 injections with our drugs; ointment from our components; 4 Dermalight procedures)
Make an appointment
5500 ₽
Treatment of severe psoriasis for 7 days (6-7 droppers or 12 injections with our drugs; ointment from our components; 4-6 Dermalight procedures)
Make an appointment
8000 ₽
Note: Most often, treatment of any grade requires a minimum of 4 weeks of treatment.