Bedsores on the heels of black color occur in bedridden patients not only at home, but also in the hospital and represent dead areas of the heel skin. The development of bedsores occurs with prolonged compression of soft tissues and skin between the heel bone and the surface of the bed. Most often, black bedsores on the heels occur in patients with prolonged immobility, especially against the background of circulatory problems. Trophic heel ulcers are treatable, but some never heal completely. Bedsores are easier to prevent than to cure. The degree of skin and tissue damage ranges from redness of the skin to a deep necrotic wound involving the bone. Many patients and their relatives try to treat pressure sores on their heels at home. This approach can be successful in the early stages of the disease, but when the process develops deep into the heel bone, it becomes impossible to cure such a bedsore without complex reconstructive plastic surgery.
Stages and symptoms
Bedsores can develop quickly, but the formation of bedsores and ulcers occurs through four stages (each of which has its own symptoms):
- Stage 1
Redness of intact skin. It is slightly inflamed and may be painful, itchy and warm to the touch. You may also notice that the texture of your skin has changed slightly. At this stage, bedsores on the heels resemble a sunburn. This initial stage is difficult to detect in people with dark skin.
- Stage 2
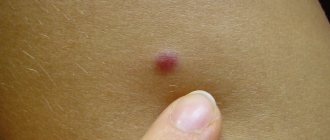
In the second stage, the first signs of skin damage appear. They look like abrasions, blisters or small pits. The outer layer of skin is broken, red and painful. The surrounding tissue may be pale, red, and swollen. The upper layers of tissue, as the most damaged ones, begin to die and peel off. Bruising at this stage indicates suspicion of possible deeper tissue damage, involving fat or muscle tissue.
- Stage 3
Complete loss of tissue. The damage extends to the deeper layers of tissue in the heel. Crater ulcers are present and are susceptible to infection. Subcutaneous fat may be visible, but no bones, tendons or muscles are affected. The depth of a stage 3 ulcer depends on its anatomical location. Most often, bedsores on the heels progress to stage 3, until others notice them and begin to treat them.
- Stage 4
Loss of tissue, opening of bone and tendons. Ulcers with black edges spread to the heel bone and can lead to the development of osteomyelitis (a purulent-necrotic process in the bone). The exposed calcaneus is visible or directly palpable at the bottom of the trophic ulcer. These ulcers are extremely difficult to treat and may require many months and activities to heal. Therefore, preventing the development of ulcers should be taken more seriously.
Treatment
Particular attention should be paid to careful treatment of lesions.
The patient should take daily warm foot baths with potassium permanganate. In this case, it is necessary to remove the crusts, open the blisters, cut off the fringe along the edges of the erosions, as well as the covers of the festering blisters. After the bath, wet-dry bandages or lotions are applied with an aqueous solution of copper (0.1%) and zinc sulfates (0.4%) or with a 1% aqueous solution of resorcinol. After the weeping stops, dermozolon, mycozolon are used, and then alcohol fungicidal solutions, Castellani paint, and finally, if necessary, fungicidal pastes and ointments.
The effectiveness of treatment depends not so much on the choice of pharmacological drug, but on their correct, consistent use in accordance with the nature of the inflammatory reaction.
Fungicidal treatment is carried out until the fungal test results are negative.
Anti-relapse treatment carried out within a month after the elimination of lesions is extremely important - wiping the skin of the feet with 2% salicylic or 1% thymol alcohol and dusting with 10% boron powder. For the same purpose, it is necessary to thoroughly wipe the inner surface of the shoes with a solution of formaldehyde, wrap them in an airtight fabric for 2 days, then ventilate and dry them, and socks and stockings for 10 minutes. boil.
When athlete's foot is complicated by pyococcal infection, antibiotics are prescribed - methicillin, cephaloridine, oleandomycin, metacycline, erythromycin. The patient must remain in bed.
Complications
Complications of bedsores (especially pressure ulcers) can be life-threatening and include:
- Phlegmon
Acute purulent inflammation of the skin and soft tissues. People with nerve damage (neuropathy) or a spinal injury often feel no pain in the area affected by inflammation and pressure sores. Cellulitis can cause severe intoxication and even general blood poisoning (sepsis).
- Heel ulcer
A chronic heel wound that does not heal for a long time significantly worsens the patient’s quality of life, as it leads to impaired support and walking function. A trophic heel ulcer can occur as a result of a bedsore, not only in spinal patients, but also in postoperative and post-resuscitation patients due to their prolonged immobilization.
- Damage to bones and joints
Infection from an ulcer can affect joints and bones. Infection in the joint cavity can cause general blood poisoning. Bone infections (osteomyelitis) can lead to destruction of the heel bone.
- Cancer
Wounds that do not heal over time can eventually develop into squamous cell skin cancer.
- Sepsis
General blood poisoning develops with weakened immunity, diabetes mellitus and other severe concomitant diseases and often causes death.
Blood clot in the legs: the most common symptoms
15.10.2019
The formation of a blood clot in the deep veins of the lower extremities is a dangerous disease, as there is a risk of life-threatening complications. The thrombus can break away from the vascular wall, and the venous system reaches the heart and pulmonary artery - a pulmonary embolism occurs. When the pulmonary artery is completely blocked by a blood clot , sudden death occurs.
An increased risk deep vein thrombosis occurs in smokers, pregnant women, the elderly, patients with obesity , tumors, and blood .
What are the risk factors for developing a blood clot?
Factors contributing to the formation of a blood clot:
- dehydration;
- prolonged immobilization, such as air travel;
- presence of varicose veins ;
- pregnancy ; injuries, operations ;
- blood disorders ;
- medicines - contraceptives;
- obesity.
There are three main mechanisms for the formation of blood clots:
- damage to the wall of a blood vessel . If there is damage to the vascular wall (rupture, trauma, tingling), adrenaline, norepinephrine and serotonin are released, causing vasospasm . Platelets, and then white and red blood cells cling to the lesion - a blood clot ;
- venous sagging - delayed blood flow and congestion in large vessels favor thrombosis ;
- increased blood - Increased blood occurs during injuries, surgeries, tumors, burns, and dehydration.
What are the symptoms of a thrombus (blood clot) in the veins of the lower extremities?
At an early stage, when the blood clot is small and does not completely block the lumen of the affected vein , there is no inflammation and symptoms may be absent.
Here are some classic symptoms you may experience with a blood clot in your legs:
- spontaneous pain. In some cases there may be little pain, such as heaviness or discomfort, and in other cases there may be quite a lot of pain. In an upright position, the pain intensifies;
- painful pain in the course of large vessels ;
- pain in the groin of large vessels occurs in the area of the inguinal fold, in the buttock, inside the thigh;
- provoked pain. Pain occurs in the following cases: in the dorsiflexion of the foot pain is provoked, in the lower part of the leg - due to the release of the tibial veins ; coughing and sneezing cause pain in the corresponding limb;
- swelling. Painful swelling in the area of the clot - ankle, lower leg . It is typical for the swelling to not go away with cold compresses and may be enlarged for no apparent reason;
- change in skin color. The skin turns red and then turns blue-gray. The appearance of red spots on the skin in the area of the clot is a characteristic sign of the formation of a blood clot in the deep veins . These spots do not disappear over time, but become larger;
- warming of the skin. Increased skin temperature in the area of the blood clot is a relatively early sign. Warm skin may be accompanied by other symptoms such as itching, throbbing;
- dilated superficial veins - dilated veins around the ankle, lower leg, at the base of the thigh dilate;
- general symptoms are increased heart rate, fever, dizziness , anxiety.
Published in Phlebology Premium Clinic
Prevention and prognosis
Movement constantly redistributes pressure on our body. When illness or injury limits our mobility, pressure builds up in certain areas of the body and blood circulation decreases. This can lead to the death of skin and tissue, creating pressure sores and ulcers. To reduce the risk, it is necessary to use anti-bedsore systems and devices that relieve pressure on bone protrusions.
Healing of the wound on the heel is delayed due to the immobile position of the patient, poor trophism due to vascular lesions and the general condition of the body. Improper wound care and various folk recipes negatively affect the patient’s condition. A bedsore is complicated by damage to the surrounding soft tissue, infection and purulent discharge. A long-term purulent-destructive process leads to a deterioration in the general condition and impaired absorption of nutrients. Without proper care, a patient develops new bedsores in other parts of the body, which aggravate the pathological process.
However, simple treatments can help prevent these painful and dangerous problems.
- Take care of your skin:
Examine the patient's skin several times a day. Pay special attention to the heel areas and other pressure points on the body. Minimize contact of moisture with the body. Keep skin clean and dry. Wash it with a mild cleanser, care oil and wipe dry. Perform hygiene procedures and wash with soap as quickly as possible to limit skin exposure to moisture, urine and feces. Change bedding and clothing promptly. Make sure that there are no wrinkles in the bed linen and clothes under the patient.
- Protect your skin from injury:
Avoid massaging the affected areas of soft tissue over bony prominences. Change your body position at least every 2 hours. Reduce friction. If the patient is bedridden, the head of the bed should be raised as little as possible. When it rises above 30 degrees, a person can slide across the surface of the bed, damaging tissue and small blood vessels.
Pillows and special pads should be used to avoid contact between the knees and ankles when turning the patient on his side. If the patient is completely immobile, pillows should be placed under the feet from mid-calf to ankle to relieve pressure on the heels. Never place pillows under your knees. This impairs blood circulation.
- Eat well:
A balanced diet is very important for healthy skin at all stages of treatment. Healthy tissue is less susceptible to damage. In cases of scuffs and abrasions, treat the defects with antiseptic preparations.
- Improve patients' ability to move:
A rehabilitation program can help some people get back into shape quickly.
- Shift your weight and change positions frequently:
If you use a wheelchair, try shifting your weight every 15 minutes or so. Get up if possible. If you have enough strength in your arms, do a push-up—lifting your body off the seat, resting on the armrests of the chair. Bedridden patients may experience discomfort, pain, social isolation or depression. Try to find something to do that suits your physical capabilities.
Attempts to treat bedsores at home with folk remedies often lead to the opposite effect. Do not try to cope with the problem without specialists - you can lead the situation to a hopeless dead end.
Common Causes
The most basic disorders that cause dark spots to appear in the heel area are bedsores, hemorrhages, and warts. In the first case, this phenomenon is due to the fact that a person remains in a lying position for a long period of time.
There are several types of bedsores. The area of the heel that is subjected to pressure begins to thicken, turn red, and then darken. The deep layers of the epidermis may be affected, which leads to impaired circulation and the formation of tissue necrosis. Sometimes erosions form in the heel area, which also causes darkening of some areas. With bedsores, there is often tingling and numbness in the affected area. Also, the skin may partially or completely lose its sensitivity.
Hemorrhages are associated with systematic compression of the foot. This mainly happens due to wearing narrow, uncomfortable shoes, especially if a person plays sports in them or simply leads an active lifestyle. In this case, blood vessels rupture, which leads to bruising. After which black spots appear on the heels. This phenomenon is often encountered by people who are very overweight. There is an increased load on the feet, and the heel is constantly under pressure.
Bruising can be recognized by the following signs:
- the spots are black or dark brown in color;
- the lesion is smooth;
- the skin structure does not change;
- When palpated, such areas do not hurt.
Warts can also cause spotty darkening of the heel area. This growth can be recognized by its protruding shape and size of about one centimeter. The shape of the wart is round, its surface is smooth at first, and then over time it becomes covered with roughness. The skin on this area of the heel first has a pinkish tint, and then turns brown.
Treatment at the Innovative Vascular Center
Doctors at the Innovative Vascular Center, treating severe vascular patients with many concomitant diseases, know firsthand about the problem of pressure sores on the heels. Often patients already come to us with such pressure ulcers, sometimes they develop during long-term vascular diseases. The complexity and danger of this problem prompted our surgeons to develop methods for the prevention and effective treatment of bedsores, cleansing the affected tissues in a sick person, because the appearance of bedsores leads to a change in the course of the underlying disease for the worse. We are able to close any pressure ulcers using reconstructive plastic surgery methods.
Why are black spots on legs dangerous?
There is reason to worry about painful mini-hematomas if they do not go away for a long time and new ones constantly form. This may indicate problems with the blood's ability to clot and requires an urgent visit to the doctor.
Bedsores are a dangerous phenomenon because:
- their consequences may be irreversible;
- the last stages of the disorder cannot be treated and require surgical intervention.
Diagnostic measures
Only a dermatologist can determine the causes of the problem. To clarify the suspicion of HPV, the doctor will scrape the dermis.
For diagnosis, a visual examination is carried out by a specialist. To confirm HPV, an analysis of certain DNA fragments in biological material is prescribed. You will also need to undergo an ultrasound examination to determine the depth of the root.
To diagnose a hemorrhage or developing pressure ulcer, an examination and an oral conversation with the patient are sufficient.