What complications are there?
- A tumor in the neck area can cause compression of the larynx and trachea, and also lead to obstruction of the upper respiratory tract.
- A tumor on the eyelid can be complicated by vision problems.
- A hemangioma in the liver or spleen can lead to bleeding.
- Hemangiomas located on the nose, ears, lips, hands can become covered with ulcers. Moreover, if an infection gets into the wounds, the inflammatory process can affect the deep layers of tissue or the corresponding organ.
- A hemangioma located on the leg can cause gait disturbances.
- The tumor can give rise to the development of Kasebach-Merritt syndrome. This is a rare disease in which hemangioma is combined with thrombocytopenia and bleeding disorders, which leads to frequent bleeding and heart failure.
- If the hemangioma affects the vertebrae and pelvic bones, disorders of the musculoskeletal system may occur.
Hemangiomas in children
My one-and-a-half-year-old patient had a bruise under his eye.
- Where is he like that? Fell? - I asked. Unfortunately, being a pediatrician involves a certain amount of suspicion. “It’s not a bruise, he didn’t fall,” my mother answered tiredly. -Have you forgotten again? He has had this since birth, a hemangioma. I was confused. I had seen the boy once or twice before and, to be honest, had already forgotten about his peculiarity.
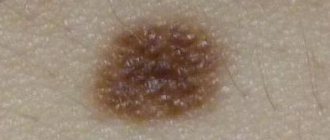
Taking a closer look, I was convinced that it was really not a bruise. A slightly convex, nodular formation clearly protruded above the surface of the skin. Its edges were uneven and seemed to consist of several small islands.
Infantile hemangiomas are benign vascular tumors growing from the endothelium. Hemangiomas come in various sizes - from millimeter to huge segmental ones, covering almost half of the head. The color of hemangiomas is usually red or bluish. Most often they occur on the head and neck, but can be on any part of the skin, mucous membranes and even on internal organs. Differential diagnosis must be made with other vascular formations.
There are single and multiple hemangiomas. Superficial, deep and combined hemangiomas are also distinguished.
How can the disease be diagnosed?
The capillary form in the vast majority of cases is diagnosed based on history and examination. The pediatric surgeon finds out when the tumor was first noticed, whether it has changed in shape, color and size, and whether there are signs of regression.
If this data is not enough and there are doubts about making a diagnosis, the specialist prescribes additional studies:
- ultrasonography;
- Dopplerography;
- computed tomography with contrast;
- magnetic resonance imaging;
- biopsy of the tumor site
- And so on.
Archives
Short Wiklad
Metry DW Postgrad Med 2003; 114(1)
Hemangiomas, the most common swellings in neonates, are the good swellings of the vessel endothelium. Stinks are found in about 10% of the wild population of the United States. Hemangiomas occur 4 times less often in girls, less in boys, and also significantly more often in white cats. Complicated hemangiomas often develop into girls, the reasons for which are unclear. The growing population is another factor in the rizik, and the rizik is directly proportional to the vase with the nation. Although most hemangiomas occur sporadically, they still report episodes of decline of the autonomous-dominant type.
A minority of hemangiomas appear during pregnancy, but become visible during the first months of life. Early outbreaks may be so weakly expressed that they are not recognized and are often regarded as rags or blues. Sometimes hemangiomas may appear as bright-red flat patches with the appearance of “wine” spots. Most hemangiomas vary in size from several millimeters to several centimeters in diameter, but they can be superficial, deep, or combined (folded hemangiomas) (Fig. 1). The superficial form is the most common and has the appearance of bright purple papules, nodules or spots that protrude above the normal skin. At the same time, the deep hemangioma of the backbone presents a bulging nodule in the color of meat, which often bears a dark tint or an excessively telangiectatic area. Although hemangiomas are often found on the head and neck, they can also be found in other parts of the skin, mucous membranes and internal organs.
Rice. 1.
A folded hemangioma of the scalp, which consumes the superficial and deep components.
As a result, hemangiomas undergo a growth phase (proliferative), which lasts on average 6-12 months. After this, a period of complete spontaneous reversal development (involution) occurs, which lasts on average 2-10 years. Complete involution occurs with an average frequency of 10% per river. Also, approximately 50% of hemangiomas are known before the age of 5 years, 70% - before the age of 7 years, and 90% - before the age of 9 years. The first clinical sign of the involution of the superficial hemangiomas is a change in color from bright-red to dark-red or gray, which begins in the center with instant softening and consolidation of the fluff. Deep puffs become less dark and colder.
The frequency and breadth of hemangiomas involution even increases among children, which is important to predict. It is especially important to recognize in many cases that the involution will end with a normal-looking skin. Approximately half of children with hemangiomas will have excessive changes in the appearance of scarring, atrophy, excessive skin thickness, changes in skin color, and telangiectasia. The risk of scarring is greatest in large, nodular, and superficial hemangiomas, especially with the appearance of sharp, shaved edges (Fig. 2). Hemangiomas in the visible areas of the lips, nose (Fig. 3) or ear canal are especially susceptible to complications. So, hemangiomas on the legs (hemangiomas that arise from a small base) may be a risk of excess fibrous-fatty tissue, which often requires surgical removal. Therefore, when assessing such conditions, the doctor is obliged to truthfully inform the fathers about the world’s inheritance.
Rice. 2.
Verkhneva, Vuzlova hemangioma with scarring.
Rice. 3.
Hemangioma of the tip of the nose with a risk of deterioration of the nasal cartilage and excess fibrous-fatty tissue.
Classification of hemangiomas and their complexity
Nina explained that the morphology of hemangiomas provides important information about potential complications. Apparently, prior to the modern systemic classification, most hemangiomas can be classified morphologically into localization, segmentation or multiplication.
Localized hemangiomas, which become important in the majority of such lesions, are characterized by a rotting, puffy growth that gives rise to a clear spatial structure; Apparently, it does not resemble a single cavity and does not provide clear evidence of a linear or geometric structure (Fig. 2). In view of this, it is clear that less wide segmental hemangiomas are more important, they are flat-like and demonstrate a linear and/or geographical structure along the entire length of the skin (Fig. 4, 5, 6, 7 and 8). Based on localized hemangiomas, segmental lesions are more likely to occur in Hispanic families and children with larger body weights and women with a larger gestational age. Moreover, segmental hemangiomas are often associated with complications such as rupture, developmental anomalies and concomitant hemangiomas of internal organs. The stinks will require intense and prolonged treatment, and may also result in a worse result.
Rice. 4.
Segmental cervicofacial hemangioma with the risk of one-hour discharge of dichotomies.
Rice. 5.
Segmental hemangioma with damaged vision.
Rice. 6.
Lumbosacral hemangioma in the absence of damage to the spinal cord. Return attention to the care of the intersecting furrow in the upper part.
Rice. 7.
Multiple small hemangiomas, characteristic of neonatal hemangiomatosis.
Rice. 8.
A large, flat-like hemangioma is presenting with erythema of the nose and upper lip in the absence of speech with PHACE(S) syndrome.
Virazkuvannya
Virus removal is the most common type of hemangiomas. It is important to open up the large segmental areas of the lips, between the spaces and folds (Fig. 9). Scarring, secondary infection, bleeding and pain may also occur. The reasons for the development of the virus are unknown, due to associated factors - typical localization, maceration and rubbing.
Rice. 9.
A large, flat-like hemangioma is presenting with erythema of the nose and upper lip in the absence of speech with PHACE(S) syndrome.
Association anomalies
The development of hemangiomas on the cervicofacial, periorbital division and middle lumbosacral division, especially if the morphology of the lesion is segmental, may be associated with accessory folds. The cervicofacial localization is clearly associated with one-hour urinary tract infections, and approximately 40% of urinary tract infections in children will likely require tracheotomy. The risk of direct connections from the widening of the scalp hemangiomas to the zone of innervation of the third gullet of the trifrequent nerve (the “beard area”), which includes the skin of the anterior area, the chin, the anterior surface of the neck and/or the lower yu lip (Fig. 4). In children, symptoms most often develop between 6 and 12 months of age, as they tend to progress; Inspiratory and/or expiratory stridor is observed. Cough, cyanosis and hoarseness of voice are also often present. The occurrence of discrepancies can be confirmed by endoscopic examination.
It is well known that hemangioma of periorbital localization can disrupt the normal development of the organ of the eye. Most hemangiomas result in destruction of the vision of the upper medial part of the canopy, which is the part that best accommodates the closed canopy (Fig. 5). Prote hemangioma of any size, morphology or other periorbital localization can cause blurred vision. Astigmatism, most often complicated, is also embossed on the cornea of the swelling as it grows. Other common problems include ptosis, proptosis and strabismus. Blindness, caused by the absence of visual stimuli, is a result of mechanical obstruction of the visual field and is one of the most common causes of blindness in children, which can be avoided.
The most important thing is that it is immediately handed over, the remaining damage to the eyes appears in a short hour (either 2 hours or less) and becomes irrevocable. Liquation can be simple (for example, gluing up an unaffected eye to secure the recovery of an eye that is partially closed by a hemangioma), but it can be irrigated and aggressive. The child may be examined by an ophthalmologist for the treatment of perorbital hemangiomas and their potential complications.
Hemangiomas, localized over the lumbosacral lobes of the spinal cord, may be associated with spinal disc gaps or other congenital anomalies. Segmental expressions that extend along the midline and may be flat or telangiectatic in nature are the biggest problem. Another important diagnostic sign of a chronic cleft ridge is the development of the interstitial groove at the upper part (Fig. 6). They also inform about such concomitant anomalies of development, such as fixation of the spinal cord, occlusion of the anus with a closed nora, cystic anomalies of the cystic cyst, anomalies of the arterial organs, and any lipomyelomenigocele. .
Because of this complexity of fixations, the spinal cord is potentially the most destructive for the child. Symptoms, which may not appear until age 3 or more, include paresis of the legs, atrophy of the ulcers, non-tearing of stool and ulceration of the plantar surface of the toes. Early detection and surgical correction of oblique ulcers may result in permanent neurological damage. For residual diagnostics, the most sensitive is nuclear magnetic resonance imaging.
| Signs of PHACE(S) syndrome P - malformation of the posterior cranial fossa (Posterior fossa), most often with the Dandy-Walker variant H - hemangioma (especially large, segmental manifestations) A - anomalies of arteries C - cardiac anomalies and coarctation of the aorta E - anomalies of the eyes (Eye) S - cleft of the sternum (Sternum) and/or supraumbilical suture |
In rare cases, hemangiomas may be associated with two congenital syndromes: PHACE(S) syndrome and diffuse neonatal hemangiomatosis. PHACE(S) syndrome is diagnosed when there is a large segmental hemangiomas associated with multiple concomitant congenital malformations, most often structural or cerebral anomalies. The syndrome represents a spectrum of many illnesses, in some cases all potential components cannot be manifested. The key feature of PHACE(S) syndrome is the presence of large, segmental hemangiomas, especially superficial ones, which can affect one to many dermatomes (Fig. 8). The first manifestation is often mildly interpreted as a “convex” nevus (“wine” plaque), associated with Sturge-Weber syndrome. The result of “inflammation” of the nevus is to develop into a vascular malformation, which is lost over a stable period of time, and develops into a hemangiomy - a dynamic formation, which has a phase of growth and a phase of involution.
Children with rhizomes with PHACE(S) syndrome require additional neurological treatment and also require radiological treatment of the brain. Ultrasonic cerebral sterilization can be used as a screening test in animals with unbroken thymus. The posterior cranial fossa is best visualized with MRI, and cerebral vascularization is most clearly visible with nuclear magnetic resonance angiography. To exclude coarctation of the aorta and structural abnormalities of the heart, it is recommended to tighten the heart and tighten the arterial pressure at all ends. If any of the already described components of the syndrome are detected, a consultation with a pediatric ophthalmologist is indicated. And finally, with widened hemangiomas on the face of children, it is necessary to carefully monitor for signs of impairment of the ductal passages for adequate assistance.
Neonatal hemangiomatosis (the presence of multiple hemangiomas) is most often benign illness, which is associated with skin lesions. Proteus may also develop a rare and dangerous illness due to diffuse (or dissemination) neonatal hemangiomatosis. Clinically, hemangiomas, which are associated with diffuse neonatal hemangiomatosis, are small (2–20 mm in diameter) and are present in numbers to hundreds (Fig. 7). Of the internal organs, the liver is most often affected, then the scolio-intestinal canal, cerebrum and leg. Hepatic hemangiomas, most likely, undergo involution in the same way as cutaneous hemangiomas, and potentially serious complications may appear during the proliferative phase. Most people with severe liver damage manifest a triad (hepatomegaly, persistent heart failure and anemia), which develops significantly during the first 3 months of life. The most common cause of death is persistent heart failure. Other potential complications resulting from the development of the urinary organs include intestinal hemorrhage, mechanical swelling and stress of the central nervous system due to the presence of volumetric rupture.
There are still a large number of hemangiomas that are needed for further investigation for diffuse neonatal hemangiomatosis. The fragments of 10-15% are unaffected by hemangiomas and there are two hemangiomas, so the fastening of such children is probably not necessary for normal signs of physical fastening. Currently, 83% of patients with diffuse neonatal hemangiomatosis may have 5 or more hemangiomas. Therefore, it is necessary to monitor the patient for less than 6 months with multiple scalp hemangiomas. Screening ultrasound of internal organs with Dopplerography is a non-invasive method for identifying liver disease, and it also helps to identify hemangioma from other vascular malformations, treat one by one or multiple hemangiomas and viconati monitoring of treatment. It appears that single segmental hemangiomas of the skin can also be associated with hemangiomatosis of internal organs. The current study describes 46 episodes, in which skin hemangiomas occurred in 36 (78%) episodes. As with diffuse neonatal hemangiomatosis, the liver is most often affected from the internal organs, then the scutulo-intestinal canal, the cerebrum and the mediastinum. PHACE(S) syndrome was also present in 18 patients (39%), in this subgroup visceral hemangiomas were most often found in the cerebrum (50%) and mediastinal hemangiomas (50%). More than a quarter of patients die due to inability to breathe, most often as a result of intestinal hemorrhage or congestive heart failure through hepatic hemangiomas.
General radiological treatment of the whole body of all patients with segmental hemangiomas is not recommended due to the high risk and need for external neurosurgery for nuclear magnetic resonance imaging in young children. In addition, it is important to remember that many posterior hemangiomas remain completely asymptomatic. However, precautions should be taken to determine the presence of other risk factors (depending on the anatomical localization of hemangiomas) and other manifestations of hemangiomas.
Likuvannya
Treatment is often necessary for large virulent hemangiomas or those that affect vital structures. Thorough local wound cleansing is the basis of wound therapy and is especially important for wounds in areas susceptible to trauma and infection, such as the perineum. Prescribe topical and oral antibiotics, barrier creams and bio-occlusive dressings. Local wound cleansing not only provides a barrier against secondary infection, but also significantly reduces pain.
It is especially important to treat virulent hemangiomas of the perineum. Fathers should only use super-fading diapers, as they need to be changed frequently to minimize exposure to dirt and feces. Barrier pastes, such as zinc oxide paste, can be applied with a thick ball and then covered with a bandage soaked in Vaseline. You can also use a hydrocoloid dressing (DuoDerm Extra Thin),
Which is especially good for the gap, it can be deprived for a few days.
It has been proven that metronidazole gel (MetroGel)
is safe and effective when applied, especially in the folds of the neck, such as the lips and crotch.
Recently published information about Becaplermin 0.01% gel (Regranex)
stagnated with hemangiomas with virulence, refractory to standard dissection.
Becaplermin, a recombinant platelet growth factor, is approved by the FDA
for the treatment of diabetic polyneuropathic diseases of the lower ends. A later author and spivrobitniki reported on a large number of additional episodes, which were successfully treated with thin-spherical applications of becaplermin for intervening hemangiomas with virulence. Bekaplermine was covered with a thick ball of barrier paste and a non-adhesive bandage as needed. Five of the eight episodes of deep infections were refractory to standard treatment and the outbreaks were silent for 3-21 days (the average one was 12 days). We consider becaplermin to be a first-line drug for hemangiomas that develop in the perineum and other areas.
Bil, associated with virulence, is often even stronger. Stressed cats often result in sleep disturbances and increased anxiety. Oral acetaminophen (with or without codeine) or local anesthetics (such as lidocaine ointment) may be necessary. To reduce the risk of ice-caine toxicity, patients should be instructed to apply only a small amount of ice-caine cream (the size of a pea) to the affected area no more than 4 times a day. EMLA
(eutectic mixture of local anesthetics) it is necessary to avoid avoiding the use of local anesthetic hydrochloride, which is associated with methemoglobinemia in neonates.
The risk increases when EMLA
is combined with other drugs that are associated with methemoglobinemia (for example, acetaminophen). Pulsed laser therapy on organic tissues alleviates and eliminates the re-epithelialization of viral hemangiomas, in order to treat the superiliacs before stagnation.
Systemic corticosteroids are deprived of first-line drugs in advanced hemangiomas, although their exact mechanism of action is not entirely clear. When the proliferative phase persists for an hour, systemic corticosteroids often inhibit the growth of hemangiomas and induce their regression. Efficiency drops to 90%. Internal tumor injections of corticosteroids may be effective for small (up to 3 cm in diameter), well-formed hemangiomas, as well as for their expansion. Inject Zagalom 3-5 injections at 6-day intervals; the cutaneous dose should not exceed 3 mg/kg. Proceed with internal tumor therapy and proceed with caution, sedation, for periocular hemangiomas. Rare and serious side effects are reported, including renal necrosis, occlusion of the central artery of the retina, and suppression of the epithelium.
Systemic corticosteroids suppress the hypothalamic-pituitary-superior function for several days per day, especially when corticosteroids are administered twice a day. Therefore, it is necessary to give priority to administering the drug once on the day of the month. The initial starting dose is 2-3 mg/kg, which is then continued for 4-8 days. Then the dose of the drug must be changed step by step over several months. Raptova treatment or changing the dose of corticosteroids, if the hemangioma is still in the active growth phase, often leads to “rebound” proliferation.
Treatment with corticosteroids in hemangiomas does not often lead to mild transient side effects, but they protect against rare side effects. Short-term effects are most likely to disappear with a course of corticosteroids for 6 months or longer and disappear with continued administration of the drug. The most common complications are the appearance of a Cushingoid appearance, which is important during the first 1-2 months of treatment. Changes in personality (for example, depressed mood, restlessness, sleeplessness, restlessness) occur in about a third of the time, as naturally, during the first 2 years of recuperation. As a result of the temporary suppression of collagen synthesis, skeletal growth is inhibited, which can clearly be affected since childhood growth is most rapid during the first years of life. In the future, all children achieve normal growth indicators immediately after stopping the bath, as a matter of fact, up to 2 years of life. Pulmonary disorders occur in approximately 20% of children and can be relieved by taking H2 blockers such as ranitidine hydrochloride.
Corticosteroids also suppress the immune system by inhibiting the migration of neutrophils to the site of inflammation. Live viral vaccines cannot be administered unless corticosteroids are removed at doses that exceed physiological ones. Patients should avoid contact with people with chickenpox; it is important not to administer vaccine against chickenpox to children under the age of 1. Serious complications of corticosteroid therapy (aseptic necrosis of the head of the femoral cyst, hypertension, osteoporosis and cataracts) are extremely rare in children.
Interferon alfa, prescribed at an initial dose of 3 million OD/m2/day, is often an effective alternative for children with life-threatening hemangiomas who do not respond to corticosteroids. The use of interferon in children is supported by reports of neurotoxicity in the form of spastic diplegia. This disabling side effect is clinically similar to cerebral palsy and may be permanent in some children who do not respond to the drug. I want 2a-form interferon alpha (Roferon-A)
The kidney was considered to be the cause of the development of spastic diplegia, and similar toxicity was also reported when treated with the 2b-form
(Intron A)
. The risk of spastic diplegia may affect as many as 20% of medical patients, but it is likely due to the dose and severity of treatment, although the cause of this toxic side effect is unknown. It is necessary to carefully watch out from the neurological point of view during the treatment with interferon.
If hemangioma becomes a major cosmetic problem, treatment tactics must be tailored individually. Oral and internal corticosteroid creams can be treated with laser or surgical treatment. Pulsed laser on organic parts is an effective method for light-colored superficial hemangiomas, but it is not possible to detect, but it is effective for deep hemangiomas, the depth of laser penetration is less than 1.2 mm. The most pleasant treatment for laser treatment of hemangiomas is the treatment of post-involutional erythema and/or telangiectasia. In addition to the treatment of “wine” spots, the application of a pulsed laser on organic semi-spots for hemangiomas in early childhood is super sensitive to the problems of hypopigmentation, changes in skin texture and smoothness Viral treatment and/or scar treatment. For smaller hemangiomas with a risk of scarring, especially hemangiomas on the lower part of the patient, the patient should be carefully treated for an early consultation with a plastic surgeon. It is necessary to carefully consider the benefits and risks of surgical intervention, as the fragments of the post-operative scar may be aggravated, as a result of spontaneous involution.
Active non-delivery is deprived of the basis of jubilant tactics in the majority of uncontrollable episodes, as spontaneous involution occurs again. The solution to the doctor’s decision cannot be treated surgically or medicinally, but rather through passive tactics. Psychological complications of hemangiomas, especially when severely exposed, require special respect. Fathers often become the subjects of inappropriate comments on the side, which include the abuse of the child. Unspeakable children can fight if they smell their father’s anxiety, fear or depression. For effective treatment of hemangiomas, emotional support and encouragement, medical and psychological aspects of care, and the provision of preventive tactics for fathers are necessary.
Visnovki
Although most hemangiomas are unlikely to disappear uncontrollably, these episodes can be problematic. It is important to recognize the problematic morphology and/or localization of hemangiomas, avoid diagnostic procedures when necessary, and reverse treatment tactics in case of serious infections.
Prepared by Fedir Yurochko