Polyps are benign growths arising from the mucous membrane.
Author:
- Galkin Alexey Vladimirovich
ENT pathology expert
3.36 (Votes: 11)
Polyps are benign growths of the mucous membrane. Nasal polyps are the result of long-term inflammation in the nose or paranasal sinuses due to prolonged infection, allergens, and certain immune disorders.
Polyps of the nasal cavity and sinuses can appear in both adults and children, but they are more often observed in adults. Drug therapy helps polyps regress in size or slow their growth, but sometimes surgery is performed to relieve the symptoms of the disease. Despite successful treatment, polyps tend to re-grow.
What is a polyp?
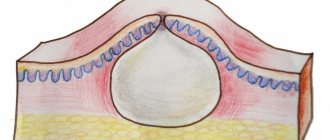
A polyp is a small, benign growth that sometimes appears on the inside of the colon or rectum (anus). Some people may only have one polyp, but it is also quite common for people to have two or more polyps at the same time. A colonic polyp may have a “leg” and a “head” and resemble a fungus growing from the inner lining of the intestine. There are other types of polyps that have a flatter shape, like a “growth” on the inner surface of the intestine. Most often, polyps form in the left half of the colon - the descending colon and the sigmoid colon. But polyps can also be in other parts of the intestine.
Where to remove a mole, polyp, condylomas, papilloma or wart in St. Petersburg
At the Diana St. Petersburg Medical Center, all methods of removing tumors are used, but preference is given to modern laser and radio wave techniques. The clinic has the latest radio wave apparatus. Treatment is carried out without pain and complications under ideal sterile conditions.
Here you can take tests for oncology and blood clotting, undergo all types of ultrasound, get advice from a urologist, gynecologist, dermatologist and oncologist. All doctors have the highest qualification category and extensive experience.
Briefly about the gastrointestinal tract
The colon and rectum (anus) are parts of the gastrointestinal tract. The gastrointestinal tract begins at the level of the mouth and ends in the anal canal. When we eat or drink, food and liquid from the mouth travel through the esophagus to the stomach. The stomach processes food and pushes it into the small intestine. The length of the small intestine is several meters and it is in it that the main processes of digestion and absorption of nutrients occur. Undigested food, water and waste then enter the colon. The largest part of the large intestine is called the colon, and is about 150 centimeters long. It is divided into 4 sections: the ascending colon, the transverse colon, the descending colon and the sigmoid colon. The colon primarily absorbs water and some salts. The colon continues into the rectum, its length is from 15 to 20 centimeters. The rectum accumulates feces (stool) before it is emptied.
Symptoms
For neoplasms in the body or cervix, the most characteristic symptom is heavy bleeding on any day of the menstrual cycle. In this case, it develops independently or after sexual intercourse. The absence of menstruation is one of the possible signs of developing formations.
As polyps grow, other signs of a problem appear:
- Paroxysmal dull pain in the lower abdomen;
- Mucous leucorrhoea;
- Pain, dryness, discomfort during sexual intercourse.
If the patient cannot become pregnant for a long time, polyposis (a large number of neoplasms) of the uterus cannot be ruled out.
Growths on the vaginal mucosa do not cause severe bleeding, but a woman often notices spotting brownish discharge and profuse odorless leucorrhoea on the pad. The patient accurately feels the location of the growth, it pulsates and seems to be bursting. Unpleasant symptoms especially develop during sexual intercourse. If the neoplasm is injured, infection is possible, then foul-smelling greenish-bloody discharge appears on the underwear.
Vulvar polyps usually do not cause obvious symptoms, but women notice small growths during hygiene procedures. If you touch them, they bleed and there is a high risk of infection. Growing tumors, especially during or before menstruation, are very painful.
Types of colon polyps
Typically, colonic polyps are divided into three types: hyperplastic polyps, adenomatous polyps (adenomas), and polyps in polyposis syndromes.
It is quite difficult to determine the degree of risk of an adenoma degenerating into cancer. Clinical studies have been conducted that have shown that if a patient has a single polyp adenoma measuring 1 cm, then the risk of its degeneration into colon cancer within 10 years is 1 in 12, and within 20 years – 1 in 4. Also described and predisposing factors for the degeneration of an adenoma into a tumor, for example, the larger the adenoma, the higher the risk. There are also different subtypes of adenomas, some of which have a much higher risk of developing into cancer than others.
Further we will talk only about hyperplastic and adenomatous polyps, which are most often found in adults.
Complications
Nasal polyps can lead to complications because they interfere with the free passage of air and the drainage of mucous secretions from the sinuses.
Possible complications with nasal polyposis:
- Obstructive sleep apnea. In this condition, prolonged pauses in breathing occur during sleep, which increases the risk of cardiovascular disease and sudden cardiac death.
- Progression of bronchial asthma. Polyposis can aggravate the course of bronchial asthma.
- Sinus infection or infectious complications of chronic sinusitis. Nasal polyps increase the frequency of exacerbations of sinusitis and can lead to serious complications (for example, meningitis, orbital phlegmon, sepsis).
How are polyps diagnosed (identified)?
Most often, colon polyps are discovered during this study. Colonoscopy is a diagnostic method in which the doctor examines the entire colon from the inside. A colonoscope is a thin flexible telescope tube. The thickness of a colonoscope is approximately equal to a finger. It enters through the anus and further into all parts of the colon until it reaches the cecum (the junction of the small and large intestines). A colonoscope has fiber optic channels that transmit light to a camera at the end of the machine. This allows the doctor to examine your intestine from the inside.
Sometimes other testing methods are used to diagnose colon polyps, such as barium enema (a special X-ray test with contrast), sigmoidoscopy (similar to colonoscopy, but uses a shorter telescope), and sigmoidoscopy.
When performing sigmoidoscopy, it is possible to examine the lowest section of the colon - the rectum and the beginning of the sigmoid colon, that is, the final 15-20 centimeters of the colon.
During sigmoidoscopy, the lower third of the colon is examined. Both studies are performed on an outpatient basis and do not require lengthy preparation.
In contrast, a colonoscopy allows you to examine the entire colon. To conduct the study, preliminary preparation of the intestine (cleaning the intestine of feces) is required.
Although stool occult blood testing is an important test for diagnosing various colon diseases, a negative result on this test does NOT guarantee the absence of polyps. If at least one polyp is detected, a complete examination of the colon is required, since in 30% of cases polyps are multiple.
As mentioned earlier, the vast majority of polyps do not manifest themselves in any way. Therefore, in a large number of people who have polyps, they will never be diagnosed (not detected). The above diagnostic methods may be prescribed if you have any characteristic symptoms or if there are other reasons. For example, if a stool test for occult blood is positive, a colonoscopy should be ordered to accurately examine the colon.
Diagnosis of the disease
Your doctor can determine the condition based on your answers to questions about your symptoms, a physical examination, and rhinoscopy (a visual inspection of the nasal cavity using a light and a nasal speculum). But additional examination may be required to determine treatment tactics.
Additional diagnostic tests for polyposis:
- Endoscopic examination. Using an endoscope, the doctor can conduct a thorough examination of the nasal cavity.
- X-ray tomography. Images obtained by X-ray computed tomography (CT) provide information about the extent of polyposis involvement in the nasal cavity or sinuses. These tests can also help the doctor detect the presence of other abnormalities, such as a deformed nasal septum or enlarged nasal turbinates. Based on RCT images, the doctor may suspect a tumor growth other than polyposis (malignant or benign).
- Allergy detection. The doctor may prescribe an additional test to identify allergies: rhinocytogram, blood test for IgE, eosinophilic cationic protein, scarification tests. This is necessary in order to identify the presence of allergic pathology, which contributes to the development of polyposis.
- Test for cystic fibrosis (cystic fibrosis). A child diagnosed with chronic polypous sinusitis should be evaluated for cystic fibrosis. This is a hereditary disease that disrupts the secretion of glands, which leads to chronic inflammation of the respiratory tract and the development of polyposis.
How are colon polyps treated?
If you have a colon polyp or polyps, you will most likely be asked to have them removed, even if the presence of the polyps is not associated with any symptoms. This is done in order to prevent the risk of malignant degeneration of polyps into a cancerous tumor in the future.
Most colon polyps can be removed during a colonoscopy. The colonoscope has a channel through which special long instruments are inserted into the intestinal lumen, with the help of which the polyp is removed. This may be a forceps-like instrument that grasps and lifts the polyp from the intestinal wall, usually used to remove very small polyps. There are other instruments, at the end of which there is a wire electrosurgical loop, with the help of which the polyp is “cut off” from the intestinal wall and at the same time the vessels are cauterized to prevent bleeding.
Typically, the polyp removal procedure is painless and can be performed on an outpatient basis. Patients may also be offered a colonoscopy with the removal of polyps in a state of medicated sleep (“under sedation”, “under anesthesia”), in which case the risk of pain during the procedure is reduced to zero.
Sometimes, multiple procedures may be required to remove large polyps. If the size and location of the polyps do not allow their endoscopic removal, surgical intervention is required.
After the polyp is removed, it is sent for histological examination (examination under a microscope). This is done to make sure that the polyp has been completely removed, to determine the type of polyp, whether it is benign (not cancerous) or whether there are signs of malignant degeneration.
Prevention
You can reduce your chances of polyps appearing or returning after treatment by following these strategies:
- Monitor allergy symptoms. Follow your doctor's recommendations to monitor the course of your allergic disease. If symptoms do not improve, consult your doctor about changing your treatment.
- Avoid irritants to the nasal mucosa. Avoid contact with substances that can cause inflammation or irritation of the mucous membranes (smoke, a suspension of small particles, caustic chemicals, allergens, dust, animal hair).
- Maintain good hygiene. Wash your hands thoroughly and regularly. This is one of the best ways to prevent infections that can cause inflammation of the mucous membranes of the nasal cavity and sinuses.
- Control the humidity in your home. When humidity levels are low, use humidifiers. This will moisturize the airways and improve self-cleaning of the sinuses and nasal cavity.
- Use nasal cleansers. Use a nasal douche (aerosol) with isotonic sodium chloride solution to clean the cavity. This will reduce the concentration of irritating agents on the nasal mucosa (allergens, dust, germs) and reduce inflammation. If you prepare your own saline solution, use distilled or boiled water.
Colonoscopy with removal of polyps (endoscopic polypectomy) is possible:
- free of charge within the framework of compulsory health insurance, that is, under the compulsory medical insurance policy, if there is a referral from a medical institution or a territorial health authority;
- free of charge as part of high-tech medical care, if a previously performed biopsy confirms the malignant degeneration of the polyp;
- on a contractual basis at the request of the patient.
Diagnostic colonoscopy, as well as removal of polyps during colonoscopy, can be performed with intravenous sedation (pain relief).
Traditional methods of treatment
With all due respect to folk, non-traditional, grandmother's, monastery, Kremlin, Tibetan, Martian and other sacred methods: please keep in mind that neoplasms are not the case when you can play Russian roulette with fate. Go to the doctor, and then, when the threat is eliminated, experiment with your health. Tablets, ointments, cauterizations, applications, aromatic oils, injections, drops, prayers, conspiracies against papillomas or condylomas - unfortunately, we have not yet invented them for you.
Please spend two hours on an outpatient procedure, save your life in passing under local anesthesia - and return to your daily activities with clean eyelids. A postoperative story about the imperfections of modern medicine is allowed.