Why does a child develop congenital moles?
Congenital melanocytic nevi (CMN) are benign pigmented tumors consisting of nevus cells that arise as a result of impaired melanoblast differentiation between the second and sixth months of intrauterine life.
UMN occurs in 1% of Caucasian newborns of both sexes.
Visually, such formations have clear boundaries, round or oval outlines, and the surface can be lumpy, wrinkled or folded. Color varies from brown to blue or black. The consistency is usually like that of healthy skin, and hair may grow on the surface.
The reason for their development is always genetic. They can be transmitted from parents or appear on their own, completely by accident.
The time of appearance of such nevi is nonspecific. They are formed during fetal development, but are not always noticeable at birth. In the literature you can find the terms “late UMN” or “with congenital features” - such formations are no different from congenital melanocytic ones, they just appear later.
Typically, UMN are those elements that develop in the first 2 years of life. An important distinguishing feature is that a child’s moles grow with him, in proportion to the baby’s growth.
LNs are often classified as melanoma-dangerous formations, but according to the latest data, such moles are potential precursors of melanoma only in 0.7% of cases.
Some information about moles
All inhabitants of the globe, without exception, have moles - birthmarks. A person is born with moles and acquires them at any age. The majority of moles appear in humans for the first time at 2-3 months of age. The active period for the appearance of new moles is also adolescence in adolescents and the period of waiting for a child in women. Birthmarks can also transform and change during a person’s life.
According to medical terminology, moles are pigmented nevi, which are classified as skin defects that can be congenital or acquired. Such a nevus consists of cells of the epidermis, or dermis, and melanocytes (cells with pigment melanin).
Not all moles are identical: there are normal birthmarks, benign ones, and there are pathological ones, which pose a significant danger to human health and life itself.
What are the types of congenital moles in a child?
VMN come in various sizes, and depending on the diameter they are divided into:
- small - up to 1.5 cm;
- medium - from 1.5 to 10 cm;
- large - from 10 to 20 cm;
- giant - more than 20 cm.
One of the most typical symptoms of VN is hypertrichosis, that is, hair is present on the surface of the formation, most often dense and black. It is worth noting that the appearance of some VN is formed gradually, the nature of the coloring may become uneven, tubercles may appear on the surface, and over time, hair begins to grow.
For VN, such changes are a variant of the norm, but they require monitoring by a doctor.
Melanomic nevi
Congenital melanocytic nevus
All congenital nevi are harmless. Among them there are small, medium and giant formations:
1. Congenital small melanocytic nevus (Fig. 2).
Elements of the rash. A spot or plaque raised above the skin measuring up to 1.5 cm. The shape of the nevus is round or oval, the boundaries are clear or blurred. The surface of the nevus is smooth or wrinkled, lumpy, folded, lobed.
Color. Light and dark brown. In rare cases, a depigmented rim is noted.
Localization. Any.
Course and prognosis. The risk of developing melanoma before puberty is virtually non-existent; in later life it ranges from 1 to 5%.
Rice. 2. Congenital small melanocytic nevus
2. Congenital medium melanocytic nevus (Fig. 3).
Elements of the rash. A round or oval plaque raised above the skin from 1.5 to 20 cm. The surface of the formation is smooth or wrinkled, lumpy, folded, lobulated, covered with papillae or polyps.
Color. Light or dark brown, there may be small dark inclusions on a lighter background.
Localization. Any.
Course and prognosis. There is virtually no risk of developing melanoma before puberty. Average congenital nevi change slightly throughout life. Due to the growth of the child, there is a proportional increase in education. It is advisable to remove the nevus before reaching puberty.
Rice. 3. Congenital medium melanocytic nevus
3. Congenital giant melanocytic nevus (Fig. 4).
Elements of the rash. A plaque raised above the skin level measuring more than 20 cm in diameter. There may be satellite lesions along the periphery of the main lesion. A disorder of the skin pattern is characteristic. On the surface of the formation there are nodules, papules and, as a rule, coarse dark hair. The boundaries can be either smooth or uneven.
Color. Darkly pigmented formation.
Localization. Any.
Course and prognosis. According to various sources, the risk of transformation of congenital giant melanocytic nevus into malignant melanoma reaches 5%. Surgical excision of the formation followed by plastic correction should be carried out as early as possible, however, often the operation is not possible due to the size or location of the formation.
Rice. 4. Congenital giant melanocytic nevus
Acquired melanocytic nevus
Acquired melanocytic nevus can be represented by a borderline (transitional) or complex (mixed) nevus. The transition from borderline nevus to complex nevus to intrademal nevus over time demonstrates the normal evolution of neogenesis.
1. Borderline nevus
Elements of the rash. A round or oval spot, sometimes slightly raised above the surface of the skin, up to 1 cm in size, with clear, even boundaries.
Color. Homogeneous (various shades of brown).
Localization. Any.
Course and prognosis. Borderline nevus, which arose in early childhood, becomes mixed as a result of the proliferation of nevus cells and their advancement into the dermis. This usually occurs during puberty. After the disappearance of the borderline component, the nevus becomes intradermal. This natural transformation usually occurs before the age of 30. In some cases, common borderline nevi remain unchanged throughout a person's life.
Rice. 5. Borderline nevus
2. Complex nevus
Elements of the rash. A formation in the form of a papule or node, usually up to 1 cm in size. The surface is smooth, less often warty, often with the growth of bristly hair. In shape, complex nevi are predominantly formations that rise evenly above the skin.
Color. Generally uniform: dark brown.
Localization. Any.
Rice. 6. Complex nevus
Dermal (intradermal, “resting”) nevus
Elements of the rash. A round, dome-shaped formation, usually up to 1 cm in size, rising above the surface of the skin. Over time, the nevus may develop a stalk and may take on the appearance of a warty (papillomatous) nevus. This phenomenon is most typical for formations localized in the torso area.
Color. Yellow-brown, brown or with brown spots, telangiectasias may be observed.
Localization. The most common are the face and neck. Formations of this group on the trunk and limbs are less common.
Course and prognosis. In most cases, intradermal nevi are not treated. Indications for removal of the formation are: localization in which there is permanent injury to the lesion.
Rice. 7. Dermal nevus
Prevention of the occurrence of acquired nevomelanocytic nevi is to reduce exposure to sunlight (especially in the early period of a person’s life). This is achieved by reducing the time spent in the sun (especially during the peak solstice period from 11 a.m. to 4 p.m.) and using sunglasses.
Blue nevus
Blue nevus can be either congenital or acquired; it most often appears in childhood or adolescence. These skin lesions are much less common than nevi of epidermal melanocytic origin. A blue nevus develops from ectopic melanocytes of the dermis. The coloring characteristic of a blue nevus is due to the Tyndall phenomenon - the refraction of light by the pigment of tumor cells located deep in the dermis.
Currently, several types of dermal melanocytic nevi are considered in the nosological form of “blue nevus”: simple blue nevus, cellular, cellular non-pigmented, combined and deeply penetrating.
Rice. 8. Blue nevus
1. Simple blue nevus (blue nevus, Jadassohn–Tiche nevus
Elements of the rash. The nodule, usually up to 1 cm in size, is sharply demarcated from the surrounding skin, round in shape, hemispherically protruding above the skin level, with a smooth surface.
Color. Blue, light blue, dark blue, gray, bluish - black.
Localization. Any type is possible, but the typical location for blue nevi is the dorsum of the hands and feet. A rare arrangement – soft and hard palate.
Course and prognosis. This formation grows quite slowly, often remaining unnoticed for several years. Over time, a blue nevus may acquire a flatter shape and lose pigment. Transformation of a blue nevus into melanoma is extremely rare.
2. Blue cell nevus (proliferating)
Elements of the rash. The development of a nevus begins with the formation of a spot or compaction in the dermis, which then transforms into a node or plaque up to 2.5 cm in diameter.
Color. Blue.
Localization. Any is possible. Quite often the localization of nevus in this group is the gluteal, lumbosacral region, less often on the dorsum of the hands and feet. Rare tumor localizations have been described - the conjunctiva and the scalp.
The diagnosis is made on the basis of clinical and histological signs; immunohistochemical studies are necessary.
Course and prognosis. Depending on the clinical picture, pathomorphological signs, course and prognosis of the process, two forms of blue cell nevus are distinguished: typical (classical) and atypical with uncertain biological potential. Malignant transformation usually occurs over a long period of time in mature or elderly people and is manifested by rapid tumor growth, ulceration and discoloration. With a cellular blue nevus, cells similar to this formation may be observed in the regional lymph nodes. This process is called “benign metastasis.” Treatment is surgical excision with pathological examination.
Spitz nevus (atypical spindle cell, juvenile, benign juvenile melanoma)
Elements of the rash. A small single dome-shaped hairless node measuring up to 1 cm in diameter. Education, as a rule, is singular.
Color. Pink-red with abundant vascularization, yellow-brown, dark brown, uneven coloring possible.
Localization. Any is possible. In children and adolescents, the most common location is the scalp and face.
The diagnosis is made on the basis of histological examination. A quickly growing dome-shaped formation in a child allows one to suspect a Spitz nevus.
Course and prognosis. Spitz nevus is characterized by a sudden appearance. From the moment it appears, the formation is characterized by rapid growth, then it flattens and remains unchanged for years. Some nevi may undergo morphological transformation into dermal melanocytic nevi, and transformation into melanoma is also possible. The risk of malignant tumor degeneration occurs during puberty. Malignant degeneration is rare, but such formations require careful monitoring. This formation must be removed before the end of puberty. Then, in the postoperative period, dynamic observation is advisable.
Rice. 9. Spitz nevus
Halo nevus (Sutton's nevus)
Elements of the rash. A slightly elevated, slightly infiltrated reddish-brown nodule of round or oval shape, with an average diameter of 4-5 mm. The halo nevus is surrounded by a halo of depigmentation. The diameter of the rim, as a rule, is 2-3 times larger than the size of the hyperpigmented nodule. Characterized by multiple skin lesions.
Localization. Any type is possible, but the most common is the back.
Course and prognosis. There are several stages in the course and resolution of halo-nevus:
- melanocytic nevus with a surrounding rim,
- the central element loses pigmentation and acquires a pink color,
- disappearance of the central element,
- complete repigmentation of the entire nevus over several months or years.
No treatment required.
Rice. 10. Halo nevus
Important features of congenital melanocytic nevi
- Small-sized UMNs are more common and may not appear until age two.
- Small and medium-sized nevi grow more slowly than the child himself and tend to darken and become hairy.
- Large and giant nevi usually occupy part of an anatomical area or all of it, for example an entire limb, neck, part of the back.
- Congenital giant melanocytic nevi transform into melanoma in 6–10% of cases.
Giant VN exceeds 20 cm in size, and such formations are sometimes compared to clothing, called “shirt” or “swimsuit” type. According to statistics, they are rare, affecting 1 in 500,000 newborns.
Giant VNs are only diagnosed at birth. Unfortunately, there is no prenatal screening to detect them, and they are not visualized on ultrasound.
The main medical problem with congenital giant melanocytic nevus is the high risk of developing melanoma, and the tumor can appear anywhere and anytime. What to do in this case? At the moment, the main method is staged excision.
The child's mole is growing. What to do?
Acquired melanocytic nevi (AMN) are benign tumors that arise from melanocytes that have migrated into the skin. They usually appear after six months of life, and reach their maximum size and number at a young age. Subsequently, they may regress or disappear altogether.
The localization of acquired formations is varied. They can be on the skin of the scalp, palms, feet, and also come from the nail matrix, creating difficulties for diagnosis and observation.
Factors influencing the appearance of nevi:
- genetic predisposition;
- level of ultraviolet radiation in childhood;
- phenotypic features of the child’s skin (fair skin, eyes, blond or red hair).
The classification of acquired nevi is varied and includes typical and atypical forms. They are also classified based on the location of the melanocytes.
PMNs are characterized by a round or oval shape and have clear boundaries. Normally they are symmetrical in color, structure and shape.
Most PN are benign and do not require any intervention, but only require lifelong monitoring.
The frequency of malignant transformations in PMN is low, since melanomas most often develop on clean skin, i.e. beyond previous melanocytic nevi. Therefore, their removal for preventive purposes is impractical.
It is worth noting that the tactics for managing patients with melanocytic formations in childhood can be implemented in three ways: surgical excision of the element, dynamic observation of the formation, and zero-intervention tactics, when further observation or surgical intervention is not required. The doctor makes a decision based on an analysis of all factors characterizing the formation: the child’s age, morphology, location, size and melanoma danger of the element.
An important diagnostic point when examining skin formations is to perform dermatoscopy.
Modern technologies have allowed doctors and patients to “monitor” the formation using its mapping. This is a procedure for fixing moles, which makes it possible to evaluate the dynamics of changes in structures, sizes and the appearance of new formations.
Red, hanging moles - which nevi can scare parents?
Nevus Spitz
Histological examination of UMN shows that this nevus accounts for 1–2% of all UMN. This pink-red or deep black mole has a flat, hemispherical shape. The boundaries are clear, even, and the outlines are regular.
The mole grows, changes quickly, initially appears as a small speck, and mothers often confuse it with dirt on the child’s skin.
Spitz nevus is a benign structure, but clinically and histologically it is the main simulant of melanoma. That is why doctors recommend removing it immediately, or taking it under total control and observation.
Red flags for Spitz nevus:
- size greater than 8 mm;
- rises strongly above the skin level, resembles a knot, a hanging mole;
- independent ulceration, i.e. the appearance of a crust on the surface for no reason;
- pronounced clinical or dermoscopic asymmetry.
Galonevus
This is an acquired melanocytic nevus surrounded by a depigmented rim. It is represented by a red-brown nodule that rises slightly above the skin level. The diameter of the nevus itself is small and is approximately 0.2–1.2 cm, but the whitish rim around it exceeds the size of the nodule itself.
This formation is usually not dangerous and does not require treatment, but dynamic observation and mapping of the element is recommended.
Nevus Reed
A black mole with clear, smooth edges. It is small in size, no more than one centimeter, and is a benign formation.
Nevi of Oto and Ito
They are bluish-gray formations with disturbed pigmentation, located in certain areas. The localization of Oto's nevus is characterized by the periorbital region (in other words, these moles appear on the face, around the eyes), and for Ita - the skin of the neck and shoulders.
Most often, these formations require constant monitoring; laser lightening may be used due to a pronounced cosmetic defect.
Summary or briefly about the main thing:
If your mole has enlarged, wait a minute to sound the alarm. First, answer the question: does the mole grow faster than 1-2 mm per year? If the rate is not higher than indicated and there are no other symptoms of melanoma (“geographical” edge, asymmetry along two axes, bleeding without injury, etc.), then most likely everything is fine with the mole. At the same time, if there is even the slightest doubt about the correctness of your conclusions, the oncologist should say the last word during an in-person examination.
If you still have questions, the following will help you:
- In-person appointment with an oncologist
(St. Petersburg) - Mole removal
with histology (St. Petersburg) - My online consultation (from anywhere in the world)
What to do if a child scratches or tears off a mole?
In most cases, nevi are not a cause for concern. The appearance of moles in a child of any age is absolutely normal. They will gradually increase along with the growth of the child himself, and the location of the moles can be anywhere, including on the head, soles and even the genitals. Moles in children can easily be irregular in shape, have uneven borders, varied color patterns and large size, especially for congenital nevi.
It is also normal that moles will arouse your child's curiosity. If a child scratches or even picks off a mole, do not panic. This is only a reason to contact a dermatologist for dermatoscopy and further observation. So the answer to the question of what to do if your baby picks a mole is very simple: don’t worry and make an appointment with a specialist. ⠀
Parents need to be wary only in the following cases:
- rapid, sudden growth of formation in volume or diameter;
- the appearance of bleeding or a crust on the surface of the mole without previous injury;
- a rare type of mole;
- a large number of moles (>50) or cases of melanoma in the family;
- positive “ugly duckling” symptom (one formation is very different from other moles).
If you or your child just touched a mole, there is no need to worry.
How to accurately determine whether a mole is growing or not?
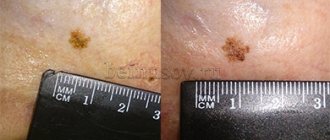
Sometimes it may seem that the mole that we have been carrying all our lives has grown in size. Sometimes it may seem that it has increased greatly. Unfortunately, the words “seems to have increased” will not help the doctor make a diagnosis. Accurate data required. There is an easy way to get them:
- Take a good photo of the mole against the background of a ruler with millimeter divisions. It's better to use a camera with a flash in macro mode. The photo must be taken by another person.
- If you have the slightest doubt about the size of the mole, you need to attach a ruler to it and compare the size with that in the original photo.