Atopic dermatitis in children is a chronic, recurrent inflammatory skin disease with an immune mechanism. As a result of hypersensitivity reactions to various antigens (food products, pneumoallergens, bacterial proteins), a number of inflammatory factors are released in genetically predisposed children.
This results in eczematous lesions, which consist of edema and microvesicles, leading to itching, irritation, scratching and inflammatory lesions, symmetrical, varying in appearance and location depending on the age of the child. It is often associated with asthma, rhinitis and food allergies.
Types of atopic dermatitis
Experts identify the following types of disease:
- Infant (from birth to 2 years). The first signs appear in the first months of life. The rash is localized in the cheeks and forehead. This type of disease is popularly called diathesis. Affected areas become wet and swollen
- Children (from 2 to 12 years old). It worsens when the skin comes into contact with an irritant. It is characterized by excessive dryness and itching.
Depending on the pathogen, there are the following clinical and etiological options: food, fungal, tick-borne and pollen. A type of disease with secondary infection is also distinguished.
Symptoms of dermatitis
Dermatitis, like any other inflammatory disease, is accompanied by a classic pentad - redness, pain, swelling, local increase in body temperature, decreased function of the affected organ. It is worth noting that in children the severity of the clinical picture can vary significantly, which is due to the anatomical and physiological individual characteristics of a particular child and his skin. In addition to the classic ones, there are additional signs:
- rash, crusts on the baby’s skin;
- itching in pathological areas;
- irritability, emotional lability;
- increase in body temperature to 37-37.3 ° C. With the parallel addition of bacterial flora with the development of purulent lesions of the epidermis, fever can reach values of 38°C and higher.
Infants with dermatitis may refuse to feed; Normal sleep is disrupted, the child is constantly capricious. These symptoms are a signal for parents to force them to show their baby to a doctor.
Reasons for development
Childhood atopic dermatitis is a public health problem in developed countries and has a prevalence of 10 to 20%. Within the same country, rates are higher in urban areas and among populations with higher standards of living. With age, the prevalence and intensity of the disease decrease. 60% of patients are diagnosed in the first year of life, mainly in the first six months, in 85% in the first 5 years and only in 10% after 7 years.
In 70-80% of patients it develops against the background of a hereditary predisposition. The genetic basis is combined with various immunological changes in the skin, which cause dysfunction of the protective barrier:
- mutations lead to the appearance of microcracks, transepidermal loss of moisture and pH imbalance;
- this facilitates the entry of environmental irritants, allergens (mites, food, pollen) that increase sensitivity, and pathogens such as Staphylococcus aureus.
These factors lead to cellular infiltration of the dermis and constant inflammation with an initial imbalance of lymphocytes that produce Ig E upon contact with allergens. Subclinical inflammation persists even beyond exacerbation
Main causes of the disease:
- Excessive dryness. Patients have a defect that prevents the skin from moisturizing. The situation is especially worse in winter due to the use of heaters and reduced indoor humidity. Frequent washing without subsequent moisturizing also dries.
- Stimulus. Various household chemicals and low-quality care products can cause burning, redness, itching or dryness.
- Emotional stress. Sheer disappointment, fear and anger are provocateurs to which the child’s skin reacts with itching and redness.
- Excessive sweating. If clothing is not appropriate for the weather, the skin performs the function of thermoregulation - it sweats, which leads to a worsening of the clinical picture.
Separately, infection with staphylococcus should be considered. In this case, outlined areas or vesicles with pus appear. The disease can be caused by herpes and fungus. In rare cases, pollen, dust mites and pets cause atopic dermatitis in very young children.
Causes of dermatitis
The pathogenetic basis for the development of the inflammatory process in the skin is considered to be the release of biochemical substances (interleukins, bradykinins) as the body’s response to the penetration of an allergen into the body.
This allergic reaction is accompanied by dilation of blood vessels in the affected area, the influx of excessive amounts of blood. The result of these changes is an increase in the severity of clinical manifestations. In children, the severity of symptoms directly depends on the duration of contact with the irritant or the amount of it absorbed internally (fruits, low-quality sweets). In addition to the allergic nature of dermatitis, inflammation can occur due to exposure to the following factors:
- applying chemicals to the skin (children's cosmetics, creams, ointments);
- mechanical irritation;
- side effects from taking various medications;
- exposure to ultraviolet, x-rays, electric current.
The key provoking factor for the development of atopic dermatitis is hereditary predisposition. It has been scientifically proven that if one of the parents suffers or has suffered from this disease before, then the chance of a similar pathology occurring in the child is 33%. If mom and dad are sick, then the probability increases to 67%.
Symptoms of atopic dermatitis in children
Clinical manifestations form the basis of diagnosis, as there are no specific microscopic or laboratory changes.
Main manifestations depending on age:
- Babies. Signs of the disease appear from the second month, with erythematous exanthema, with a large exudative component that forms scabs and is localized on the cheeks, forehead, and also affects the nasolabial triangle. Distributes symmetrically to the scalp, front part of the body and limbs. The diaper area is usually left untouched.
- Children from 2 to 12 years old. Skin manifestations may begin at this stage or recur after a free interval of up to 2-3 years. Localization is typical on the elbow bends and popliteal folds. There is a characteristic itching in the affected area. Other typical sites include the thighs, wrists, eyelids, hands and fingers.
- Teenagers. Papular and lichen-like lesions predominate in this phase based on intense xerosis. It is predominantly localized in large folds, on the upper third of the arms and back, the back of the arms and legs, and on the fingers.
Symptoms that should alert parents: dry skin, small cracks in the crease of the earlobe, fingers and toes, redness and peeling on the back of the toes or mouth. Hyperkeratosis, which gives the appearance of goosebumps, is localized on the buttocks, deltoid region, outer thighs and torso. Erythematous plaques on the cheeks, dark circles under the eyes and pallor may occur.
What is dermatitis?
Dermatitis is a skin reaction to external irritants of a biological, physical or chemical nature.
The disease manifests itself in the form of irritation on the skin and can cause the baby not only physical, but also emotional discomfort. The most typical manifestations of dermatitis include:
- redness,
- peeling of the skin,
- rashes that cause itching and pain.
However, dermatitis is not so scary if you know the reasons for its occurrence, be able to distinguish it from other diseases, carry out prevention and seek help from a specialist in a timely manner.
Possible complications
Complications of atopic dermatitis in children:
- Asthma and allergic rhinitis (hay fever). Sometimes eczema precedes these diseases. More than half of young children with atopic dermatitis develop asthma and allergic rhinitis by age 13.
- Chronic itching and flaking. This disorder can cause the affected area to change color and become thicker.
- Skin infections. Infection increases the risk of contracting bacteria and viruses, such as the herpes simplex virus.
- Allergic contact dermatitis. This disease often occurs in patients with atopic dermatitis.
- Sleep problems. The characteristic severe itching can lead to insomnia.
Diagnosis of atopic dermatitis
A test for general and specific Ig E is prescribed to determine the cause of skin inflammation. The doctor makes the diagnosis by examining the affected areas and taking a medical history. The specialist may also use patch tests or other tests to rule out other skin conditions.
If parents suspect that a certain food was the cause of a rash on the child’s body, then they need to inform the doctor about this and ask about the possibility of identifying potential food allergens. In this case, a diet is prescribed for treatment.
About the disease
Dermatitis is an inflammatory process in the patient’s skin, which can occur due to the influence of physical, chemical or biological factors.
In children, the pathogenetic basis for the development of the corresponding problem is initially an inadequate immune reaction such as an allergy or classic inflammation due to exposure to aggressive substances on the skin. One of the most common nosologies of this group is atopic dermatitis. According to WHO statistics, approximately 25-30% of all infants suffer from an allergic form of skin lesions of varying severity. As you get older, this figure drops to 5-10%.
Dermatitis can occur as an acute disease (one-time chemical exposure to the baby’s epidermis) or be accompanied by a chronic course (allergy to milk, citrus fruits, etc.).
Treatment of atopic dermatitis in children
Atopic dermatitis can be permanent. You may need to try multiple treatments over several months or years to control the disease. Even if treatment is successful, signs and symptoms may reappear.
Early detection of the disease allows timely treatment to begin. That is why, when primary symptoms appear, you need to contact an allergist-immunologist or dermatologist.
If regular moisturizing and other personal hygiene measures do not help, your doctor may suggest medication:
- Corticosteroid ointments. Relieve itching and help restore skin. Apply them according to the instructions after moisturizing the skin to avoid adverse reactions.
- Calcineurin inhibitors. Ointments are prescribed for ages 2 years and older. Affect the immune system. Avoid intense sunlight when using these products.
- Medicines to fight infection. Antibacterial cream is prescribed for bacterial infections, open sores or cracks. Oral antibacterial drugs may also be prescribed.
- Medicines to control inflammation. In severe cases, your doctor may prescribe oral corticosteroids.
Effective and intensive treatment for severe forms of the disease involves wrapping the affected area with topical corticosteroids and moist dressings. The procedure is performed under the supervision of medical professionals.
Phototherapy (light therapy) is prescribed to children whose condition does not improve with local treatment. The procedure involves exposure to a controlled amount of natural sunlight alone or in combination with medications.
Although effective, long-term phototherapy has detrimental effects, such as premature aging and an increased risk of cancer. For these reasons, phototherapy is not often used in young children and is not performed in infants.
Diagnosis of dermatitis
“SM-Doctor” is a modern medical center staffed by specialists with over 10 years of experience. The clinic’s extensive experience and high-tech equipment allow our doctors to identify the disease at almost any stage of its development. Diagnosis of dermatitis is not difficult in most cases. A doctor can make a preliminary diagnosis during the initial examination of a sick child. Attention is drawn to the nature of the skin damage, the presence of itching and other typical symptoms. The dermatologist pays special attention to the circumstances under which inflammation of the epidermis occurred. If there is a clear cause-and-effect relationship between the provoking factor and dermatitis, diagnosis is simplified. To eliminate any doubts, the doctor may prescribe additional examinations:
- skin allergy tests;
- serological diagnostics to identify specific antibodies to antigens;
- a set of traditional laboratory tests (blood and urine tests, “blood biochemistry”).
Allergic dermatitis may be a consequence of a lack of enzymes that digest milk, etc. In such cases, appropriate additional laboratory tests are required. Sometimes atopy is a secondary symptom of helminthic infestation. Intestinal parasites secrete aggressive substances that trigger an allergic reaction. To identify this pathology, the doctor prescribes a stool test for worm eggs.
Disease prevention
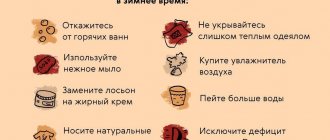
The following recommendations are aimed at preventing episodes of illness and minimizing the effects of dryness after bathing:
- Moisturize your skin at least twice a day. Use creams, ointments, or lotions that lock in moisture. Select one or more products suitable for your child.
- Try to identify and avoid triggers that make the condition worse. Prevent stress, negative effects of pollen dust. Dress your child according to the season to prevent him from sweating.
- Infants and children may experience flare-ups when consuming certain foods, such as eggs, milk, soy, and wheat. Talk to your doctor about how to identify possible food allergens.
- Use only mild soap. Choose products with a neutral pH level. Antibacterial soap removes natural oils and dries out the skin.
Water procedures should not exceed 10-15 minutes. After your bath, dry your skin gently with a soft towel and apply a moisturizer.
Allergic dermatitis
Important preface.
| The text below is aimed solely at site visitors. Any copying of this article or its fragments is prohibited without the written consent of the author. |
Inflammation of the skin of an allergic nature (i.e. allergic dermatitis ) is a very common disease. A child in the first two years of life, without reddening of the cheeks, without occasional spots on the skin, is not so common. Variant names - atopic dermatitis , childhood eczema . The most common, but completely incorrect “folk” synonym is diathesis . Readers who want to clarify the essence of this “wrongness” are asked to re-read or read the chapter “Diathesis” in the book “The Health of the Child and the Common Sense of His Relatives.” The mechanisms of allergic dermatitis are extremely complex. It’s almost impossible to explain them clearly, but medically competently. Nevertheless, understanding the essence of what is happening can guide many parents on the right path and significantly alleviate the suffering of tens of thousands of children. The author tried repeatedly to explain the nature of allergic dermatitis (AD), which is called “on the fingers,” but all attempts to create an article entitled “Allergic Dermatitis” constantly failed. Because a lot of things simply cannot be translated into non-professional language. Enormous difficulties arise, because, in relation to this topic, “correctness” and “understandability” contradict each other . This is where the main difficulty lies. The author, as a practicing physician, observed and treated hundreds of children with AD and came to the conclusion: the explanations and recommendations are quite satisfactory for most parents. Following the recommendations leads to an improvement in the condition of most children. That is, ethically, I simply do not have the right not to disclose information, but explanations for like-minded people and explanations at the level of a scientific work or an article in a popular children's magazine are essentially different things. Because any publication is not only advice for parents. This is also food for the masses of “well-wishers” who see the meaning of their lives in asserting themselves by exposing stupid colleagues. Without the slightest desire to enter into discussions, but having a great desire to reduce the number of letters devoted to the problem of blood pressure, the author addresses this article exclusively to site visitors and once again asks: do not allow copying of this article or its fragments. I would also like to emphasize that in this article the names of some medications will be spoken. Take these names not as a call for self-medication, but as food for thought.
* * *
An allergy is an inadequate reaction of the body to a completely common irritant. Well, a paracetamol tablet should not be a source of allergies. 1000 children ate this pill without any problems, and Seryozha became covered with red spots. A dog ran into the room, it was all right for everyone, but Uncle Petya started coughing and scratching his eyes. An ordinary dog. But for Uncle Petya she is an allergen. Exactly the same as paracetamol for Seryozha. Let's imagine 100 children aged 1 year. And we will give each of them a bar of chocolate. The next morning, 99 children will have problems - some will only have red cheeks, and some will be covered in a rash - from head to toe. Let's wait 10 years. Let's collect the same 100 children and repeat the experiment. With the highest possible probability, 99 children will not react in any “bad” way to chocolate. That is, chocolate was an allergen, but for some reason it stopped being so. Why!? After all, no one treated these children for “chocolate allergy,” but it (the allergy) went away on its own. Let's try to figure it out. An allergy is the body’s reaction to a foreign protein. The immune system detects a foreign protein (antigen) and neutralizes it through the formation of antibodies. Another option is also possible - some substances (they are called haptens) enter the blood, combine there with blood proteins, and these proteins, native in the recent past, acquire foreign properties and become the target of the immune system. Antigen and antibody form special complexes, and these complexes underlie allergic reactions. Let's imagine a squirrel in the form of a chain - like a train and a dozen cars. After we have eaten this “composition”, the enzymes of the digestive system must break down the protein - relatively speaking, disassemble the composition - the train separately, each carriage separately. If this does not happen, if the splitting is incomplete, if the two trailers remain together, they will no longer be a normal, ordinary “digested” protein, but an allergen. The conclusion suggests itself: the immature enzyme systems of the liver and intestines of a 1-year-old child are unable to break down chocolate proteins. And after 10 years, when the liver and intestines “ripe,” no problems arise. And the allergy goes away on its own - without any treatment (“it has outgrown” - grandmothers rightly say). Another option is also possible. Can the child’s body break down this protein. But the amount of protein was so great that there simply weren’t enough enzymes. That is, an allergy did not develop from 100 g of cow's milk, but from 150 ...
* * *
Theoretically, everything seems very simple and the essence of allergic dermatitis is obvious - you ate something wrong, the existing antibodies in the body react to it, and as a result a rash appears. They excluded the allergen, that is, they “calculated” this “something wrong” - and the disease receded (I repeat, theoretically). In practice, everything is not so rosy. The diet is changed many times and the supposedly diseased intestines are “treated”, everything that could cause an allergy, even theoretically, is excluded, but there is no result. Logic dictates that trying to “blame” an allergy solely on the quality of the food is completely wrong. There must be some other factors that provoke the occurrence of blood pressure. The essence of the problem is as follows. Certain substances—foreign or poorly digested—are absorbed into the blood. They can “exit” from the blood in three ways - with urine, through the lungs (if you don’t understand how, read the chapter “Pneumonia”), with sweat. The skin reacts to these substances and a rash appears. That is, the reason is indeed digestion, but is it just the type of food that matters? Any practicing pediatrician will confirm to you: 1) allergic dermatitis extremely rarely occurs in thin and malnourished children; 2) if a child suffering from allergic dermatitis gets an intestinal infection, then against the background of hunger and diarrhea, the symptoms of allergic dermatitis noticeably decrease. Hence an important conclusion: limiting the load on the intestines makes the child’s condition easier. What is the point here: almost always it is a question of the child eating more food than he can adequately digest. Most often this occurs with artificial feeding (or with any bottle feeding). In this regard, we draw the readers' attention to extremely important information. What is the main problem of artificial feeding : a certain time passes between the filling of the stomach and the loss of the feeling of hunger (appetite) - usually 10-15 minutes. If a baby is breastfeeding, then in 5-10 minutes he eats about 90-95% of the amount of food he needs, and then continues to suck until he feels full, i.e. the hunger center in the brain will not respond. When feeding from a bottle, the baby fills his stomach much faster, but the feeling of fullness is delayed, so he continues to suck. That is, a normal healthy child who is fed formula from a bottle always overeats. Let us repeat again in other words, because understanding this point is extremely important. The child needs to eat 100 g of food (the figure is relative, as you understand). In 5 minutes of being near the mother’s breast, the child will eat 95 g, and then for another 20 minutes he will simply enjoy communication and in these 20 minutes he will eat another 5 g. In total, 100 g will be obtained. If we offer a bottle (it doesn’t matter what will be in it - formula or expressed milk), then in the first 5 minutes the child will eat the required 100 g that the body really needs, but the feeling of hunger will not go away, and the child will continue to demand food that , taking into account the domestic mentality, will certainly receive it. And as a result, he will eat 120 g, 150 g, or even more. Please note: if in the first month of life a child is supposed to gain 600 g (in accordance with the norms of medical science), and the weight increases by only 550, all the luminaries of pediatrics living in this region will be raised to their feet. If instead of 600 g the weight gain is 1 kg, then relatives will clap their hands in admiration and rejoice at the size of their cheeks. And no one cares about the fact that after a very short time these cheeks will most likely turn red and begin to itch.
* * *
The food eaten is processed by enzymes, and the amount of these enzymes often does not correspond to the volume of food. As a result, some of the food is not completely broken down; relatively speaking, it lingers in the intestines, rots, and the breakdown products are absorbed into the blood. These absorbed substances are partially neutralized by the liver, and the healthier the liver, the fewer problems. A child’s liver is one of the most immature organs, but its activity, its ability to neutralize absorbed “harmful substances” are very individual. This is why: 1) not everyone has allergic dermatitis; 2) the adult liver can neutralize almost everything, so adults do not have such problems; 3) most children “outgrow” allergic dermatitis, which is due to the “ripening” of the liver. Let's continue. So, the “harmful substances” absorbed into the blood come out with sweat. But very, very often, by themselves they (these substances) do not act on the skin, but have an allergic effect only when they are combined with something in the environment. Where there is no sweat, or where sweat is instantly absorbed (under a diaper), a rash rarely occurs. This is one of the diagnostic methods: if the skin under the diaper is clean, then it is not so much the eating mechanism that is very important, but the mechanism of external contacts . Thus, in order for allergic dermatitis , three prerequisites are necessary: 1) for some harmful substances to be absorbed from the intestines into the blood; 2) so that these substances come out with sweat (i.e., so that the child sweats); 3) so that there is something in the external environment that can touch the skin and react with sweat, causing an allergy. Now the essence of the treatment becomes clear. In order to get rid of the disease, you need to act in three directions: A. Reduce the absorption of “harmful substances” into the blood. B. Reduce sweating. C. Eliminate skin contact with factors that contribute to the development of dermatitis. Now we “treat” in order. A. How to reduce the absorption of “harmful things” into the blood? 1. Achieving timely bowel movements is very, very important. Any constipation, dense stool, or hint of constipation requires immediate help. The optimal and safest treatment for constipation in young children is lactulose syrup (Duphalac, Normaze). Never start using these medications at the age dose indicated in the instructions. Start with a dose of 1 ml per day (once a day, in the morning, on an empty stomach) and gradually increase (by 1 ml every 2-3 days), the maximum is the dose that is in the instructions for your child’s age. Give the effective dose (or the maximum that you will gradually reach) for about a month, then you can slowly reduce the amount of the drug. Let us emphasize that lactulose is completely safe, there is no addiction to it, and if there is a real effect, you can use it for six months or a year. Constipation in a nursing mother is an equally significant factor that provokes the occurrence of blood pressure. Lactulose, suppositories with glycerin, a sufficient amount of fermented milk products in the diet - all this definitely makes sense. 2. If a child is gaining weight well (especially if more than normal), then under no circumstances should you improve the already active digestion with all sorts of enzymes and eubiotics, etc. Undigested food residues rotting in the intestines are an excellent environment for bacteria. In principle, our doctor cannot tell our woman “we need to feed less.” This is so contrary to the national mentality that it doesn’t even occur to me to say something like that. It’s much easier to do an analysis for dysbacteriosis, detect those same bacteria, prescribe more bacteria to help neutralize what has not been digested, plus enzymes. As a result, the mother is in business, the child is diagnosed, the pharmaceutical industry is profitable. Everyone except the child experiences a feeling of deep satisfaction. It's not our fault, but nasty dysbacteriosis. 3. Remember that saliva is an active participant in the digestion process. Slowing down the eating process will increase the benefits of saliva. Make the hole in the nipple smaller, pick up the bottle occasionally, maintain optimal air parameters in the room so that your mouth doesn’t get dry, take more walks. 4. When bottle feeding, the “slowing down of the process” we mentioned is very important. If nothing helps and you can’t reduce the amount you eat, the only real way to help is to reduce the concentration of the mixture. Manufacturers of formulas do not recommend this; moreover, they often write on the boxes supposedly standards that the average child simply cannot master. But the fact remains a fact. If instead of the prescribed 5 spoons you dissolve 4.5 in the same volume, nothing terrible happens, and the manifestations of allergies decrease. The topic of reducing the concentration of the formula is relevant even when the weight gain of a bottle-fed child clearly exceeds the norm. 5. When breastfeeding, try to reduce the fat content of mother's milk. Kefir - 1%, cottage cheese 0%, ban on lard, sour cream, butter, fatty broths, etc. Drink more, sweat less. 6. Prevent the absorption of poisons from the intestines. Intestinal sorbents: enterosgel, sorbogel, smecta, activated carbon, etc. - all this is absolutely safe, it makes sense to use it for both children and nursing mothers. 7. Very often, allergies intensify after a child eats sweets. We're not even talking about candy or cake. They gave me sweet cough syrup and my cheeks turned red. At first glance, this should not be the case. After all, an allergy is a reaction to a foreign protein. And sugar is a carbohydrate; in principle, it cannot cause allergies. The essence of the problem, most likely, is as follows. Sugar activates the processes of decay of those food residues that were underdigested or left the intestines untimely. Decay products are more actively absorbed into the blood - hence the increase in allergies. The conclusions are obvious - limit sweets, if you still can’t, use fructose instead of sucrose, again solving the problem of constipation and excess food. 8. The main thing: do not under any circumstances overload the intestines with food - it is better to underfeed (!!!!!) than to overfeed. I repeat once again: NB! Quite often there is no trace of any allergies. It's not about the quality of food, but about its quantity. Not surprisingly, changing the type of mixture does not fundamentally change anything. But there is often no logic in the actions of mothers and doctors: if a child is allergic to cow’s milk protein, then what should happen after eliminating this protein from the diet is, of course, immediate recovery. What if this does not happen, despite the fact that the child is fed a soy formula or a formula based on goat milk? Logically, cow protein has nothing to do with it... Taking into account the above, it becomes clear that allergic dermatitis is more and more often considered as a sign of protein overdose. Many infant formulas, in which the amount of protein is either reduced or the protein is further broken down, are called hypoallergenic. They just cost... Not every family can afford it. So wouldn't it be more economical to simply limit the amount you eat? Food for thought. The veterinarian advised me, or rather my dog, dry food. What was said was approximately the following: “The dog needs 400 g per day. The dog will need exactly 30 seconds to swallow this portion. And at first you will be constantly haunted by the thought that you are a real sadist who is starving an unfortunate dog weighing under 50 kg. But if you increase the dose, then after a maximum of 2 weeks the dog will begin to itch and we will have to treat allergic dermatitis.” It’s strange that veterinarians thought of this before, and pediatricians still write articles about the relationship between dysbiosis and allergic dermatitis... Q. How to reduce sweating? 1. Maintain an optimal temperature in the room - no higher than 20, ideally 18. Cover the radiators with foam plastic, install regulators, and do not turn on the heaters if possible. 2. Ensure that the humidity is at least 60%: buy a hygrometer, remove dust accumulations, wash the floor frequently, have an aquarium, put a bowl of water, ideally, buy a household humidifier. Ventilate often, walk as much as possible. 3. The minimum possible amount of clothing. 4. Remember that absorbed “harm” comes out not only with sweat, but also with urine. Do not limit fluid intake. C. How to eliminate skin contact with factors that contribute to the development of dermatitis? 1. The most important danger - chlorine in water and detergents - should be eliminated at any cost. Either boil the water filter, or heat it to 80-90 degrees in a boiler and pour it into the bath at that temperature, then wait until it cools down. Sometimes it is enough to boil a bucket of water, cool it and pour this water over the child after bathing. Wet especially problem areas less often, do not wash your face and perineum with water 10 times a day - use wet sanitary napkins. 2. Only special children's powders, preferably without biosystems. Important: after washing, carry out the last rinse in water that does not contain chlorine - either filtered or boiled. The simplest thing is to put it in boiling (very hot) water for a few seconds after washing and rinsing - the chlorine will instantly evaporate. 3. Everything that the child’s skin comes into contact with must be treated in this way: adult clothing in which he is carried, sheets, pillowcases, clothes, diapers. If you lie in your parents’ bed for even a few seconds, your parents’ sheets and blankets should also be washed. If your grandmother comes to visit, give her a robe, washed with baby powder. 4. It is desirable that all children's clothing in direct contact with the skin be white (without dyes) and natural - 100% linen or cotton. 5. How to wear for a walk: a long-sleeved shirt that meets the above requirements, the sleeves protrude beyond the jacket (fur coat, coat, sweater) and are folded, so that other than this shirt there is no chemicals, paint, synthetics, wool, etc. on the skin didn't touch. Likewise, a hat. 6. When bathing, use soap and shampoo (of course, children's) no more often (preferably less often) once a week - any soap-shampoo neutralizes the protective fatty film that covers the skin. 7. Eliminate any toys and care items, the origin and quality of which “is a great mystery.” If you have any doubts that this is high-quality food-grade plastic, don’t! I understand that this is more a question of material capabilities, but one obviously high-quality toy from a respected manufacturer is better than ten masterpieces, no one knows how they were made, delivered and processed. For now, forget about any soft toys. And all rattles, pacifiers, balls, etc. should again be washed not with “Ariel” or “Domestos”. 8. If it is not possible to protect from many external contacts, you should proceed as follows. Buy good white cotton sheets and sew several sets of pajamas for your child - pants and a shirt, long sleeves, a collar that covers the neck. And you need to live in these pajamas, which change as they get dirty. Sleep in them, wear under any clothes. Wash, boil, etc. The beauty of such pajamas is that you can, without fear of ruining valuable clothes, use all sorts of staining ointments, dyes, etc. for treatment. Medicines . We won't tell you much about medications. Still, doctors must treat with medications. The main thing is to understand: there is no golden pill for blood pressure that you eat and everything goes away. Treatment is the implementation of the above set of measures. We have already talked about smecta, sorbents, and lactulose. It's harmless. Please note - the effect of antihistamines (for example, suprastin or tavegil) is largely due to the fact that one of the side effects of these drugs is dry skin and mucous membranes (i.e. suprastin, tavegil, diphenhydramine, pipolfen - all these drugs reduce sweating). The slightest deficiency of calcium in the body increases allergic reactions - it is not surprising in this regard that the manifestations of AD often intensify at the stage of active bone growth and teething. An important factor that provokes calcium deficiency is an overdose of vitamin D. The optimal drug for use by parents is regular calcium gluconate (crush into a fine powder and add to any dairy food). Talk about the ineffectiveness of calcium gluconate (which costs pennies) is explained by the widespread advertising and sale of all sorts of coral and other “calciums”, which cost... well, let's say, quite a lot. The main argument of opponents of calcium gluconate is that it is allegedly not absorbed from the intestines. Let's explain. Calcium absorption is regulated in a very complex way. Calcium absorption is influenced by three main components: 1) a hormone from the parathyroid glands, called parathyroid hormone; 2) thyroid hormone - calcitonin; 3) vitamin D. In order for calcium to enter the blood through the intestinal wall, you need: again, vitamin D, a special calcium-binding protein and very specific amino acids, in particular lysine and L-arginine. All of these substances ensure the active absorption of calcium, although a very small amount can be absorbed passively, mainly in the duodenum (passively - that means, without all these hormones, vitamins and amino acids). Calcium will not be absorbed if any of the above is lacking and if it (calcium) enters the human body (no matter whether it is an adult or a child) in the form of insoluble salts, which has absolutely nothing to do with calcium gluconate, which dissolves even in cold water! Conclusions: calcium gluconate is absorbed by the body and can and should be used as a therapeutic agent where there are indications for this. But if the mechanism of absorption is clear, the fact that calcium gluconate is almost impossible to overdose on is also clear - if it is not needed, then it will not be absorbed. 1 tablet per day - serve for 1-2 weeks, repeat if allergies worsen - it won’t hurt. Treat dry and cracked areas on the skin with panthenol or (better) bepanten, dermopanten - ointment, cream, lotion - do not spare it. You can use topical antihistamines - fenistil-gel, for example. The most effective drugs for eliminating skin manifestations of allergies were, are, and will continue to be for a long time, corticosteroid hormones. Modern drugs (the best, perhaps, Advantan and Elokom) are practically not absorbed from the surface of the skin and do not have an overall negative effect on the body. It is only important to remember: any ointments are a treatment for the external manifestations of the disease, without any influence on the causative factors. The real reason to use hormones is that skin manifestations are no longer just a cosmetic defect. The rash really affects the child’s well-being, there is itching, the child cannot sleep, etc. The mentioned drugs are available in the form of creams and ointments. For deep lesions - ointment, but if the changes are moderate - cream. After obtaining the effect, do not stop using it, but reduce the concentration of the drug. For example, squeeze 1 cm of hormonal cream from a tube and mix with 1 cm of baby cream. After 5 days, change the proportion - 1:2, etc. Remember that cream must be mixed with cream, and ointment with ointment (with bepanthen, for example).
author Komarovsky E.O. published 17/01/2007 12:38 updated 04/02/2019 — Diseases and treatment