According to statistics, foot skin fungus, or mycosis, affects every fifth inhabitant of our planet. This disease, although not fatal, is accompanied by very unpleasant symptoms: severe itching, peeling of the skin between the fingers, redness and an unpleasant odor. coming from the legs. It is important to start treatment in a timely manner in order to get rid of the disease at the initial stage of development. If this is not done, the disease will go into a chronic stage, and then it will be very difficult to eliminate the symptoms of skin fungus and toes.
- Baths
Fungus is itchy and soggy skin between the fingers
Fungal spores penetrate into those areas of the foot where the skin is tender. Under the influence of the parasite, the epidermis becomes wet and destroyed. The fungus destroys proteins in the skin, feeds on them, multiplies and releases toxic products of its metabolism.
Important! Men are more susceptible to fungal foot infections due to constant wearing of closed shoes and increased sweating of the feet.
Among women, dermatomycosis of the legs is more common in athletes. Pedicures pose a certain risk, especially in the absence of sterilization of instruments.
Signs of interdigital fungus on the feet
The initial stages of the fungus often do not have severe symptoms. Itching between the fingers almost does not bother the patient, there is practically no discomfort. This nuance often leads to the fact that an infected person ignores the mild manifestations of a dangerous disease. As a result, the fungus progresses and develops, affecting not only the skin on the foot, but also the nails. If you experience the slightest discomfort, you need to listen to your body, seek help from a dermatologist and begin immediate treatment for the fungus.
There are several main symptoms of mycosis:
- the skin between the fingers begins to noticeably peel off;
- sweating of the feet increases;
- cracks appear on the skin;
- itches between the toes, itching and pain often occur;
- seals form on the sole;
- large, gray or yellow spots form on the fingers and feet (they increase if the fungus is not cured in time).
Forms of fungus: chronic and acute
When a strong immune system suppresses the infection, then the disease occurs in an erased form. A person occasionally feels itching of the skin between the fingers and observes peeling of the epidermis there. Typically, sweating and water procedures lead to increased discomfort.
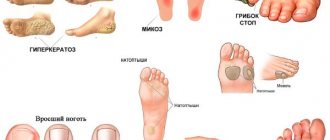
What fungus looks like on the feet in various forms of chronic disease:
- Erased . Peeling is slight, manifests itself in the space between the last and penultimate fingers of the lower extremities.
- squamous . The affected area is covered with small scales and itches after getting wet and sweating.
- Hyperkeratotic. Peeling, a small number of blisters, plaques resembling calluses, discomfort worsens at night.
- Opreloid . Reddened, swollen, weeping skin between the fingers, the epidermis quickly softens, becomes covered with erosions, cracks, which causes pain.
- Dyshidrotic . Numerous blisters, weeping areas, erosions, under which pink-red skin is visible.
Attention! The inflammatory process and wetting occur more intensely in young and middle age. In older people, the skin is prone to hyperkeratosis and peeling.
The acute form of the disease is accompanied by elevated body temperature, painful erosions, cracks, and crusts between the fingers. Once the skin is contaminated, a bacterial infection occurs and an unpleasant odor is felt.
Rules for hygienic pedicure for mycosis of the feet
If fungus affects the feet, interdigital spaces and toenails, you need to get a pedicure at least 2 times a month. The hygienic procedure is performed by a podiatrist.
Medical pedicure includes several stages:
- Steaming the legs. To soften cuticles and calluses, take baths with the addition of an antiseptic.
- Disinfection of skin and nails. Before the procedure, the lesions are wiped with an antiseptic solution - Chlorhexidine.
- Hardware removal of calluses and corns. Special tools and cutters clean off thickenings on the feet and in the toes.
- Nail cutting. The doctor trims the nail plates so that they do not subsequently grow into the skin.
- Treatment of lesions with antifungal agents. Finally, anti-fungal ointment or cream is rubbed into the peeling area.
It is not advisable to do a pedicure yourself during an exacerbation of mycosis. This is dangerous due to self-infection and spread of the fungus to other parts of the body.
The podiatrist has a large number of special tools at his disposal - cutters, skin trimming machines, staples, rasp, scraper, cuticle pushers. Before a pedicure and while cleaning your feet, the doctor must sterilize the instruments. This prevents the spread of infection.
Variety of fungus species
Skin mycoses on the legs are caused by microorganisms belonging to the group of dermatomycetes: Trichophyton, Microsporum, Epidermophyton. They account for 9 out of 10 cases of skin mycoses and onychomycosis (nail fungus). The distribution of microorganisms of the genus Candida is more modest - 9% of all cases.
Treatment of fungus in the folds between the toes is difficult not only because of the variety of types of microorganisms. Pathogens may become resistant to the agents used. Together with constant cases of infection and self-infection, this makes it very difficult to get rid of the infection. Microbial toxins suppress local immunity, the skin is constantly inflamed, because interdigital fungus on the feet weakens its protective properties.
Coffee
Ground coffee in the amount of five tablespoons must be placed in a deep bowl. Pour one liter of hot water over the powder. Wait until the coffee infusion has cooled slightly, then pour it into a basin. Keep your feet in this liquid for about 30 minutes. Put cotton socks on your wet feet and then go to bed. In the morning, rinse your feet with cool water. As a rule, after a month of such procedures, the fungus completely recedes.
Causes of the disease
Fungal infections are transmitted from sick people and pets to healthy people. It must be remembered that germs constantly attack the skin, but not all people get sick. Fungus on the feet and in the spaces between the toes is more common among those who are at risk, are not treated correctly with antibiotics, and do not comply with personal hygiene requirements.
Attention! Fungal spores persist for several weeks in scabs and scales of the epidermis, especially with high humidity on the floor in the bathroom, shower, or around the pool.
Increase your chance of getting a fungal foot infection:
- heavy sweating;
- immune disorders;
- hormonal imbalance;
- thyroid diseases;
- cracks, abrasions of the skin, wounds on the legs;
- deficiency in the body of vitamins A, C, and the microelement zinc;
- metabolic disorders;
- diabetes;
- overweight.
Where does mycosis come from?
The development of a fungal disease on the feet is quite often diagnosed in those people whose immune systems are very weak. In addition, mycosis develops actively with vitamin deficiency, in the presence of heavy sweating, with impaired metabolism, as well as with existing wounds on the feet and toes.
In the field of medicine, experts distinguish two types of fungal infection between the fingers: indirect and direct. As for the direct route of entry of the fungus into the human body, it includes:
- Contact with an animal or person who is already developing mycosis.
- By touching soil and plants, you can easily contract the disease.
In case of indirect infection with mycosis, this disease may be preceded by:
- Use of items that were used to serve an infected animal.
- Operation of any item used by a person with fungus.
Symptoms and diagnosis of the disease
In the area of the skin where the fungus develops, a slight itching is initially felt, but many do not attach importance to this symptom. This is followed by swelling, redness and peeling of the skin, small blisters and maceration (wetting of the epidermis) may appear. Cracks and erosions often appear; when skin flakes peel off, a burning sensation is felt and an unpleasant odor appears.
Attention! Signs of a fungal infection are first observed in the space between the fourth and fifth toes of one foot.
When conditions are favorable for the fungus, the primary lesion expands, persistent itching appears, which intensifies in the heat and when the feet sweat. The skin in the affected area is constantly inflamed and irritated, covered with white scales and scabs. After they are cleansed, burning and pain occur.
Diagnosis of the disease is carried out by a dermatologist or mycologist based on an external examination of the patient and laboratory tests to identify a fungal infection.
Herbal baths
The use of medicinal plants helps to quickly overcome fungus, get rid of inflammation, as well as improve the healing of existing cracks and disinfect wounds. The following medicinal plants have a high antifungal effect:
- Canadian goldenseal.
- Golden mustache.
- Oak bark.
- Carnation.
- Shell of black walnut fruit.
- Celandine.
The following herbs have antiseptic and regenerating effects:
- Mint.
- Sage.
- Chamomile.
- Calendula.
- St. John's wort.
- Nettle.
To prepare a solution for a foot bath, you need to take two spoons of any herbs and pour them with one glass of boiling water. The broth should sit under the lid for 30 minutes. The liquid is then filtered through gauze. The prepared solution is diluted in five liters of warm water, where the feet are then immersed. This procedure should last about 20 minutes.
You can also make your own collection by taking the required plant varieties in equal proportions. In this case, it is best to combine plants with different directions of action.
Local treatment with antiseptic agents
The dark purple crystals of potassium permanganate are shaken with warm water to create a concentrated solution. It is added to water and taken in foot baths, or cotton pads are soaked in the liquid and used as lotions.
Antiseptics and antimicrobial substances will help get rid of fungus:
- Alcohol solution of iodine.
- Sulfur-salicylic ointment.
- Salicylic alcohol.
- Potassium permanganate.
- Boric acid.
- Resorcinol.
- Fukortsin.
Attention! Antiseptics relieve itching of the skin and limit the spread of infection, but these medications cannot completely get rid of the fungus in advanced cases.
Iodine tincture has a strong antimicrobial effect. Before treating the fungus with this remedy, it is necessary to lubricate the healthy skin around the peeling area with Vaseline.
Salicylic ointment is better suited for treating the hyperkeratic form of foot fungus. The active substance in the composition has an antiseptic effect. The product softens scabs, relieves inflammation and pain, and facilitates cleansing the skin of parasite waste products.
Soda baths
You need to fill the basin with warm water. Dissolve one tablespoon of soda and salt in it, mix everything thoroughly. Then lower your feet into the resulting solution and hold for several minutes. At the end of the procedure, rinse the limbs with clean water, put on socks, which should be soaked in wine vinegar in advance. With this compress you need to sleep all night. As a rule, the fungus recedes after several such procedures.
Local treatment with antifungal drugs
They get rid of fungus at home using pharmaceutical sprays, ointments, gels and creams. In difficult cases, medications in tablets prescribed by a dermatologist are additionally taken orally.
Fungoterbin
This is the name of the line of drugs based on the fungicidal substance Terbinafine. They produce spray, gel and cream Fungoterbin. There is the same drug in tablets. The treatment course for uncomplicated forms of fungus is 1 week.
Lamisil
Antifungal drugs are produced under this trade name in the form of a spray, solution, gel, ointment, cream. The active substance in the composition is Terbinafine.
Bifosin
The active ingredient in the cream, solution and spray is Bifonazole - an effective fungicidal agent. It is recommended to use for treatment and prevention for 3 weeks.
How to treat fungus between the fingers: drugs from the pharmacy
Toenail fungus between the toes requires long-term treatment with antifungal agents. At the first stage of mycosis, local remedies are used - aerosols, gels, creams, liniments. If the infection spreads to the nails and feet, take systemic antimycotics in the form of capsules and tablets. The duration of therapy varies from 1 to 6 or more months.
For topical use
Interdigital mycosis of the feet is treated with antifungal agents, which contain:
- clotrimazole;
- econazole;
- terbinafine;
- levorin;
- ketoconazole;
- Naftifine.
Too frequent treatment of the feet with local antimycotics can lead to skin irritation and blistering rashes.
The following pharmaceutical preparations are used to treat affected areas:
- Binafin is a terbinafine-based cream that destroys pathogens of mycosis of the skin, hair and nails. Used to treat the skin between the fingers 2 times a day.
- Lamisil is an antifungal cream that kills dermatophytes, yeasts and molds. Apply to areas of peeling up to 2 times a day.
- Mycospor is a cream with bifonazole that destroys pathogenic flora on smooth skin. Rub into the interdigital area of the feet once a day before bed.
- Nizoral is an ointment with ketoconazole, effective in the treatment of mycosis on the legs and skin folds. Apply to the affected areas and 2 cm of healthy skin around them once a day.
- Exoderil is a cream with naftifine that eliminates most pathogens of fungal infections. Used in the treatment of mycosis of nails and skin up to 2 times a day.
The course of treatment for fungus in the interdigital area is 2-4 weeks. If the nail plates are affected, treatment is extended to 3-6 months.
For oral administration
Antifungal drugs are prescribed orally for complicated disease. To destroy the fungus, tablets with itraconazole, ketoconazole, terbinafine and other antifungals are used. Typically, therapy includes the following:
- Fluconazole is an antifungal tablet from the triazole group that inhibits the growth of fungus. If the skin and nails are affected, take 150 mg of the drug once a week.
- Griseofulvin is an antibiotic active against trichophyton and microsporum. If the interdigital spaces are affected, 1 g of medication per day is prescribed.
- Lamisil - tablets with terbinafine destroy most parasitic fungi. Adults take 250 mg of the drug once a day.
- Diflucan - antifungal capsules destroy candida flora. If the toes are affected, 1 capsule is prescribed once.
Systemic antimycotics place a greater burden on the liver. Therefore, they are taken only as prescribed by a doctor in the recommended dosage.
Systemic therapy
In most cases, only external use of antifungal agents is sufficient. It is recommended to ask your doctor about which drug is best to use. If a fungal infection develops against the background of severe internal diseases, then local and systemic therapy is combined.
It is important! The use of medications and alternative medicine recipes must be combined with proper foot skin care.
Treatment with antifungal drugs taken orally will be required in advanced cases. Additionally, the doctor prescribes immunostimulants and vitamin-mineral complexes. Complete healing takes several months, and only if the chosen remedy corresponds to the form and stage of the disease.
Complications of interdigital mycosis
The progression of the disease is fraught with damage to the nail plates. Inadequate treatment leads to atrophy of the subungual bed. This creates conditions for bacterial infections to attach.
Untreated mycosis is dangerous due to the following consequences:
- transfer of infection to nails;
- bacterial skin inflammation;
- purulent necrotic bone disease.
Over time, the fungus spreads to the back of the foot, toes, and ankle. This leads to the transition of mycosis to a generalized form.
Treatment with folk remedies
At home, they independently use antiseptics and fungicides. Treatment of fungus between the toes with folk remedies helps reduce discomfort in the first week.
Foot baths
A soda solution for the treatment of interdigital fungus on the hands and feet is prepared from 2 liters of water, 2 cups of table salt and 1 tbsp. l. soda
Baths with decoctions of medicinal plants are useful for fungus between the toes: celandine, wormwood, oak bark, birch leaves, willow bark. Brew the raw material and boil over low heat, or preferably in a water bath, for 5–15 minutes. The proportions of grass and water are 1:5.
Sometimes more plant materials are brewed to increase the concentration of biologically active substances in the solution, increasing the impact on the causes of the disease. Baths with plant decoctions or soda solution are done in the evening. Take the procedure for 30 minutes.
Lotions and compresses
Propolis and its tincture are strong folk remedies for fungus on the skin between the toes, having an antimicrobial and healing effect. Use 10 or 20% alcohol tincture for lotions and compresses. You can prepare the product yourself or purchase it at a pharmacy.
Vinegar - table vinegar from the store or homemade from apples and cherries - helps relieve itching and unpleasant odor. The acid changes the pH of the skin, which stops the growth of the fungus. They make lotions with vinegar, calendula tincture, and strong tea leaves.
Egg
The chicken egg must be placed in a jar. Pour it with vinegar essence with a concentration of 70%. The egg is then placed in a dark room for several days until the shell begins to dissolve. After this, remove the film and add one teaspoon of butter to the jar. Mix all ingredients thoroughly. Infuse the home remedy for another day. The finished ointment is used to treat skin that has been affected by fungus. Procedures should be performed twice a day. Therapy for the disease should last about a week.
Prevention
It is necessary to observe the rules of personal hygiene and care for the skin of your feet. Socks should be washed at a temperature not lower than 40°C. It is recommended to treat the inside of shoes with a formaldehyde solution or a special spray. It is advisable to choose shoes made from natural materials; in summer, wear sandals and sandals more often.
If the areas between the toes are wet and very itchy, then use products that do not increase sweating. These are spray, lotion and powder (powder). For the dry form of the fungus, a good option is an ointment or cream. Before applying the product, be sure to clean the affected area of scales and scabs using a warm foot bath.
Shoe care and prevention
Mycosis between the toes is a serious and insidious infection. If you have recovered from a fungus and do not want to become infected with it again, you must follow some simple preventive rules. They are as follows:
- It is not recommended to put someone else's shoes on your feet, especially wearing them for a long time. If you are invited to visit, you should refrain from suggesting the use of slippers; it is best to stay in socks or put on the house shoes that you took with you.
- You should maintain your immune system in good condition, take vitamins, and also adhere to a healthy, balanced diet.
- During the cold season at the workplace, it is best to change into replacement shoes, so you can avoid excessive sweating, which is considered a provoking factor in the development of fungal infections.
- If you are going to visit the sauna or swimming pool, then you need to take slippers or flip-flops with you.
- After bathing, the feet are wiped dry, paying special attention to the areas between the toes.
- Socks, tights, and stockings must be changed daily.
- It is not recommended to share such personal hygiene items as a nail file, washcloth, nail scissors and much more with another person.
- It is not advisable to try on new shoes in a store on bare feet, since previously they could have been worn by people infected with fungus. It is best to carry a cotton or nylon sock with you while shopping.
Particular attention should be paid to your feet, taking proper care of them, as a result of this the fungus will bypass you.