Brief description of the disease
Streptococcus is an opportunistic microorganism that is normally present on the skin of all people. For it to reproduce, damaging factors must occur. These include:
- decreased immune system resistance;
- frequent use of antibacterial agents for other purposes or in large dosages;
- the presence of hemolytic type streptococcus;
- the presence of lesions on the skin through which pathogenic microorganisms penetrate.
Streptococcus in children often settles in places of frequent cuts, abrasions, and insect bites. The skin looks intact on the outside, but there are microcracks on it through which bacteria penetrate, causing inflammation. First, redness and accumulation of serous exudate form, then pus is released.
One child may suffer from the pathology, but it often appears in the form of an outbreak of an epidemic, for example, in a kindergarten.
Pathogenic microorganisms spread from an infected person or carrier, or household items. The patient's body temperature rises and his health worsens. Intoxication of the body occurs, causing headache, joint, and muscle pain. The main symptom: the skin suffers, profuse suppuration appears on it, penetrating to the deep layers of the epidermis.
Conducting diagnostics before prescribing treatment
It is impossible to determine the method of therapy if the exact cause of the pathology is not established. Several types of diagnostics are used to differentiate the diagnosis. Laboratory and instrumental methods are used.
- Collecting anamnesis from the parents or child.
- General inspection. Areas of redness, inflammation, and damage to the skin appear on the body. Due to the proliferation of streptococcus, erosions and ulcers can form. Rashes containing pus are often observed.
- General clinical analysis of urine and blood, biochemical test. Determine the condition of internal organs and biological fluids. With bacterial carriage, the ESR is increased and the number of leukocytes is increased.
- Bacteriological culture. This is the main method for identifying the pathogen. A smear is taken from the affected area and inoculated onto a nutrient medium. The result is determined after 5-7 days. They identify not only the bacteria, but also the antibiotics to which it is sensitive.
Using bacteriological culture, drugs to which the microorganism is sensitive are found. This allows the doctor to prescribe the correct method of therapy. The risk of using too many antibiotics, which can lead to superinfection, is eliminated. That is, a strain of pathogenic bacteria that lacks sensitivity to any type of antimicrobial agent.
How is streptoderma transmitted?
The main route of transmission of infection is through household contact. The disease occurs through close contact with an infected person, sharing common things, bedding, and household items with him.
Sometimes there are cases of infection with streptococcus through insect bites (mosquitoes, midges) or when the pathogen gets into the wounds through dust in a sports hall or gym. In rare cases, streptoderma develops as a result of mechanical damage to the skin (cuts, scratches, abrasions).
Hygiene rules during therapy
In addition to using medications, the patient and parents must observe hygiene rules so that the pathogen does not spread to other people. Streptoderma is contagious, so the child is dangerous and can cause an outbreak of the epidemic. The following methods are distinguished aimed at normalizing patient hygiene.
- During the first 4 days of therapy, you should not wash. Otherwise, the consistency of the lesion will become moist, and the infection will spread to other areas of the body. The use of ointments becomes difficult.
- To prevent contamination of the body during the period of no bathing, the affected areas are wiped with a towel with water or herbal decoctions.
- Do not scratch the affected areas. For severe itching, apply antihistamine ointment.
- Availability of individual personal hygiene products, cutlery, toys for the period of illness. The rule continues after therapy to prevent the spread of other infections among children.
- Soft toys are washed and put away during treatment. They use objects made of plastic, wood and other hard elements. They are washed and disinfected.
- Bed linen, clothes, and towels are ironed with a hot iron.
- Scratches and wounds are treated with an antiseptic.
The use of hygiene methods does not eliminate the disease, but controls it and prevents infection of other people. If parents continue to take their child to a public institution, there is a risk of an epidemic.
Preparations and products for topical use
Affected areas and surrounding tissues must be periodically disinfected. Older drugs were previously used to treat streptoderma in children, but these methods are no longer recommended due to the high risk of side effects. These include silver nitrate and mercury ointment.
Additionally, herbal infusions were used. These include chamomile, calendula, string, coltsfoot. They have antiseptic, anti-inflammatory, healing properties. The method is effective, but traditional methods are auxiliary components. Requires the use of medications.
Some dermatologists and pediatricians advise using a solution of potassium permanganate. It is not sold in all pharmacies. You can buy it only with a doctor's prescription. This causes complications with prolonged therapy.
It is recommended to use modern antiseptics and antibiotics with high-quality composition. They are applied in a course of no more than 10 days so that the bacteria does not develop resistance to the active substance.
Antiseptic treatment
Unlike antibiotics, antiseptics contain components that rarely cause adverse reactions. This reduces the risk of allergies that worsen a person’s well-being. It is preferable to use the following means:
- brilliant green, 2%;
- hydrogen peroxide, 1%;
- salicylic alcohol, 2%;
- boric acid;
- fucorcin.
When the medicine is applied for the first 1-2 days, the child feels pain and burning. As the skin heals, the discomfort disappears. It is recommended to treat the affected areas and the skin around them in a diameter of 5 cm every day. When the affected area has dried after applying the solution, use the ointment. It has a thick consistency, so it lingers on the tissues, causing a prolonged effect.
Antiseptics cannot be used as the only treatment; antibacterial ointments must be used.
A decoction of plants has an antistatic effect. They destroy some bacteria, relieve irritation, itching, and pain. But folk remedies are not used as the main method of treatment. Their effectiveness is not enough.
Local antibacterial therapy
Antibiotic-based ointments are used, and an additional substance of steroid origin is used less frequently. The product destroys pathogenic microflora, relieves inflammation, and heals tissue. Types of combination drugs and their prices are presented in the table.
| Antibacterial ointment | Price, rub.) | Ointment with antibiotic and hormone | Price, rub.) |
| Levomekol | 40 | Triderm | 750 |
| Erythromycin | 30 | Akriderm | 420 |
| Tetracycline | 50 | Kanizon | 500 |
| Retapamulin | 120 | Celestoderm | 500 |
| Bactroban | 300 | Lorinden | 320 |
| Mupirocin | 370 | Belogent | 350 |
| Lincomycin | 50 | ||
| Gentamicin | 30 | ||
| Sintomycin | 40 | ||
Combination ointments use antibacterial and anti-inflammatory components; an anti-fungal substance may be present. This is due to the fact that with prolonged antibacterial therapy, candidiasis can develop, worsening the condition of the tissues.
Before a year, the use of steroids, even topically, is not advisable.
Hormonal components negatively affect the baby’s endocrine system. There is a risk of health problems. A dermatologist can prescribe a drug, but the effect caused must exceed the risk of side effects.
Principles of antibacterial therapy
Before using antibiotics, the doctor warns the patient about the risks that arise from improper use. It is prohibited to use the products for more than 10 days.
You cannot apply or drink large doses, this will cause resistance of the pathogenic microflora. There are 2 ways to use antibiotics.
- Locally
. The product penetrates only into the deep layers of the epidermis, bypassing the systemic bloodstream. Therefore, adverse reactions in the form of dyspepsia and neuralgia do not appear. - Systemically
. Use tablets, capsules, injections. A form of the drug is prescribed for severe lesions to cause rapid action. It is recommended to additionally consume lactobacilli to prevent dyspeptic disorders. The product penetrates into all tissues, so there is no risk of streptococcus spreading inside.
The bacterium causes extensive inflammatory processes. This is due to an immune reaction that directs lymphocytes to the lesion, releasing inflammatory mediators. To eliminate the effect, not only antibiotics are used, but a complex with hormonal substances.
For children under 5-6 years of age, drugs in the form of a suspension are preferable. They have a gentler effect on the gastrointestinal tract and are less likely to cause disruption of stool formation. An older child or adult is prescribed tablets. Injections are rarely used.
Therapy for pyoderma
Bacterial skin infections are an interdisciplinary problem; they are encountered in the practice of surgeons, therapists, pediatricians, and gynecologists.
Pyoderma (from the Greek pyon - pus, derma - skin) constitute a large group of dermatoses with different clinical forms, course and prognosis, which are based on purulent inflammation of the skin, its appendages and subcutaneous fatty tissue (Fig. 1).
Skin diseases associated with the activity of bacteria, both pathogenic and opportunistic, are characterized by nosological diversity. The infectious process in pyoderma is sometimes not limited to only a local effect - the development of inflammation, but can cause serious damage to the general condition of the body (for example, staphylococcal and streptococcal toxic shock syndromes), leading to the occurrence of diseases that occur without inflammatory phenomena (point keratolysis) [1, 2 ].
The causative agents of pyoderma are mainly staphylococci and streptococci, which belong to the gram-positive microbial flora. The occurrence of suppuration of the skin under the influence of staphylococci and streptococci is explained by the influence on it of various metabolic products secreted by pyogenic cocci during their life activity (exotoxins, enterotoxins, enzymes, etc.).
In Russian dermatology, the generally accepted classification of pyoderma proposed by Jadasson (1949) as modified by A.A. Kalamkaryan (1954) and S.T. Pavlova (1957), according to which pyoderma, depending on the pathogen, is traditionally divided according to the etiological principle - staphyloderma and streptoderma, as well as mixed ones - streptostaphyloderma. According to the course of the disease, acute and chronic forms are distinguished; according to the depth of the lesions - superficial and deep, and according to the mechanism of occurrence - primary and secondary.
Clinical manifestations of pustular skin diseases are varied. The most common are folliculitis, sycosis vulgaris, furuncle, carbuncle, hidradenitis, impetigo, chronic ulcerative pyoderma. Infants may develop epidemic pemphigus of newborns, etc.
Pyoderma often complicates itchy skin diseases (so-called secondary pyoderma), especially scabies, eczema, neurodermatitis, and atopic dermatitis. Often, secondary pyoderma is observed in pemphigus, herpes zoster, mycoses, and necrotizing ulcerative angiitis.
Treatment of pustular skin diseases remains one of the pressing issues in the treatment of dermatoses [3].
Treatment of pyoderma should always be comprehensive and include a special regimen of behavior and skin care, diet, local and systemic medications, as well as physiotherapeutic procedures.
In the treatment of pustular skin diseases, it is necessary to observe the basic principle, namely, to carry out etiotropic treatment, i.e., affecting the pathogen, and pathogenetic treatment - to eliminate factors contributing to pyoderma and correct concomitant pathology.
The regimen of a patient with pyoderma primarily involves rational skin care, both in the lesion and outside it.
In localized forms of the disease, it is not recommended to wash the skin only in and near the lesion, and in the case of a disseminated process, washing is prohibited altogether.
The hair in the area where pyodermic elements are located must be cut off (do not shave!).
Unaffected skin is treated, especially carefully around the lesion, with disinfectant solutions (1–2% alcohol solution of salicylic acid, 0.1% aqueous solution of potassium permanganate, etc.).
In order to prevent the spread of infection, nails should be cut short and treated with a 2% alcohol solution of iodine twice a day.
In case of long-term ongoing processes, as well as in case of multiple rashes, special attention should be paid to diet: meals should be regular, nutritious, rich in vitamins; sharply limit the amount of salt and carbohydrates; Alcohol is completely excluded.
For local treatment of superficial forms of pyoderma, alcohol solutions (salicylic acid, camphor), aniline dyes (fucorcin, 1% brilliant green, 0.1% potassium permanganate), topical antiseptic and antimicrobial drugs are used. If necessary, taking aseptic measures, the cover of the phlyctena and pustules is opened, followed by washing with a 3% solution of hydrogen peroxide (hydrogen peroxide) and lubrication with disinfectant solutions: nitrofural 0.1%, iodine alcohol solution 5%. Chlorhexidine (0.5% alcohol or 1% aqueous solution of chlorhexidine digluconate), dioxidine, eucalyptus leaf extract, microcide, povidone-iodine, etc. are widely used as antiseptics; Aerosols are also effective for external treatment, since they are evenly applied to the surface and quickly penetrate the skin: triamcinolone, hydrocortisone + oxytetracycline, lifusol, dexpanthenol. Ointments containing antibiotics and sulfonamides are applied to common multiple lesions: 2% ointment, fucidin cream, 2% mupirocin ointment, sulfadiazine, bacitracin + neomycin, silver sulfathiazole, levomekol, heliomycin ointment 4%, lincomycin ointment 2%, gentamicin ointment 0.1 %. The course of treatment is 7–14 days.
Topical combined glucocorticosteroid drugs with anti-inflammatory and antibacterial effects are prescribed for secondary pyoderma of the main dermatoses (atopic dermatitis, scabies, eczema, etc.): fucicort, fusidic acid, hydrocortisone + oxytetracycline, lorinden C, celestoderm with garamycin, travocort, etc. Course of treatment 7 -14 days.
In the treatment of superficial forms of pyoderma (ostiofolliculitis, folliculitis, impetigo, ecthyma), a good therapeutic effect was obtained using silver sulfathiazole - 2% argosulfan cream [4].
After the initial treatment of deep limited foci of staphylococcal infection, absorbable agents, enzymes, ointments are also indicated that accelerate reparative processes in the skin, ensure deep penetration of the drug and limit the spread of pus: ichthammol, 0.25% trypsin solution, chymotrypsin, levosin, pyolysin, actovegin, solcoseryl, zinc hyaluronate.
To treat ulcerative lesions in pyoderma, epithelializing ointments and dressings are used, and to cleanse necrotic masses - iruksol, trypsin, chymotrypsin. Recently, an impressive effect in the treatment of ulcerative defects in pyoderma has been obtained from the use of 2% argosulfan cream. As an active principle it contains the silver salt of sulfathiazole, which has a powerful antibacterial effect on gram-negative and gram-positive microorganisms (staphylococci, streptococci, Proteus vulgaris, Escherichia coli, clostridia, etc.). and is more than an order of magnitude superior to the similar effect of sulfonamides alone. Silver ions contained in the cream weaken the sensitizing properties of sulfonamides, and due to binding to the RNA of microbial cells they also have a bacteriostatic effect. The silver salt of sulfathiazole has poor solubility and absorption from the wound surface, which makes it possible to maintain a more or less constant concentration of the drug at the site of inflammation for a long time. Sulfathiazole, as a component of the cream, inhibits the proliferation of microorganisms. The hydrophilic base of the cream, which has an optimal pH value and contains a large amount of water, provides a local analgesic effect and moisturizes the wound, promoting tissue repair. The drug is applied to the lesions 2-3 times a day.
We used argosulfan in the treatment of pyoderma gangrenosum. Its use as part of complex therapy made it possible to achieve complete or almost complete clinical cure in all patients. This was expressed in the reduction or disappearance of pain during and outside of dressings, in the cleansing of the ulcerative defect from necrotic tissue and the appearance of mature granulations and marginal epithelization in the area of the ulcers, as well as in the absence or sharp decrease in the growth of microflora. The use of argosulfan in all patients led to rapid scarring of the ulcers (on average within 20–22 days, depending on the depth and extent of the defect), while during the treatment the patients did not note any side effects from the local therapy.
In order to sanitize the entire skin, general ultraviolet irradiation or wiping of visually healthy skin with disinfectants is recommended. If there is no effect from external treatment of deep lesions on the face, neck (furuncle, carbuncle), with pyoderma complicated by lymphangitis, lymphadenitis, etiotropic treatment with broad-spectrum antibiotics (parenterally or orally) is indicated.
Systemic antibiotics for pyoderma are used for long-term chronic course of the process, its high prevalence, the presence of general phenomena (fever, headache, malaise) and regional complications (lymphadenitis, lymphangitis), localization of deep pyoderma on the face, especially in the area of the nasolabial triangle.
Treatment of patients with chronic pyoderma with systemic antibacterial drugs should be based on the results of bacteriological analysis with determination of the sensitivity of the microflora to them.
In recent years, penicillin preparations have practically not been used in the treatment of pyoderma. Currently, the most effective and at the same time causing the least number of adverse reactions are antibiotics - macrolides (erythromycin, josamycin, clarithromycin, etc.), lincomycin, tetracyclines (tetracycline, metacycline, doxycycline). You can also prescribe rifampicin, ceporin, cefazolin, cephalothin, cefotaxime, ceftriaxone and other antibiotics that are resistant to β-lactamases and have a wide spectrum of action. Single and course doses of antibiotics and the method of their administration are selected individually depending on the clinical picture and the course of the process.
Less often than antibiotics, usually in case of intolerance, sulfonamide drugs are used, which are less effective and often cause toxicoderma. Long-acting drugs (sulfamonethoxine, co-trimoxazole, etc.) are usually used.
In outpatient practice, it is advisable to use only oral antibiotics with high bioavailability and a long half-life (which allows reducing the number of doses per day), while the effect on the intestinal microflora should be minimal.
When treating in a hospital, preference is given to parenteral administration of antibacterial drugs. In step-by-step treatment, the antibiotic is first prescribed parenterally, and if the patient’s condition improves (after 3–7 days), they switch to oral administration. For primary skin infections, penicillin antibiotics are chosen, alternative drugs are II and III generation cephalosporins, lincosamides and fluoroquinolones. For mild or moderate forms of the disease, oral dosage forms are prescribed.
In acute cases of the disease, an antibiotic is prescribed for a course of at least 5–7 days, in chronic cases – for 7–10 days.
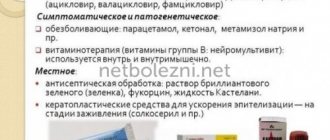
In addition to antibacterial therapy, immunotherapy is widely used for chronic forms of pyoderma. Active specific immunotherapy includes staphylococcal toxoid (native and adsorbed) and staphylococcal antiphagin, staphyloprotectin, which is a mixture of cytoplasmic staphylococcal antigen and toxoid (the drug is administered subcutaneously into the area of the lower angle of the scapula 2 times a week). The first injection is in a dose of 0.3 g, the next four are 0.5 g each. Patients with severe diseases of internal organs, which is a contraindication for active immunotherapy, are prescribed antistaphylococcal γ-globulin or antistaphylococcal hyperimmune plasma.
In order to stimulate nonspecific immune factors, autohemotherapy, pyrogenal, prodigiosan, dioxomethyltetrahydropyrimidine, splenin, Chinese Schisandra tincture, Eleutherococcus extract, and blood transfusions are used.
In the treatment of recurrent, persistent pyoderma, immunostimulants are widely used, especially in cases where it is possible to confirm the fact of immune disorders: thymus preparations (thymalin, tactivin, etc.), γ-globulin preparations (intramuscular γ-globulin, etc.), synthetic chemicals (levamisole, diucifon, isoprinosine), sterile filtrate of the culture fluid of some types of spontaneously lysing actinomycetes (actinolysate), azoximer bromide (polyoxidonium). Stimulators of interferon production (sodium oxodihydroacridinyl acetate, meglumine acridone acetate, etc.) are promising. For all chronic, sluggish forms of pyoderma, ascorbic acid and B vitamins and drugs that improve microcirculation (pentoxifylline, xanthinol nicotinate, etc.) are indicated.
For various forms of chronic deep pyoderma (ulcerative-vegetative, gangrenous pyoderma), systemic glucocorticoids (prednisolone 30–60 mg/day, methylprednisolone, betamethasone), cytostatics (azathioprine 150 mg/day, prospidium chloride) are added to antibiotic therapy.
In the treatment of abscessing and undermining Hoffmann's folliculitis, isotretinoin is used at a rate of 0.5–1 mg/kg body weight for several months or a combination of systemic antibiotics and glucocorticoids.
Complex therapy for pyoderma includes physiotherapeutic procedures: ultraviolet irradiation, dry heat, UHF, low-energy laser radiation, wiRA therapy - short-wave infrared radiation filtered through water (780–1400 nm).
Prevention of pyoderma, both primary (in persons without a history of pustular diseases) and secondary, which involves preventing relapses of pyoderma, consists of carrying out certain measures at work and at home.
In production, it is necessary to eliminate factors that lead to violations of sanitary and technical and sanitary-hygienic standards, industrial injuries and microtraumas.
One of the means of combating pyoderma is the timely treatment of microtraumas, for which solutions of aniline dyes, an alcohol solution of iodine, and also a film-forming aerosol nitrofural are used.
It is necessary to treat identified common diseases against which pustular skin lesions may develop (diabetes mellitus, diseases of the digestive tract, ENT organs, etc.).
Secondary prevention of pyoderma includes periodic medical examinations, recording and analysis of morbidity, clinical examination of patients, anti-relapse therapy (staphylococcal toxoid, vitamins, general ultraviolet radiation, skin care, sanitation of focal infection).
Systemic antibacterial drugs
When streptococcus spreads, the risk of developing complications in the form of sore throat, frontal sinusitis, and sinusitis increases. In severe cases, purulent pericarditis develops. That is, bacteria along with toxins accumulate in the pericardial sac, and myocardial damage gradually forms.
To prevent the spread of the microorganism, it is recommended to use systemic medications, that is, those that affect the entire body. They are prescribed after bacteriological culture. The doctor uses a dosage appropriate to the child's weight. This eliminates the risk of severe side effects. The following groups of drugs are recommended:
- penicillins (Amoxicillin, Amoxiclav, Augmentin);
- cephalosporins (Ciprofloxacin, Suprax, Cefuroxime);
- macrolides (Erythromycin, Sumamed, Clarithromycin).
Every day they drink medications that restore the composition of the intestinal microflora (Linex, Normobakt-L are suitable for children). This prevents diarrhea and inflammatory processes on the mucous membrane of the digestive tract. If a child develops adverse reactions, the drug should be discontinued without waiting for addiction.
Taking the medicine orally in the correct dosage will prevent gastritis, exacerbation of ulcers, colitis, and other inflammatory pathologies of the gastrointestinal tract.
If the child has not previously used antimicrobial drugs at the time of treatment, start with the mildest medications. The bacteriological test for the product must be positive.
Analogs
There are several drugs that have a similar effect to Baneocin.
Lincomycin in the form of an ointment copes well with inflammatory processes in the skin. The composition also contains neomycin, which affects aerobic microorganisms.
Bonderm ointment is actively used for various skin diseases. Can be used by adults and children. It is also prescribed to prevent infection of sutures, cuts and wounds after surgery. In rare cases, it leads to allergic reactions and other side effects. Can be used during pregnancy and breastfeeding under medical supervision.
Additional rules for antibiotic therapy
During antibiotic therapy, the patient's condition worsens. This is due to the effect of the active substance on internal organs. It spreads through the systemic bloodstream, penetrating the liver, kidneys, heart, and brain. This not only causes the destruction of bacteria, but also harms your own tissues. Therefore, the following rules must be observed:
- drink still water daily in a ratio of 50 ml of liquid per 1 kg of body;
- the child should sleep at night and have naps during the day;
- take tablets with food to reduce the load on the digestive tract;
- drink kefir, fermented baked milk to replenish destroyed intestinal lactobacilli;
- reduce physical activity;
- use multivitamin complexes to prevent hypovitaminosis;
- if there is no increase in body temperature, walk in the fresh air without contact with other children.
Despite the large number of side effects from drug treatment, antibiotics cannot be avoided. Bacteria are destroyed only by these categories of drugs. If you use only antiseptics or traditional methods, there is a high risk of the pathogenic microorganism spreading into the systemic bloodstream.
Symptoms of streptoderma
The symptoms of streptoderma in children and adults are the same. The duration of the incubation period for streptococcal infection is from 7 to 10 days. Then:
- Round pink spots appear on the skin (most often the face). Their outlines may be regular or irregular.
- After a few days, purulent-vesicular elements form on the surface of the lesions.
- With impetigo, they quickly open and heal. After them, no scars remain on the skin.
- With ecthyma, the germ layer of the skin is damaged, so the formation of permanent scars is possible.
- With shallow skin lesions, temporary hypopigmentation of the skin is possible after recovery.
There are no subjective sensations associated with the disease. In rare cases, patients complain of:
- skin itching;
- dryness of the affected areas;
- headache;
- muscle pain.
With extensive dermatological lesions in children, there may be an increase in body temperature and enlargement of regional lymph nodes.
If the pathological process takes on a diffuse nature, the foci of streptoderma very quickly spread throughout the body, merging with each other, forming larger elements.
Signs of chronic streptoderma
The disease can become chronic:
- overheating, hypothermia;
- phlebeurysm;
- decreased local immunity;
- the presence of open wound surfaces;
- decreased body reactivity;
- constant traumatization of affected areas of the skin (for example, children scratching sores).
Chronic streptoderma manifests itself:
- Large scaly lesions with uneven scalloped edges (diameter about 10 cm).
- Purulent blisters, after opening which form serous-purulent crusts of yellow or brown color.
- When the scabs are removed, an erosive, bright pink surface is exposed.
With a prolonged course, the disease can develop into microbial eczema.
If you experience similar symptoms, consult your doctor
. It is easier to prevent a disease than to deal with the consequences.
Prevention rules
It is easier to eliminate the risk of infection than to treat pathology. If the skin and mucous membranes are heavily colonized, therapy becomes difficult. Therefore, it is recommended to adhere to the following preventive measures:
- daily hygiene procedures that cleanse the epidermis and mucous membranes;
- antiseptic treatment of household items, home furniture;
- timely treatment of infectious pathologies of any location, even if it is simple nasal discharge (most streptococcal infections are localized in the ENT organs);
- use antibiotics only according to the rules;
- the use of antibacterial drugs after passing a bacteriological test, excluding the possibility of using the wrong drugs;
- antiseptic treatment of skin and mucous membranes only in the presence of a bacterial infection, but not for prevention;
- periodic visits to the pediatrician for health checks, which include laboratory tests;
- If rashes appear on the face and other parts of the body, you cannot squeeze them out or eliminate them yourself using other methods, contact a cosmetologist or dermatologist.
Prevention rules will not eliminate the risk of streptococcal infection. It spreads through airborne droplets and household contact from a sick person. Therefore, it is recommended to avoid places with crowded people in the autumn-winter period.
Contraindications and adverse reactions
You should avoid taking Baneocin in the following cases:
- increased susceptibility to constituent components;
- in case of serious skin damage, do not take the drug in the form of an ointment;
- when infected with an infection of the ear canal in the presence of perforating damage to the eardrum;
- for problems with the excretory system;
- for problems with the muscular-nervous system;
- diseases of the visual organs.
You should strictly adhere to the instructions for use and not exceed the permissible dose.
With prolonged use of the product, allergic processes may begin, accompanied by redness, itching and rashes. When treating large skin lesions, systemic negative reactions may occur.
To date, no cases of overdose with Baneocin have been recorded.
Dangers of Streptococcus
Streptococcus is an opportunistic species. If the patient's health is normal, it is present in normal amounts in areas of the body. But under the influence of negative environmental factors, improper treatment, and decreased immune function, bacterial carriage develops.
Hospitalization is not required; treatment of streptoderma in children can be carried out at home, since there is no danger to life during the period of drug use, parents can handle it on their own.
Of particular danger is hemolytic streptococcus, which can cause inflammatory pathologies of internal organs.
If therapy is carried out in a timely manner, the risk of developing a resistant strain of bacteria and its spread to the tonsils, inner ear, pericardium, and genitourinary system is eliminated. The drugs of choice are antibiotics. It is advisable not to use a broad spectrum of action, but to use a medicine to which the microbe is sensitive. Therapy is carried out for 7-10 days, the dose is limited.
What is streptoderma?
Most often, streptoderma occurs in children. The reason for this is the imperfection of the protective function of the skin in childhood and the inability to fully control the child’s hygiene. Outbreaks of streptoderma are not uncommon in closed children's groups and preschool educational institutions. Our portal contains verified pediatric dermatologists and reviews
about them, which will help you choose a good specialist for your child. Streptoderma in adults is a consequence of parental contact with an infected child.
How is streptoderma transmitted?
When answering the question whether streptoderma is contagious or not, it should be noted that infection occurs in two ways:
- contact (direct contact of damaged skin with the skin of a carrier of the disease);
- contact-household (through household items, dishes, toys, towels).
Thus, the disease is contagious.
Classification of streptoderma
According to the nature of its occurrence, streptoderma in children and adults can be:
- primary (streptococci enter the body through damaged areas of the skin, an acute inflammatory process develops);
- secondary (the disease joins an existing streptococcal infection - eczema, chicken pox, herpes simplex virus, etc.).
Foci of streptoderma may appear:
- on the face;
- in the armpits;
- on the skin of the upper and lower extremities;
- on the hands, feet;
- on the folds behind the ears;
- in the groin area;
- in the intergluteal fold;
- in the inframammary folds.
Localization depends on the form of pathology. Dermatologists distinguish the following forms of streptoderma:
- streptococcal impetigo (foci form on the torso, upper and lower extremities, face);
- streptococcal diaper rash (affects the groin area, behind-the-ear folds, intergluteal fold, axillary area);
- bullous impetigo (inflammation occurs on the hands, feet, legs);
- streptococcal ecthyma (inflamed elements appear on the upper and lower extremities, buttocks);
- streptococcal infection (the disease is localized in the corners of the lips);
- tourniol (flaky lesions are diagnosed in the area of the nasal plates).
The spread of streptoderma throughout the body is facilitated by scratching painful areas of the skin, as well as getting water on the lesions (for example, while bathing, swimming in the pool).
![Folliculitis [13]](https://dlradio.ru/wp-content/uploads/follikulit-13-330x140.jpg)