For the first time, it is impossible to take your eyes off your newborn baby. After counting all the fingers and toes several times, the mother notices that the baby has spots on his face, head and body. Immediately after birth, babies often have many spots on their skin. They pass quickly, and those that remain are called moles, or birthmarks.
Not all moles last a lifetime. Some fade over time, but there are also some that remain forever, and sometimes even require medical intervention. After reading this article, you will learn about which birthmarks appear on a child’s body from birth, and which ones appear in later life.
What are moles?
Every child is unique, and every mole is too. From the name you can easily guess that moles are spots that are on the baby’s skin from birth. There is also a theory that identical “marks” on the body were a sign of the same genus. Some moles form before the baby is born and are immediately visible. Others are present on the skin “in theory,” but only appear some time after birth.
Moles can differ significantly from each other in appearance: some can be flat, others can be convex, some can be regular in shape, others can have uneven edges. Colors can vary from yellowish and brown to red and blue.
Most often, moles on the skin are not dangerous. Some even shrink in size or fade completely over time. In rare cases, moles can be a symptom of an underlying disease. In any case, if your baby's moles cause you concern, consult your pediatrician.
Alarm bells or when you need to contact an oncodermatologist
In global oncology practice, there are accepted criteria by which a child’s parents can see signs of the disease and seek advice from a specialist:
- A (asymmetry) – asymmetry . The mole may grow unevenly to the side. It is considered normal that if you draw an imaginary line through the middle of the mole, the halves should be symmetrical.
- B (border irregularity) – uneven, jagged, fuzzy edge.
- C (color) – color. Suspicion of melanoma is caused by changes or heterogeneity in color, the appearance of inclusions.
- D (diameter) – diameter. Increase in size of a common mole.
- E (evolving) – variability of any characteristic: color, shape, size is a reason for immediate consultation with an experienced dermato-oncologist.
Basalioma
Basal cell carcinoma or basal cell carcinoma is more common in adults than in children, but in recent years this pathology has also been diagnosed in adolescents.
A malignant neoplasm forms from the basal layer of the skin epithelium, most often on the face and resembles warts.
Squamous cell skin cancer
This disease is more common in adults. In children, such a tumor looks like a small ulcer that can increase in size and bleed. A tumor can form at the junction of the skin and mucous membranes, for example, on the lips or in the corners of the eyes. In the absence of timely treatment, it metastasizes to nearby tissues and lymph nodes.
Types of moles
The following types of birthmarks are found in newborns:
Pigmented birthmarks. Vascular birthmarks.
Pigmented birthmarks
Pigmented moles are usually brown, yellowish, or gray in color. They form in areas where there is a higher concentration of cells responsible for skin coloring.
Pigmented birthmarks include:
"Coffee" stains. Cutaneous melanocytosis. Nevi (warts).
"Coffee" stains
These are oval, yellowish or light brown (cafe-au-lait) spots that may be present on a child's skin from birth or appear during the first few years of life.
If there are only a few coffee stains, there is no reason to worry. However, if your baby has several spots larger than a 25-cent coin (about 25 millimeters) on his body, it could be a sign of neurofibromatosis, a genetic disorder that causes abnormal growth of nerve cells.
A large “coffee” spot with jagged edges sometimes indicates the presence of a rare hereditary disease called McCune-Albright-Braitsev syndrome.
At the slightest suspicion, we advise you to show the baby’s moles to a pediatrician and, possibly, a dermatologist and geneticist.
Cutaneous melanocytosis (“Mongolian” spots)
The so-called “Mongoloid” spots are flat moles of various sizes, brown, gray and even bluish in color.
Areas of cutaneous melanocytosis are usually located in the lower back or on the baby’s buttocks. Such birthmarks are very common in dark-skinned, Mongoloid babies. Usually these spots fade before school age.
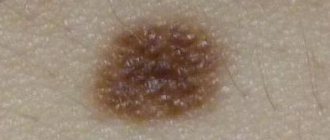
Nevi
Nevi can be either congenital or acquired. Nevi can grow with the child.
The color of nevi varies from yellowish to black. This is a relatively common occurrence - about 1 percent of all newborns are born with nevi.
As a rule, nevi are not dangerous and are benign skin formations, but sometimes after a long enough time they can turn into a malignant skin tumor (melanoma). It is recommended to periodically show the baby's pigment elements to the pediatrician. If the size of the wart has changed, be sure to tell your doctor about it.
In extremely rare cases (1 in 20,000 children), a nevus can grow to a size of over 20 centimeters in diameter. Such nevi can be either flat or convex, and hair can grow on them. Consult a doctor - he will conduct an examination and advise what to do in this case.
Vascular birthmarks
Vascular birthmarks are collections of blood vessels. For this reason, such spots may be red or even purple.
These spots can be either flat or convex in shape. The following types of vascular birthmarks are distinguished:
Infantile hemangioma. Simple nevus. "Wine" stains.
Infantile hemangioma (“Strawberry” spots)
So-called “strawberry” spots, or hemangiomas, are collections of small blood vessels under the skin.
Usually these spots are not visible immediately after birth. In the first weeks they may be flesh-colored or even white, and only turn red later. "Strawberry" spots occur in 10 percent of babies aged 2 months, most often appearing by 2-3 weeks.
Such spots can appear on any part of the skin, but, as a rule, they are concentrated on the head or neck. They are more common in Caucasians, female babies, twins, premature babies and low birth weight babies.
Hemangiomas often grow with the baby and reach their largest size by three or four months of age. These spots gradually disappear by school age.
If your baby’s hemangioma worries you, grows too quickly, begins to bleed, or bothers your child, then let a doctor examine it. Typically, hemangiomas do not require treatment and are self-necrotic, but they are sometimes removed if they are causing serious problems, such as being located near a child's eye, in the mouth or throat. They are also removed if there is bleeding or infection.
Most often, hemangioma is single. In rare cases, a child may have several hundred small hemangiomas throughout the body. Sometimes hemangioma lies in the deep layers of the skin.
In the latter case, local treatment, oral medications, injections, laser treatment or surgery are prescribed. Discuss all your options with your doctor.
Simple nevus
Popularly, these pink spots on a child's neck, forehead, upper eyelids, nose or upper lip are called "salmon" spots, "stork bites" and "angel kisses".
Such spots are very common - in more than 80 percent of babies, most often in fair-skinned children. As a rule, they merge with the skin after a few years.
Wine stains
These are large, flat, uneven patches of dark red or purple color on a child's face or neck. They appear due to disturbances in the development of blood vessels under a specific area of the skin. Such spots do not disappear, but, on the contrary, darken over time. Port-wine stains do not go away on their own and require treatment.
To reduce the likelihood of darkening of port-wine stains during adolescence and adulthood, pulsed dye laser treatment is sometimes prescribed to young children. We recommend discussing all possible treatment options with your doctor.
If a port-wine stain is located near the eye, forehead, or scalp, it may indicate an eye and brain disorder called Sturge-Weber disease. This very rare neurological disease causes glaucoma, seizures, developmental delays and learning delays.
The pediatrician will be able to make the correct diagnosis and prescribe the appropriate treatment, including laser lightening of the spot.
Why does skin cancer occur?
There are a number of reasons that provoke the development of a skin tumor in a child:
- aggressive exposure to sunlight (staying on the beach at the wrong time, sunburn, etc.)
- hereditary predisposition - cases of skin cancer in close relatives
- endocrine system diseases
- increased sensitivity to ultraviolet radiation
- Skin phenotype 1 and 2 - children with fair skin, blond or red hair, blue or gray eyes and freckles
Diagnosis of skin cancer
Diagnosis in our clinic is carried out by experienced dermatologists-oncologists. After which the following can be prescribed:
Dermatoscopy - “surface microscopy” - is the study of altered areas of the skin using a high-precision optical system - a dermatoscope. The tool allows you to enlarge the inspected area several times.
The Melanoma Unit uses a manual Heine Delta 20 device and a unique, only in Russia, digital device FotoFinder Master. The advantages of digital diagnostics are the objectivity of the assessment of the data obtained. An automated dermatoscope allows you to analyze skin tumors digitally, taking the visualization of skin cancer to a new level.
A tumor biopsy is the removal of a piece of pathological tissue for subsequent histology - examination under a microscope, which allows one to establish the nature of the formation and confirm or refute the primary diagnosis. The histological material is examined by the most experienced specialists in Moscow in the Melanoma Unit partner laboratory. In complex cases or at the request of the patient’s parents, we can send histological material for analysis to our head center in Israel - to our own Prime Pathology laboratory. When the diagnosis of melanoma is confirmed, its thickness is determined using a special device.
Treatment of skin cancer in children
Oncologists use surgery, chemotherapy, hormonal therapy, immunotherapy, and targeted drugs to treat this disease.
Surgical intervention
During the operation, the surgeon removes the tumor and healthy tissue no more than 1-2 mm around it. Often the effect of surgical treatment is consolidated with chemotherapy.
Immunotherapy
Drug treatment of melanoma aimed at stimulating one's own antitumor immune response . This therapy does not directly affect the tumor; it works indirectly through the immune system.
The following can be used in treatment:
● cytokines
● vaccine therapy
● mononuclear antibodies
Chemotherapy
This treatment is based on the use of cytostatics that “destroy” cancer cells.
Radiation therapy
Treatment based on the use of a special type of electromagnetic radiation energy or particle beams that can kill or inhibit the growth of tumor cells.
Targeted therapy
Specially selected agents specifically target the tumor target cells of a particular patient, without affecting healthy tissue.
How to prevent skin cancer in children?
To reduce the risk of melanoma and other types of skin tumors, it is recommended:
- limit the child’s time in direct sunlight during periods of special activity - from 11 a.m. to 4 p.m.
- Use high-quality sunscreen with a high SPF level, as well as hats, sunglasses and loose clothing in light colors
- carry out skin examinations in children both independently and in a dermatologist’s office (if there are a large number of nevi or a family history)