05/24/2018 Many people who discover a spot under their nail begin to search on the Internet to find out what it could be? And it turns out that this can be a fatal disease - subungual melanoma.
In this article we will look at:
- concept of subungual melanoma;
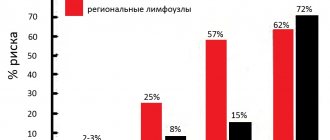
- the chances of this type of tumor occurring;
- photos of symptoms with histological confirmation;
- ways to distinguish subungual melanoma from hematoma;
- procedures to clarify the diagnosis;
- prognosis and treatment.
Subungual melanoma – what is it?
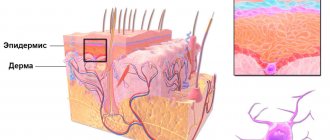
The share of melanoma among skin tumors is only 4%. But it is from this malignant neoplasm that 80% of patients with skin tumors die [1]. In Russia, about 8,717 people a year currently develop skin melanoma (data for 2012) [2]. Subungual melanoma is located in the nail bed and usually appears as a stripe on the nail.
Sign up for the webinar “Carcinogens in cosmetics: truth, lies and... marketing”
Complications
Subungual melanoma is characterized by an aggressive course. This is one of the most aggressive forms of this disease. Radical surgery for an invasive tumor does not guarantee complete cure and prevention of relapses or the development of metastases. Most often, metastases are found in the lungs and liver, and their degree of malignancy exceeds the primary tumor. As the process develops, general complications characteristic of malignant neoplasms arise: weakness, anemia, cachexia, etc.
It must be taken into account that surgical removal of the primary focus of melanoma leads to partial loss of function of the affected limb. During surgery, a visible defect is formed on the hand, which is almost impossible to hide from others, plus the functionality of the hand is impaired.
In some cases, foot surgery requires resection of the metatarsus. This greatly reduces the support of the operated leg and creates additional stress on other parts of the musculoskeletal system, leading to the development of arthrosis, myositis, muscle spasms and other disorders.
What are the chances of this type of tumor occurring in a resident of Russia?
Of the total number of melanomas, the share of this tumor is only 2% [3], i.e., in absolute values, in 170 people per year. Against the background of the country's total population of 146,000,000, this, in my opinion, is very small. At the same time, a low incidence rate does not eliminate the possibility of getting sick.
For representatives of other skin phototypes other than 2, the chances may be very different. Representatives of the Mongoloid and Negroid races have a higher (up to 40%) chance of developing melanoma of the nail bed [4, 5].
Where does subungual melanoma appear most often?
The tumor most often affects the big toes [3].
At-risk groups
The diagnosis of subungual melanoma is made in most cases to people predisposed to the disease. Risk factors are observed in groups:
- with hereditary characteristics,
- fair-haired, pale-skinned from birth,
- after sunburn,
- fans of solariums,
- age representatives of the male and female half.
“At the age of forty we are faced with a choice: either to extend our Youth, or to extend our Life...” - Jacques Deval.
Those who fall into one of the categories should carefully examine their fingers. If symptoms are detected, even if there is doubt, subungual melanoma is excluded by the results of the examination.
What does subungual melanoma look like? Photos and signs.
All pictures below are histologically confirmed and not taken from the Internet. The source is indicated in square brackets. There are 2 most common signs:
Sign I
Most often, subungual melanoma appears as a brown or black stripe. The strip starts from the nail fold and ends at the edge of the nail. This condition is called longitudinal melanonychia. Some medications can cause such bands to appear - retinoids and Docetaxel (Taxotere) [10]. This sign can also occur in conditions not associated with melanoma, for example, with fungal infection of the nail, pigmented nevus of the nail bed.
Subungual pigmented nevus in a 13-year-old boy [9]
Subungual melanoma stage I, 0.2 mm according to Breslow [10]
Sign II
The most common sign of this type of melanoma is Hutchinson's sign - a transition of pigmentation to the nail fold or fingertip. This feature is visible in 7 of the 8 images below. At the same time, it cannot be stated unequivocally that this symptom occurs only with melanoma. It can also be observed with a transparent cuticle [10].
8 cases of subungual melanomas in situ (initial stage) [6]
Subungual melanoma of the thumb with level 4 invasion according to Clark, thickness according to Breslow is not specified [8]
Subungual melanoma, Breslow thickness 1.5 mm [7]
No confirmations
None of the experts interviewed by a Rosbalt correspondent confirmed that there is a direct or indirect connection between gel polish and subungual melanoma. Thus, oncologist Grigory Zinoviev refuted this assumption:
“There are no statistically reliable studies showing a relationship between shellac and acral melanoma. If the light source in the technology for applying gel polishes is an LED lamp, and not an ultraviolet lamp, as, for example, in a solarium, this procedure should not affect the likelihood of melanoma.”
38478
“Oncological disease is a 100% crisis in the family”
Elena Likhova, a master at a federal network of manicure and pedicure salons, shares the same opinion: according to her, LED lamps have been used in the industry for a long time.
“The LED lamp cannot provoke the growth of cancer cells and hyperpigmentation of the skin. Light is different from ultraviolet radiation, which we are exposed to in direct sunlight. Curing lamps are safe; they only speed up the hardening process of the polymer coating,” Likhova noted.
Manicurist Tatyana Smirnova notes that even old UV lamps operated at a power of only 9 watts, which is not enough for serious consequences:
“This is a very low power, and the client held his hands directly in the lamp for a maximum of 15-20 minutes once a month. For comparison, solarium lamps have a minimum power of 180 watts or more.”
Elena Likhova suggested that anyone in doubt apply sunscreen to their hands immediately before applying it or use special manicure gloves that only expose their nails. But you should pay closer attention to the composition of gel polish.
“At a minimum, the composition should be 3FREE and not contain toluene, formaldehyde and dibutyl phthalate, parabens and camphor. In principle, now all normal manufacturers have already removed this from their formulations, so if you use proven brands, no consequences will arise,” says the master.
Tatyana Smirnova agrees with her, noting that for most modern materials that are sold in stores and have a quality certificate, the raw materials are purchased from factories in Europe. However, you can find many fakes on the Internet, which can contain anything. It is also worth paying attention to the professionalism of the master: if he did not properly remove the coating with the device or applied a lot of material to the nail, this can lead to burns, onycholysis, cuts and damage.
17639
Hit below the belt
How to distinguish subungual melanoma from everything else?
Here is a fairly simple algorithm.
Algorithm for the differential diagnosis of benign melanonychia and the same condition in melanoma [8]
ABCDEF rule for diagnosing nail bed melanoma
And (age) age - the peak incidence of subungual melanoma occurs between the ages of 50 and 70 years, and also denotes races with an increased risk: Asians, Africans - they account for 1/3 of all melanoma cases.
B (brown to black) – the color is brown and black, with a stripe width of more than 3 mm and blurry boundaries.
C (change) – change in the color of the nail plate or no change after treatment. D (digit) – finger as the most common site of injury.
E (extension) - spread of pigmentation to the nail fold or fingertip (Hutchinson's symptom).
F (Family) – relatives or the patient have a history of melanoma or dysplastic nevus syndrome. [eleven]
How to distinguish a hematoma from a subungual melanoma by dermatoscopy
Hematoma: [10]
- It moves under the nail along with its growth. You can track this by taking a photo of the formation against the background of a ruler located longitudinally. It is important to note that a hematoma does not always appear due to trauma.
- Color from red-blue to black-blue.
- Does not transfer to the cuticle, nail fold and fingertip.
- Does not involve the entire nail in the longitudinal direction.
- May change within a few weeks.
- The color intensity decreases from the center to the periphery.
- It may be preceded by trauma.
- Small blood spots oriented towards the edge of the nail on dermatoscopy
Subungual melanoma: [12]
- Heterogeneous color, irregular stripes with melanonychia.
- Triangular stripes.
- Spreads on the nail plate, free edge of the nail or fingertip.
- Destruction or dystrophy of the nail.
Diagnostic methods
Subungual melanoma belongs to tumors of external localization, however, timely diagnosis can be difficult due to the similarity of the clinical picture with nevi, subungual hematomas and hemangiomas. To differentiate the nature of the neoplasm, special dermatological research methods are used:
- Dermatoscopy is a visual assessment of pathologically changed tissues using multiple magnification.
- Epiluminescent microscopy is a dermoscopic examination of pathologically altered tissues in an immersion environment. This technique makes it possible to differentiate a benign neoplasm from a malignant one with a high degree of probability.
If there are changes in the nail plate, a cytological examination of fingerprint smears can be performed. The final diagnosis is made after a histological conclusion. In the case of melanoma, taking a biopsy is strictly not recommended, so as not to provoke metastasis. Therefore, the study is carried out after radical surgery.
If within two months after the patient’s request it is impossible to exclude subungual melanoma, marginal resection of the nail plate with matrixectomy is performed, followed by histological examination of the resulting material. If the diagnosis is confirmed, radical surgery is indicated.
To determine the stage of the disease, radiation methods (ultrasound, CT or MRI) are used, which make it possible to determine the presence of local and distant metastases.
Bibliography
- Miller AJ, Mihm MC. Melanoma. N Engl J Med. 2006; 355:51-65.
- Data from the Globocan 2012 study, International Agency for Research on Cancer (IARC): https://gco.iarc.fr/today/online-analysis-multi-bars?mode=cancer&mode_population=hdi&population=643&sex=0&cancer=29&type=0&statistic=0&prevalence= 0&color_palette=default
- Kuchelmeister C, Schaumburg-Lever G, Garbe C. Acral cutaneous melanoma in caucasians: clinical features, histopathology and prognosis in 112 patients // J. Dermatol. – 2000
- Takematsu H, Obata M, Tomita Y. Subungual melanoma. A clinicopathologic study of 16 Japanese cases // Cancer. – 1985
- Wu XC, Eide MJ, King J. Racial and ethnic variations in incidence and survival of cutaneous melanoma in the United States, 1999–2006 // J. Am. Acad. Dermatol. – 2011.
- Jae Ho Lee, Ji-Hye Park, Jong Hee Lee, Dong-Youn Lee. Early Detection of Subungual Melanoma In Situ: Proposal of ABCD Strategy in Clinical Practice Based on Case Series Ann Dermatol. Feb 2022; 30(1): 36–40.
- Stephan Braun, MD and Peter Gerber, MD. Subungual malignant melanoma. CMAJ. 2015 Sep 8; 187(12): 909.
- Pierre Halteh, Richard Scher, MD, FACP, Amanda Artis, MS, MPH, and Shari R. Lipner, MD, PhD. A Survey Based Study of Management of Longitudinal Melanonychia Amongst Attending and Resident Dermatologists. J Am Acad Dermatol. May 2022; 76(5): 994–996.
- Kamran Khan and Arun A Mavanur. Longitudinal melanonychia. BMJ Case Rep. 2015; 2015: bcr2015213459.
- Holger A. Haenssle, Andreas Blum, Rainer Hofmann-Wellenhof, Juergen Kreusch, Wilhelm Stolz, Giuseppe Argenziano, Iris Zalaudek, and Franziska Brehmer. When all you have is a dermatoscope— start looking at the nails. Dermatol Pract Concept. 2014 Oct; 4(4): 11–20.
- Levit EK, Kagen MH, Scher RK, Grossman M, Altman E. The ABC rule for clinical detection of subungual melanoma. J Am Acad Dermatol. 2000 Feb;42(2 Pt 1):269-74.
- Haenssle HA, Brehmer F, Zalaudek I, Hofmann-Wellenhof R, Kreusch J, Stolz W, Argenziano G, Blum A. Dermoscopy of nails. Hautarzt. 2014 Apr;65(4):301-11. doi: 10.1007/s00105-013-2707-x.
Reasons for appearance
Any neoplasm has a cause that affects its activation. The target is the nail. The basis for its origin is considered to be:
- living in a poor environmental climate,
- consumption of modified, low-quality products,
- relationship with harmful carcinogenic substances,
- bad habits (often cheap alcoholic drinks, tobacco),
- nail injuries,
- signs of one of the risk groups.
A healthy cell, according to the conclusions of modern scientists, mutates, changing the number of genes, and is rebuilt with a violation of its usual integrity. Changes in DNA, enzymes, and genes provoke factors that cause the occurrence of nail melanoma.
Prevention of cancer
The main preventive measure is a preventive examination. It is necessary to undergo it at least once a year. Early detection of diseases is the main task of any person.
To maintain health, follow these simple recommendations:
- adhere to a nutritional culture: a balanced menu, the absence of genetically modified products oversaturated with chemicals in the diet,
- Quit smoking and alcohol abuse. Particularly harmful are low-quality products containing high levels of carcinogens.
- Protect the purity of intimate relationships. Be selective in sexual relations, maintain hygiene, use protection during sexual intercourse,
- Living in an area with high environmental pollution, go to the sea more often, not necessarily in the summer, and use sanatoriums and health services in resort areas. Don't be in the open sun
- having a history of hereditary predisposition, examine yourself more carefully, undergo laboratory examination,
- Load your body with physical exercise. Play sports, saturating the body with oxygen, activating the work of all organs, improving blood circulation,
- Strengthen the immune system, the best barrier to viruses and bacteria. The body is a wise and complex apparatus, capable of redistributing forces with a healthy immune system,
- monitor hormonal levels so that a lesion does not form due to pathology of the endocrine system.
Annual statistics record an increase in malignant diseases. It is unrealistic to exclude a sad diagnosis, but everyone can reduce the risk by protecting their body. Now you know what subungual melanoma is and how to treat it.