Melanoma is one of the most dangerous malignant diseases.
Detection of a tumor at an early stage makes it possible to cure it radically surgically. When melanoma is widespread and has distant metastases throughout the body, treatment options are limited.
The incidence of melanoma is growing, and although melanoma accounts for only 4% of all cancers, it accounts for 80% of deaths from skin cancer. Compared with primary lung, breast, kidney, or colorectal cancer, melanoma has the highest propensity to metastasize.
The main cause of death in patients with melanoma is widespread metastases.
Melanoma stages take into account four main indicators:
- tumor thickness;
- ulceration;
- degree of lymph node damage;
- presence of isolated metastases.
Metastases in melanoma
Lymph circulation and chemotaxis are responsible for homing melanoma cells to a variety of locations. Metastases develop in regional lymph nodes as satellite or transient lesions, as well as in the form of tumors in distant organs.
In 2/3 of patients, the first metastases are localized, in 1/3 there is damage to distant organs.
Based on the nature of their spread, local metastases can be grouped:
- local recurrence: recurrence of the scar after the primary operation;
- “en route” metastases: metastases that spread along the lymphatic tract between the primary tumor >2 cm from the scar and regional lymph nodes;
- satellite tumors: new formations within a radius of 2 cm from the scar after removal of the primary tumor; these satellites may be caused by remnants of the primary melanoma.
The presence of satellites and metastases “en route” should raise suspicion regarding distant metastases.
Pigmented tumor can metastasize to almost all areas of the body. 1/3 of patients have distant metastases of melanoma without intermediate spread to regional lymph nodes.
Metastases in malignant melanoma can spread lymphogenously and hematogenously.
The most common metastatic sites:
- leather;
- The lymph nodes;
- lungs;
- liver;
- bones;
- brain and spinal cord.
The first metastases of melanoma usually appear in the skin or lymph nodes, but metastases to the lungs, liver and brain are the most common causes of death in patients. Metastasis pathways have a certain dependence on the location of the primary tumor.
For example, mucosal melanoma usually metastasizes to the liver, lungs, brain and dermis; Local tumor growth can be extensive, with bone destruction and sinus involvement, and local recurrence is very common. In melanomas of the oral cavity, metastases are more common than in malignant melanomas of the accessory sinuses.
In ocular melanoma, metastases almost always spread hematogenously, since the eye does not have a lymphatic drainage system.
In 10–12% of cases, at the time of diagnosis, there are already metastases in the lymph nodes; in 25%, metastases develop in the lymph nodes during the course of the disease. In more than 90% of patients, liver metastases are the first sign of disease spread.
Principle and routes of metastasis
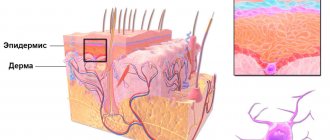
The process of the appearance of secondary foci of neoplasms is very complex and has not been fully studied. It is assumed that the cause of metastasis is a disruption in the interaction between atypical cells of the primary tumor, the extracellular matrix and normal cells. Several proteolytic enzymes have been discovered that trigger the degradation of the extracellular matrix and improve the adhesion of cancer cells, which allows them to move throughout the body and invade any tissue. Vascular endothelial growth factor plays an important role in the growth of secondary tumors, which stimulates the formation of new vessels, which subsequently feed the tumor. The spread of melanoma metastases usually occurs through the lymphatic and blood vessels. Most often, secondary lesions appear in the lymph nodes, skin and subcutaneous tissue, bones, liver, lungs, and brain.
Metastases to the brain
More than a third of patients with metastatic melanoma develop brain metastases. Based on autopsy results, the frequency of metastases at this location reaches 75%, while when the initial diagnosis of melanoma is made, only 7% of patients have metastases in the brain. This indicates that in most cases, secondary metastatic damage to the central nervous system develops during the course of the disease.
Metastatic brain damage may be accompanied by:
- the formation of large (more than 4 cm) metastases;
- small disseminated tumors;
- secondary tumor hemorrhages into brain tissue.
The symptoms that arise in this case are in most cases not specific and are determined by the location of the lesion. Brain metastases from melanoma can cause the following symptoms:
- headache, often paroxysmal;
- unilateral paralysis of the body;
- visual impairment, etc.
Among patients with brain metastases, the prognosis is always very serious and varies greatly depending on the extent of the damage and the patient's condition.
Comment from a doctor at the oncology center:
– Melanoma affects even young people. The lighter your eyes and skin, the more easily you burn in the sun, the more difficult it is for you to tan, the higher your risk of developing melanocytic skin cancer. Yet melanomas occur even in people with dark skin color.
On average, 1 in 5 people will be diagnosed with melanoma during their lifetime. Skin cancer cannot be guaranteed to be avoided, but the likelihood of developing a tumor can be reduced. Wear thick clothes with sleeves. Try not to walk outside in the middle of the day, during peak solar activity. Use sunscreen regularly. All of this will help you reduce your risk of skin cancer.
Women between the ages of 20 and 30 often come to us, so Christina’s case is not an exception to the rule. I told this girl the following: if you have already had melanoma, then your risk of developing a second such tumor throughout your life is 10-20%. For this reason, every 4-6 months you need to undergo a preventive examination by a dermatologist. If a second melanoma does appear, it must be detected as early as possible.
Find out if the treatment is prescribed correctly
Early detection of melanoma is the key to reducing mortality rates. Melanomas are perhaps the most obvious cancers. If detected early and treated immediately, they pose no real threat. But once melanoma metastasizes, no therapy is effective.
If melanoma is detected early, it can be cured with 100% probability. That's why you need to go to a dermatologist as soon as you notice a suspicious growth on the skin.
Metastases to the lungs
Treatment of metastatic melanoma in Israel is carried out only after an accurate diagnosis of the disease has been established, including a revision of histology and immunohistochemical tests.
Israeli clinics have unique equipment that allows them to detect microscopic foci of metastasis, accurately determine the genetic form of the disease (on the basis of which certain medications are prescribed) and determine the aggressiveness of the process.
To treat metastatic melanoma in Israel, both immunotherapy and the effect of inhibitors on tumor cells in combination with biological methods are used. When prescribing a treatment program, the form of melanoma, the prevalence of the tumor process, as well as the general condition of the patient’s body are taken into account.
Modern medicine, even in the most advanced cases of metastatic melanoma, is able to stop the development of the tumor process, significantly reduce tumor intoxication, relieve pain, prolong the patient’s life and improve its quality.
Below are the types of treatments for metastatic melanoma.
How does the quality of drugs affect the cure for melanoma?
Current treatment for advanced melanoma often includes targeted and immune-based drugs. Their cost is usually quite high, so it is important that the authenticity and high quality of these medicines are guaranteed. This is why they are worth purchasing in Israel:
- Israeli drugs are reliably protected from counterfeiting. The guarantor of the authenticity and high quality of medicines in Israel is the Ministry of Health, which exercises strict control over the production and sale of medicines.
- New medicines are being rapidly introduced in Israel. In this country, approval of a drug does not require a lengthy bureaucratic procedure.
- The Israeli pharmaceutical company TEVA is one of the most advanced in the world. Medicines from this company are prescribed in 60 countries.
Liver metastases
The spread of melanoma cells to the liver leads to the formation of metastases. Changes are happening quite quickly. Secondary liver damage can be represented by a single metastatic focus, as well as multiple disseminated forms. Clinical manifestations of melanoma metastases to the liver will depend on the volume and location of the process. Symptoms are presented:
- pain in the right abdomen;
- yellowness of the skin and mucous membranes;
- tuberous compaction in the right hypochondrium;
- loss of appetite;
- significant weight loss;
- nosebleeds.
In this case, there is a significant increase in the volume of the liver and spleen, and the biochemical composition of the blood changes.
Characteristics of metastatic melanoma
Characteristics of advanced metastatic melanoma include:
- location of distant metastases;
- number and size of tumors;
- an increase in the level of lactate dehydrogenase (LDH) in the blood serum, which usually indicates the spread of the tumor to internal organs.
There are three subclasses of metastatic melanoma. This division is based on the location of metastases and LDH levels:
- M1a:
the tumor metastasizes to a distant area of the skin, subcutaneous tissue or distant lymph nodes; LDH is normal. - M1b:
tumor metastasizes to the lungs; LDH is normal. - M1c:
tumor has metastasized to organs other than the lungs, LDH is normal, or there are any distant metastases with elevated LDH levels.
Melanoma with metastases: prognosis
Why is it important to know the location of metastases? Large-scale studies have shown that survival rates for advanced melanoma are directly related to the location of metastases, which determines the further prognosis of the disease:
| Localization of metastases | Survival periods | ||
| 1 year | 2 years | 5 years | |
| Skin, soft tissue and/or lymph nodes | 62% | 43% | 28% |
| Lungs | 53% | 31% | 15% |
| Visceral organs | 33% | 18% | 9% |
Risk groups and factors predisposing to the development of skin melanoma.
Individuals at increased risk of developing melanoma include:
- with white skin, red hair, blue, gray or green eyes;
- constantly sunburned;
- those who have suffered sunburn and have been exposed to the sun for a long time, especially under the age of 20;
- having close relatives with melanoma (other skin cancer);
- having more than 100 moles on the body or more than 50 before the age of 20;
- having Dubreuil's melanosis (precancerous skin disease).
There are well-known cases of melanoma being diagnosed after injury to a pigmented nevus of the skin (mole). Melanoma often occurs after accidental or intentional (cutting, burning) injury to a mole. Sometimes 1-2 injuries are enough for melanoma to occur.
Trauma to the nevus can be chronic and occur unnoticed. For example, a well-starched shirt collar can injure moles on the neck, and bras can injure moles on the torso. Moles localized on the soles of the feet, palms, and perineum are chronically injured.
The influence of certain hormones on the development and clinical course of melanoma is assumed. Puberty, pregnancy and menopausal changes are regarded as risk factors for the development of melanoma from pigmented nevi.
Genetic predisposition plays a role (familial cases of melanoma).
Melanoma with metastases: treatment
Various methods are used to treat metastatic melanomas in modern oncology:
Surgical method
For melanoma with metastases, surgical treatment is possible only in cases where it is necessary to relieve the patient of pathological symptoms, as well as for single tumors of visceral organs with a relatively satisfactory general condition of the patient (for example, with single metastases in the liver or lung).
Sometimes surgical treatment can be used in the presence of single lesions, if antitumor therapy has led to a significant reduction in the volume of the metastatic tumor.
After decades of research, promising therapies have emerged that offer hope of extending patients' lives and, in some cases, even providing a cure. We are talking about immunotherapy and targeted therapy for metastatic tumors.
Immunotherapy
Immunotherapy in oncology is a collective concept that involves the use of a wide arsenal of antitumor drugs:
KEYTRUDA (pembrolizumab), OPDIVO (nivolumab) are designed to block a cellular target known as PD-1, which limits the body's immune system from attacking melanoma cells. When using drugs, the body's immune system's ability to fight metastatic tumor tissue increases.
YERVOY (ipilimumab) is an anti-CTLA-4 monoclonal antibody to restore and strengthen the immune system by supporting T cell activation and proliferation.
PROLEKIN / IL-2 (interleukin-2) is intended to restore and strengthen the immune system. Using the drug shrinks tumors in about 16% of patients, of whom 6% have long-term responses.
IMLYGIC (talimogene laherparepvec "T-Vec") is a genetically modified live oncolytic herpes virus designed to replicate in cancer cells and produce an immune-stimulating protein called GM-CSF (granulocyte-macrophage colony-stimulating factor). 16.3% of patients receiving Imlygic experienced a reduction in the size of secondary skin lesions and lymph nodes.
Targeted therapy
COTELLIC (cobimetinib) and ZELBORAF (vemurafenib) in combination work to inhibit the growth of metastatic melanoma.
MEKINIST (trametinib) and TAFINLAR (dabrafenib) in patients with a BRAF mutation Tafinlar in combination with Trametinib blocks a cellular pathway to inhibit the growth of melanoma metastases. The drugs Braftovi (Encorafenib), Mektovi (Binimetinib) and Erivedge (Vismodegib) work in a similar way.
ZELBORAF (vemurafenib) . The BRAF protein is normally involved in regulating cell growth, but is mutated in about half of patients with advanced melanoma. Vemurafenib and dabrafenib interfere with the function of the V600E mutant BRAF protein gene.