Melanoma is a malignant disease that affects the pigment cells of the skin - melanocytes. Studies have shown that the incidence of skin cancer has been steadily increasing in recent years. Among many types of skin cancer, melanoma causes changes in pigment cells. Although the disease is mainly observed on the skin, the painful process can also affect the mucous membranes, or, for example, the eyeball.
Cause of melanoma
The content of the article
The causes of melanoma can be different. Scientists include genetic and environmental factors among them. It is estimated that up to 10% of cases of the disease are associated with genetic complications. It is therefore recommended that the next of kin (for first degree relatives) of the patient undergo dermatological consultation and monitoring.
Environmental factors are also of great importance, among which sunbathing and associated skin burns stand out first.
Skin burn from sunbathing
Melanocytic changes can also cause melanoma. They usually appear on the skin as small nevi. They can be congenital or acquired. However, assessing the change, whether it is just a harmless mole or cancer, is based on additional diagnostic tests.
Almost everyone is at risk of developing this disease because we are exposed to sunlight every day, which is a very important factor in the development of melanoma. Therefore, it is very important to regularly examine moles yourself and have an annual examination with a dermatologist. A timely removed mole will save you from painful procedures and difficult operations.
Melanoma symptoms
Symptoms of melanoma include new-onset skin lesions or those that arise from a pre-existing pigmented nevus (mole):
- It is often observed that in the immediate vicinity of these lesions thickenings form, changes in the existing surface, color and changes at the edges of the mole.
- You should also be concerned about sudden itching or the appearance of bleeding or bloody discharge.
- An inflammatory reaction associated with a mole is also a warning sign of melanoma.
- One symptom to look out for is blue and black moles. The occurrence of this type of pigmentation should be resolved as soon as possible by consulting a doctor.
For early diagnosis of melanoma, monitoring changes in moles, carried out by the patient individually, is of great importance.
If there have always been pigment changes on the skin, the following should alert you:
- sudden itching;
- bleeding;
- increase in lesion;
- changes in the structure of the mole.
Particularly noteworthy is the fact of uneven pigmentation, which contains various shades of brown and pink. It is also worth paying attention to the new changes.
How to recognize melanoma?
To diagnose melanoma, it is necessary to carry out very extensive diagnostics. Of course, the basis is the medical interview conducted during the first visit. The information obtained from the patient concerns mainly information about the condition of the skin, with particular emphasis on changes in moles on the skin or the appearance of new ones.
Information regarding factors that have been identified as increasing the risk of melanoma is also very important to the dermatologist. This group usually includes sunburn or the use of tanning beds. It is also very important for the doctor whether there have been cases of skin melanoma in the patient’s family.
An in-depth interview is the basis for further action. The most important element of diagnosis is the skin examination, which the dermatologist performs during the visit.
Causes and risk factors
Melanoma develops due to malignancy (malignant degeneration) of melanocytes. No reliable causes of cell degeneration have been identified; every person is at risk of the disease. Factors that increase the risk of tumor development:
- hereditary predisposition;
- Phototypes I and II – fair skin, hair and eyes, pink freckles;
- multiple moles, age spots;
- excessive ultraviolet radiation - both natural and in a solarium;
- age over 50 years;
- endocrine diseases;
- previous melanoma.
The combination of any three of these factors is a reason for regular preventive visits to a dermatologist.
Dermatoscopy
Dermatoscopy is an examination in which a dermatologist uses a dermatoscope. This is an instrument that combines a magnifying glass 10 or 20 times, magnifying the fragment under study, equipped with a standardized light source. In such conditions, the doctor may initially assess skin changes.
Dermatoscopy
Videodermatoscopy is a study that, in addition to the techniques used in dermatoscopy, uses visualization on a computer monitor. This allows the clinician to store the displayed image in the device's memory, which can be useful for comparative purposes at a later stage in treatment. In practice, several dermoscopic methods are used to diagnose melanoma.
The doctor, based on the appearance of the lesion, will evaluate whether there is a reason to remove it along with a margin of healthy skin, and send the material after the procedure for histopathological examination.
The specialist studies the characteristic features of the mole, in particular:
- Color—uneven color, darker and lighter areas, or pink and red areas are abnormal;
- Ragged edges - moles with smooth edges are less dangerous to health;
- Asymmetrical shape;
- Size greater than 5 mm - smaller lesions are usually not a cause for concern, but if they are growing dynamically or show other abnormalities, they need to be removed;
- Bleeding, ulceration, presence of discharge.
Diagnosis that confirms or excludes a skin neoplasm, which is melanoma, is possible on the basis of a histopathological examination, which is carried out after removal of the entire lesion.
Types of melanoma
Skin lesions diagnosed as melanoma do not always look the same. Thus, there are several types of melanomas, which define different clinical subtypes of the disease.
- Superficial melanoma
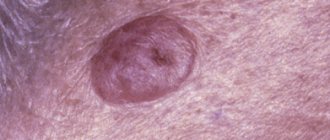
. It is indicated that the most common type of melanoma, which accounts for up to 60-70% of all cases of the disease, is superficial melanoma. This group of melanomas is most often based on pigmented lesions of a dysplastic nature. - Nodular melanoma
. Indicated as the most severe form of the disease, affecting 10-30% of patients. This group, in turn, includes two clinical subtypes. The first is lentiginous melanoma, which is a malignant form. Occurs in 5-15% of cases. It most often affects older people, especially in the neck or face. Lentiginous melanoma is caused by prolonged and prolonged exposure of the skin to sunlight. The second subtype is acral melanoma, which is observed on the inner surface of the skin of the arms and legs. - Colorless melanoma
. The disease also includes pigmented melanoma. Only 2% of patients suffer from it. This is a characteristic type of skin lesion in which pigment is absent. In this case, the symptoms are also quite specific, and the not very characteristic but enlarging pink-red papule should be of concern.
Superficial melanoma
Nodular melanoma
You should also pay attention to the so-called Spitz moles, which are a juvenile form of melanoma. Most often, scientists indicate that this is an active nevus, usually single, and occurs in young people.
The surface of a Spitz mole is very well demarcated from the surrounding area and has a smooth, red or bluish color. Most often it occurs on the face. When observing the lesion, there is no inflammatory reaction. Spitz nevi rarely become cancerous, although it is recommended to remove them before puberty.
Melanoma is a malignant skin tumor
Melanoma is one of the types of malignant skin tumors. The test that confirms or excludes the diagnosis is a biopsy, which confirms the diagnosis based on microscopic examination. The results of the performed biopsy provide information about factors that have a significant impact on the prognosis of the patient's treatment. This information allows you to determine the further course of the treatment process.
Melanoma biopsy
Examination of removed tumors for malignancy is carried out on the basis of macro- and microscopic examination. Among the factors that play a significant role in assessing the patient's health prognosis, primary outbreaks are of great importance. If there are no metastases in the progression of the disease, the change in thickness (Breslow scale) and the presence of ulcers observed in the primary lesion are assessed.
Due to the fact that melanoma is classified as a malignant neoplasm, some patients experience metastases to other organs. Therefore, during diagnosis and treatment, the surrounding lymph nodes are also checked.
The second scenario is a doctor’s mistake (oncologist, dermatologist or surgeon)
A mole was removed without histology, and skin cancer (melanoma) developed at the site of removal.
In our country there is no law that prescribes that all removed skin lesions must be sent for histological examination. Therefore, a very large part of them is removed after a visual inspection - “by eye” - and sent to a waste container. This is where a tragic mistake can occur. If the doctor mistook skin cancer (melanoma) for a benign mole and removed it without histology and corresponding indentation, events unfold as follows:
- a recurrence of melanoma (skin cancer) develops at the site of removal;
- relapse grows more aggressively than the primary tumor and metastasizes early;
- after this, only 30% of patients have a chance to live five years or more [1].
You might be thinking, “ Aha! Here you are! That's all, as people say, a man had a mole removed and he got cancer! ", but you will be wrong. The removed mole was not a benign nevus - it was originally a malignant tumor. All further unpleasant consequences are caused not by removal, but by medical error - incorrect diagnosis and treatment.
You can avoid medical error if the mole is sent for histological examination after removal.
Fortunately, there are very few such stories and it is very easy to avoid them - request a histological examination of the mole after removal. This is the only way you can be sure that it is benign.
The first two scenarios, in my opinion, make up the same 99% of stories like “cancer developed after a mole was removed.” Moreover, the first accounts for the vast majority of such stories.
When is melanoma dangerous?
Metastasis always occurs when the cancer process is far advanced and cancer cells damage subsequent internal organs of a person. First, stage III is indicated when regional lymph node metastases are diagnosed. To treat melanoma, it is important how many lymph nodes are affected by cancer cells.
It is indicated that a much more serious disease is the occurrence of macrometastases, that is, changes that indicate tumor foci in a significantly enlarged, clinically palpable lymph node. Particular danger and difficulties in treatment are indicated for those patients who are diagnosed with infiltrates outside the lymph node capsule.
Melanoma, as a malignant tumor, can also metastasize to distant organs. Then the progress of the disease and the effectiveness of treatment depend on the organs in which the metastases are located and the general condition of the patient.
Briefly about the main thing:
Removing a mole , the benignity of which is confirmed histologically, DOES NOT INCREASE THE RISK OF GETTING MELANOMA. Melanoma can develop 1 cm from the site of removal against the background of normal skin, or maybe on another part of the body against the background of another mole. If a person has a benign mole removed, his chances of developing melanoma are the same as they were before.
Always be critical of what you read on the Internet. Clinical research is more difficult to find, but it is several orders of magnitude more reliable than anonymous posts on the Internet and articles by unknown authors rewritten for the hundredth time.
If you still have questions, you can ask them to me at any time on the forum or in the group.
For urgent questions that cannot be delayed, it is possible to receive a quick answer within one hour for a reasonable price.
Treatment of melanoma: what will happen with delayed examination and treatment?
When analyzing methods of treating melanoma, it is indicated that surgical treatment is the basis. However, you should know that only rapid diagnosis and radical action, that is, removal of the entire lesion, can determine the effectiveness of treatment. The basis for the treatment method is an excisional biopsy, which determines the malignancy of the tumor. The lesion is excised along with the edge of healthy tissue.
In special cases, re-treatment is carried out, during which the original lesion site is cut off. A sentinel lymph node biopsy is also performed to assess the severity of the disease. The selection of the sentinel node is made taking into account the location of the original lesion.
Excision of the lesion and histopathological result allow the selection of appropriate treatment. As a rule, if the lesion has been removed and the correct margin has been preserved, and lymphadenectomy has been performed, that is, removal of the lymph nodes, then there is usually no indication for further treatment, but it is necessary to be under constant medical supervision.
Metastases associated with melanoma can appear even several years after surgery to remove the primary lesion. The risk of metastases, as well as the time at which they may appear, depend on several factors, the most important of which is the thickness of the primary lesion.
Melanoma metastasis
Wide excision
If a biopsy is diagnosed as melanoma, it must be completely removed.
The surgeon excises the tumor and some healthy tissue around it and underneath it. Normal tissue is captured in order to completely remove all tumor cells. After surgical removal, the skin melanoma is sent to a laboratory for analysis. It is important to check the resection margin - the area of tissue that is located at the incision site. If only healthy tissue is found here, then the resection margin is negative, which means that the tumor has been completely removed. If malignant cells are found at the resection margin, it is called positive. This suggests that the tumor tissue may not have been completely removed. The more healthy tissue the surgeon captures during surgery, the higher the likelihood that the resection margin will be negative. But in some places, for example on the face, the cosmetic effect is important. In such cases, you need to look for a middle ground: try to remove as little surrounding healthy tissue as possible, but so as to completely excise the melanoma and not leave tumor cells in the skin. After surgery, your doctor may prescribe a course of adjuvant chemotherapy. In some cases, if the melanoma is on an arm or leg, amputation is performed. Is it possible to perform laser removal of melanoma? Laser surgery is widely used to remove moles, but it often does not provide any benefit for melanoma. Melanoma is a potentially fatal disease that is a surgical pathology and in most cases must be excised with a scalpel. Most often, the operation is performed under local anesthesia. One of the possible consequences of laser removal of melanoma is that there may simply be no material left for a biopsy; all tumor tissue will be destroyed by the laser. Laser surgery is sometimes used in the early stages of tumors, usually in older people.