Dermatovenerologist
Khasanova
Alina Rashidovna
9 years experience
Make an appointment
Nail onycholysis is a dystrophic lesion of the nail plate, manifested in its separation from the bed while partially or completely maintaining its usual shape. Pathology develops with equal frequency on the fingers or toes. About 60% of detected cases of the disease are the consequences of injuries, up to 30% are formed under the influence of dermatomycosis. The remaining 10% are due to somatic diseases, dermatoses or pyoderma. The disease can develop in a person at any age; women are diagnosed more often than men. In case of traumatic damage to the nail, the pathology does not cause significant discomfort to the wearer; treatment is carried out for aesthetic reasons.
Reasons for development
Dermatologists distinguish three groups of causes for the development of the disease:
- injuries;
- mycoses;
- allergies.
The mechanism of development of onycholysis on the fingers is determined by the root cause of the pathology.
Traumatic injuries to the hands or feet affect the nails and nail bed. A subungual hematoma is formed between them, the vessels in the upper layers of the dermis are compressed, which leads to disruption of the nutrition of the nail, a change in its chemical composition and loss of elasticity. The plate is deformed, the connection between it and the bed weakens. Detachment occurs from the free edge. Violation of the fit increases the risk of infection and the development of inflammation. The nail root does not lose connection with the matrix. After the hematoma resolves, the plate grows as before.
Infectious onycholysis on the arms or legs occurs due to inflammation. The process includes three stages:
- alteration - pathological damage to the dermis, cells of the immune system produce cytokines and inflammatory mediators;
- exudation - disturbance of water-electrolyte balance in tissues, swelling of the nail, development of pathogenic microflora on the bed;
- proliferation - the development of hyperkeratosis of the nail bed with its subsequent deformation.
Normal growth of the nail plate begins after complete relief of the inflammatory process. Complicated onycholysis of fingernails or toenails will require the patient not only to comply with all medical prescriptions of the dermatologist, but also to follow a diet.
The allergic variant of the pathology develops according to a similar scenario to the inflammatory one. During the exudation stage, an excess amount of antibodies to pathogenic microflora is produced. This leads to increased sensitivity of the skin, increased deformation of the nail plate and the adjacent dermis. The regeneration process slows down significantly.
How to get rid of emptiness under the nail: reviews
Emptiness under the nail
If any defects appear on the nails, it is always unpleasant. Women especially worry very much, since their appearance and the way their hands look are important to them. Read reviews from other people who know how to get rid of hollow spots under their nails.
Natalia, 36 years old
Loceryl varnish helped me in the fight for my nails. I got infected in the pool. I stopped the growth of the fungus with varnish, but I couldn’t save the affected part and gradually sawed it off. Now I sometimes paint as a preventive measure, there have been no relapses yet. And there were nail crumbles, white dots inside, waves.
Ekaterina, 42 years old
When I was a student, I bought fashionable shoes one size smaller. I wore it for a long time until my legs began to hurt. The nails on my thumbs turned black, then a void formed. Now they grow back healthy, then again with holes. As soon as I start doing baths, applying creams - everything is fine, you forget a little - and it’s back to old times.
Olga, 23 years old
I got a hardware pedicure in an unfamiliar salon. It was urgent, and my manicurist was on vacation. The girl got under her nail a lot. After this procedure, a void formed at the angle of the nail and almost 1/3 inward. During the consultation, the dermatologist suggested that after the bath, carefully cut off the steamed nail with nail scissors, where there is emptiness. And drip Exoderil into the hole, several times a day. The treatment helped, and now I feel better.
Kinds
Dermatologists distinguish several main types of pathology based on the clinical picture of the disease and the cause of damage to the patient’s nail plates. The most common types of onycholysis are:
- traumatic;
- dermatological;
- endocrine;
- systemic;
- fungal;
- bacterial;
- allergic.
Traumatic lesions of the nails occur after wounds or burns to the patient’s tissues. Probable causes remain splinters, excessive physical impact, and exposure to toxic or toxic substances. Toes can be hurt when wearing tight or poorly ventilated shoes.
The dermatological type of pathology develops under the influence of dermatoses, leading to disturbances in the processes of cellular nutrition in the affected area. Endocrine onycholysis results from humoral disorders in the human body or chronic disorders of the endocrine glands.
Systemic onycholysis is caused by diseases of the human digestive tract and subsequent metabolic disorders. The condition of the patient's tissues improves significantly after eliminating the disease that is the root cause of the separation of the nails from the bed.
The fungal type of pathology is formed after the formation of colonies of microfungi in the subungual space. The subsequent change in the nail bed almost does not affect the nail itself, which remains unchanged. The disease develops as a result of a long-term mycotic infection.
The bacterial course of onycholysis is the result of the addition of a secondary infection to any type of pathology. Allergic lesions of nail tissue develop when the patient takes medications, contacts with chemicals or directed ultraviolet radiation.
Advantages of nail prosthetics for fungus
If a fungal infection occurs, this means that very soon delamination, deformation, splitting and atrophy of the plate will begin. This makes it so fragile that the slightest impact breaks the nail.
If the damage is very severe, the person tries to choose wider shoes and reduce movement to a minimum. It is worth noting that the risk that the fungus will spread to soft tissue is very high. It can also be accompanied by a bacterial infection, followed by severe inflammation.
To avoid everything listed above, prosthetics are used, which help restore health to the lower extremities. However, it is necessary to remember that there is practically nothing in common between this procedure and nail extensions.
In the second case, craftsmen use the synthetic material acrylic, which creates a very durable and non-plastic coating. Plates made from it last a very long time, but if the tissues are affected by a fungal infection, the substance can injure them, which will lead to complications of the disease.
Recommended articles on the topic:
- Medical hardware pedicure
- Curvature of the nail plate
- Removing an ingrown toenail and how to avoid it
When performing nail prosthetics, softer materials are used, which make it possible to create a plate similar to a natural one. They do not have any negative effect on the damaged finger, but only help recovery and prevent re-infection.
Very often, prosthetics are performed for ingrown toenails, which are a consequence of fungus. The fact is that the artificial plate prevents deformation of the natural one and corrects its shape.
Often this procedure is used when most of the nail is removed, which often occurs during surgery on a plate affected by a fungus, or after deep hardware cleaning.
Thus, when, as a result of any therapeutic measures, an open bed is formed, artificial material allows it to be closed, thereby protecting it from damage or infection.
It is worth noting that prosthetics for fungus is a procedure that is performed exclusively in a medical institution by professional podiatrists. Conducting it at home is excluded.
In addition, you should not take risks and trust the manipulation to masters working in beauty salons. The only thing they can do is to place the denture on a deformed, broken or unattractive plate. But they are unlikely to cope with a fungal disease.
Symptoms on arms and legs
The clinical picture of the disease is the same for all types of pathology: the nail plate is separated from the bed from the free edge in the distal or lateral sections to the nail hole. The color of the plate changes from flesh-colored to gray-white due to air entering the subungual space. With the development of pathogenic microflora in the resulting free space, a further change in color is possible: yellow becomes the result of bacterial infections, brown - the formation of a colony of microfungi, green - damage to Pseudomonas aeruginosa.
Bacterial infections affect the structure and strength of the nail plate. The surface of the nails loses its shine, becomes rough and gradually becomes deformed. The subungual space is filled with dirt and keratin. This leads to the development of hyperkeratosis, characterized by an unpleasant odor. In advanced stages of the pathology, a focus of secondary inflammation may develop. Detachment of part of the nail is called partial onycholysis, while the entire plate is called total.
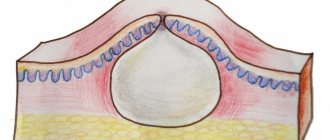
Structure of the nail and nail plate
Our nails are quite complex. The following illustration will help you understand their structure.
Inside the phalanx of the finger there is a thin bone (1). The nail plate (3) grows from the root of the nail (4). Matrix (5) is a special zone responsible for growth. The nail ligament (7) is located under the nail bed. In this place, the nail tissue is fused with soft tissues. The posterior nail fold (9) limits the edges of the nail, on which the eponychium (8) and cuticle are located. There are also rollers on the sides, which are called side bolsters. On the opposite side of the eponicium and cuticle is the free edge of the nail. Underneath it is the hyponychium (6) - a special fold of skin, the shape and size of which is different for each person.
Seeing a doctor
Detecting the first symptoms of onycholysis is a good reason to visit the clinic. Any stage of the disease requires consultation with a dermatologist. During the diagnosis and treatment of the disease, the patient may require the opinions of other specialists: an endocrinologist, a surgeon, a therapist.
Ignoring the symptoms of pathology can lead to multiple damage to the nail plates on the patient’s hands and feet, the formation of numerous foci of infection and damage to other tissues and systems of the body.
Are you experiencing symptoms of onycholysis?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Prevention methods
To reduce the risk of re-infection, you must follow simple rules:
- When visiting public places, you must wear rubber slippers.
- You cannot try on or walk in someone else's shoes.
- Do not use someone else's towel or manicure accessories without treatment.
- Inspect your skin and nails regularly; if the first symptoms appear, you should consult a doctor.
- Boots and shoes should be made from natural materials, appropriate for the season, and not cause discomfort when worn.
- Change socks or tights as they become dirty.
- Use preventative varnishes that protect the nail plate from external influences.
- After the bath, dry your feet, especially the spaces between your toes.
- To prevent dryness, apply moisturizer to your feet.
It is quite easy to protect yourself from the fungus that causes onycholysis: if you suspect an illness, do not delay the process and get examined.
Diagnostics on legs and arms
The diagnosis is made during a visual examination of the patient by a dermatologist. The development of onycholysis is preceded by damage to the nail plates by Bo lines, which occur against the background of damage to the nail matrix. This sign indicates systematic injuries or the presence of somatic pathologies.
A mandatory stage of clinical tests is obtaining scrapings from damaged tissues to conduct laboratory tests and exclude mycotic lesions of the nail and nail bed. Differential diagnosis of onycholysis is carried out with mycoses, psoriasis, lichen planus, Bowen's disease and onychodystrophies of unknown etiology.
Different types of onycholysis on the fingers or toes will require in-depth analyzes to establish the causes of the development of pathology with multiple clinical pictures. The reason for this is the variety of colors of the nail plates, visible differences in their structure, transparency, and area of hyperkeratotic layering.
Basic techniques used in nail prosthetics
- Nail prosthetics with “Ungisan” (filling method).
This prosthetic technique was developed in 1953 by Josef Greppmeier. It involved mixing two components (polymer in powder form and Unguisan (liquid)) to obtain a mass from which a durable and plastic prosthesis was subsequently formed.
In this case, the mixture is poured onto the prepared nail bed and a plate is formed that is as close as possible in appearance to the natural one. In addition, the prosthesis can be made separately for a specific patient, after which it is installed in place.
It is worth noting that this prosthetic technique is only possible if the person has at least a small part of a healthy nail left.
- Nail prosthetics with “Ungisan” using a plate prosthesis.
Using scissors, a blank is cut out of transparent material PG-190/Greppmayr, after which it is fixed to the remaining part of the natural plate using the same mass as in the case of cast-in prosthetics. The prosthesis, which is formed in advance, is placed vertically on the nail fold and then slowly pressed.
Before the material begins to harden, the excess protruding from the sides is removed with a spatula. The artificial nail should not move throughout the entire time until it is completely fixed, that is, until the mass has completely hardened, which usually occurs after five minutes. Before installing the prosthesis, the open bed, which is located below the nail plate, is tamponed, as with the pouring method.
The main advantage of a prosthesis made from a finished plate is that it can be used repeatedly. For example, if it is separated from the rest, the remaining polymer material is removed from the inside by grinding, after which the installation procedure is repeated according to the same scheme described above.
The main condition for prosthetics using Ungisan is the presence of at least three millimeters of a healthy natural nail.
A combined technique can also be used to prevent moisture or dirt from getting under the prosthesis.
- Nail prosthetics using nail mass.
This method of prosthetics is one of the most complex, since during its implementation, conoline (a natural breathable material) and glue are alternately applied. The number of layers depends on the thickness of the nail plate. Finally, the surface is sanded and polished.
After this, the prosthesis is no different in appearance from a natural plate.
As a result, the nail is strong and natural. This is the optimal method of prosthetics for the lower extremities, as well as in case of infection of the plates with a fungus, since the glue used during the procedure contains antifungal drugs.
- Nail prosthetics "Gevolem".
This method involves the use of Gevol gel, which is a hardening polymerization composition containing a light-curing substance. The process is very simple: a soft nail prosthetic agent should be applied to the damaged bed, after which it hardens and a thin elastic surface is formed. At the end, the master can only give the artificial material the desired shape.
The main advantage of this method is its simplicity, which distinguishes it from previous methods.
Gewol gel is available in three colors, namely: pink, transparent and opal. By mixing them, it is possible to obtain a natural shade of a natural plate. Another advantage of this composition is the content of antifungal components. Indications for toenail prosthetics with gel are deformed, broken and delaminated plates.
It is worth noting that the prostheses obtained in this way can be easily painted with decorative varnish, since the material is not afraid of the components it contains, as well as acetone. In addition, when the nails grow, the place where the artificial plate transitions to the natural one is not at all noticeable.
It should be borne in mind that this type of prosthetics is recommended for use if the damage to the fingers is minor, since the material is very elastic.
- Nail prosthetics with acrylic (acrylate).
Nail prosthetics with polygel allows you to grow a plate of a physiologically correct shape. This type of plastic is a new generation invention and is used to create removable dentures. It ensures fixation of the artificial material in such a way that a certain pressure is applied to it. Thanks to this, the distal roller is pressed, and the nail passes freely without resting against it. Only after the plate has grown to the required length is the prosthesis removed.
Treatment of nail onycholysis
Pathology requires complex therapy. The key task is to treat the underlying disease against which onycholysis of the nails develops. The allergic type of damage to the nail plate requires consultation of the patient with a nutritionist or gastroenterologist to adjust the functioning of the digestive system through diet. Correcting the imbalance of minerals and vitamins will reduce the likelihood of further progression of onycholysis.
The traumatic type of pathology involves daily removal of the growing tissue of the exfoliated area, followed by disinfection of the subungual space and protection of the bed with an antibacterial patch.
Large area detachments are treated surgically. After removing the nail plate, antibacterial and antiseptic dressings are applied to the bed. The operation allows surgeons to remove hyperkeratotic deposits, dirt and the consequences of hematoma development. Nail restoration is carried out using gelatin solutions of various concentrations.
Bacterial and mycotic lesions of the nail are treated with alcohol solutions of aniline paints, antibacterial and antifungal drugs.
Reasons why nails move away from the skin
Wearing tight shoes often leads to peeling toenails. Female representatives are more susceptible to the problem when wearing shoes with narrow toes and stiletto heels. Non-breathable shoes can cause splitting, inflammation and suppuration of the nail.
Initially, the thumb is affected; if treatment is not started, it spreads to the neighboring ones. The little finger rarely suffers, only in severe stages.
The nail begins to delaminate and deform after a procedure such as extensions. In open shoes, the nails covered with gel are not in any danger, but in closed shoes they are compressed, bent, and peeled. As a result of the accumulation of infection under the gel, the nail plate and skin are affected, and a void is formed.
The main reasons why the nail begins to move away from the skin:
- fungus;
- injuries and bruises;
- infectious diseases;
- exposure to medications;
- extension;
- aggressive influence of chemicals, including household ones;
- genetic factor.
If the nail is constantly exposed to chemicals, it can also peel off from the skin. For example, upon contact with washing powder, varnish, solvents, etc.
Onycholysis can appear on the legs along with a skin disease. The formation of emptiness can be a side effect of taking fluoroquinol and tetracycline antibiotics. After completing the course of treatment, the nail continues to grow in its natural place. It takes several months for complete recovery.
If delamination occurs only along the edge, most likely it is a fungal disease. The problem cannot be treated at home, but requires immediate medical attention.
If you do not pay attention to the problem, the plate may peel off over its entire area. If a nail falls off, then it is extremely difficult to eliminate the defect.
Make an appointment
You can make an appointment with the specialists of JSC "Medicine" (clinic of Academician Roitberg) on the website - the interactive form allows you to select a doctor by specialization or search for an employee of any department by name and surname. Each doctor’s schedule contains information about visiting days and hours available for patient visits.
Clinic administrators are ready to accept requests for an appointment or call a doctor at home by calling +7 (495) 775-73-60.
Convenient location on the territory of the central administrative district of Moscow (CAO) - 2nd Tverskoy-Yamskaya lane, building 10 - allows you to quickly reach the clinic from the Mayakovskaya, Novoslobodskaya, Tverskaya, Chekhovskaya and Belorusskaya metro stations .
Treatment with folk remedies
It is recommended to carry out treatment with folk remedies if there has been a mechanical injury or chemical exposure and there are no diseases of the internal organs. This treatment of onycholysis is advisable if the body is not affected by infection.
You can cure your nails by taking baths with a beneficial composition, using ointments made from herbs and oils. It is recommended to take a daily bath with a solution of sea salt (take a tablespoon of salt per 1 liter of water). You can also add soothing herbs, calendula or chamomile.
The voids under the nail plate are eliminated with gelatin baths; they will help the nail plate to grow faster and saturate it with protein - the main building material. The bath is prepared in a water bath so that the gelatin dissolves. Do not bring water to a boil so that the beneficial substances do not evaporate.
Tea tree oil has a beneficial effect. It is applied in its pure form every 2 hours. If a void has already formed under the nail, then the oil is dripped directly into it to eliminate bacteria.
If the nail plates move away from the fingers, baths with iodine are made 2 times a day. 5 drops of the drug are added to the container. The duration of the procedure is 15 minutes.
If the nail is moving away from the nail bed, aloe juice will help solve the problem. Compresses are made from fresh leaves of the plant, using leaves of a tree that is more than 2 years old.
Nail diseases - symptoms
Symptoms of nail disease are visible to the naked eye. Therefore, they should pay special attention to:
- nail color - white, yellow, green, gray, brown can be a symptom of the disease;
- the shape of the nails - scapular, gonadal, tubular - is incompatible with the natural growth of the nail;
- nail structure - longitudinal grooves and transverse grooves should attract attention;
- general condition of nails – brittle, peeling;
- condition of the skin around the nails - redness, swelling, bumps.
For fungal infection
Such a serious reason for the development of onycholysis as a fungal infection requires not only the use of special drugs, but also long-term treatment using folk remedies. To do this you need to show persistence and patience.
It is very beneficial to fight fungus with regular iodine. They need to lubricate the damaged nail twice a day for 20 days.
Propolis tincture
Propolis tincture (20%) can be a real salvation for this disease. It is recommended to soak the diseased nail in the solution using a tampon for 10 minutes. In just a few days, the plate will be able to move away, and a new one will grow in its place.
You should not always resort to expensive medications if problems arise with your nails; minor damage can be cured using traditional methods. But if a serious problem arises, consultation with a specialist becomes a vital necessity.
Nail care should not be limited to manicure and pedicure. Fingers will be beautiful if they are healthy. The “reference” nail is even, smooth, and pure pinkish in color. Any other color effects: grooves, white spots, etc. - all these are deviations from the norm; they are not cosmetic defects, but belong to the category of diseases.
Diseased nails have an unsightly appearance
Rehabilitation after removal of an ingrown toenail
The recovery period after excision of an ingrown nail is on average 1 month. During the rehabilitation period it is recommended:
- Ensure the patient remains calm.
- Regular treatment of the nail with antiseptic agents and bandaging.
- Applying medications prescribed by a doctor to the wound.
- Taking painkillers for pain.
- Wearing loose shoes that do not put pressure on the toe.
- Other procedures indicated by the surgeon.
During the recovery period, you must strictly adhere to the doctor's instructions for a successful recovery.
Signs
It is usually easy to notice the problem visually, since the nail plate partially or completely becomes white, which explains the appearance of a void between the stratum corneum and the nail bed. However, most often more than one emptiness appears, which indicates the development of the disease - Onycholysis.
It is accompanied by a number of signs and symptoms:
- Thickening of the nail surface;
- Changing the shade of the manicure area. It appears yellowish, and individual spots may appear;
- Peeling of the side ridges, the appearance of a non-standard skin structure in the form of scales;
- The appearance of itching;
- Redness of fingers;
- Discomfort when pressing on the fingertips;
- The formation of irregularities on the nail, the detachment zone becomes convex.
Symptoms are found in most cases, however, in the presence of internal pathologies or aggressive influence of external factors, additional symptoms may form.
For example, when a fungus appears, dark or light spots may form on the surface, and the nail itself becomes dull and rough. The formation of ingrowth is possible with the progression of pathogenic microflora.
Also, often in the initial stages of the development of the disease, most signs may not appear, so you need to pay attention to even small cosmetic defects.
Diagnosis of onychocryptosis
Diagnosis of ingrown toenail disease may include the following steps:
- The doctor listens to the patient's complaints.
- The surgeon visually examines a finger with an ingrown nail, identifying the underlying disease and associated diseases, such as fungus.
- When the inflammatory process begins, the doctor prescribes tests:
- general analysis to determine the degree of the inflammatory process;
- blood glucose test to determine diabetes mellitus;
- culture of purulent discharge to determine the type of infection.
- The doctor prescribes an x-ray of the foot, which will determine the size and shape of the nail growth, damage to bone structures and the area of suppuration.
After diagnosis, the doctor prescribes treatment, which depends on the stage of the disease.