Symptoms of candidiasis in women, treatment and prevention
Candidiasis (thrush) in women is a common disease caused by yeast-like fungi of the genus Candida, which penetrate the female body through sexual, contact and nutritional routes. However, talking about infection with a fungus in this case is not entirely correct, since, under normal conditions, it is part of the normal microflora of the mucous membranes of the human body bordering the external environment.
Initially, the body's natural defense mechanisms and constant interaction with other microorganisms of normal microflora prevent Candida fungi from causing a harmful process. However, when certain conditions occur, they acquire pathogenic forms and begin to parasitize the epithelial cells of the mucous membrane.
Causes
Why thrush occurs is one of the most common questions among women. After all, this problem is very common. Unpleasant sensations arise at the most inopportune moment. This fungal disease destroys intimate relationships and ruins everyday life.
You can become infected with candidiasis from a sexual partner. Especially if a man has obvious signs of this disease or is a carrier of fungi. However, this reason is far from the most common. Much more often, thrush occurs as a consequence of decreased immunity and disruption of the natural balance of the microflora of the genital organs.
There are many factors that provoke the development of vaginal candidiasis in women.
- Changes in hormonal levels during menopause.
- Use of hormonal contraceptives.
- A decrease in the body's defenses as a result of chronic diseases or after infections.
- Hormonal changes during pregnancy and before menstruation.
- Use of intimate hygiene products: intimate gels, soaps, shower gels containing a lot of alkali and fragrances.
- Long-term use of antibiotics, corticosteroids and cytostatic drugs.
- Intestinal dysbiosis, in which fungi can be introduced into the vagina.
- Deodorized tampons and pads cause allergic reactions and disrupt the condition of the mucous membrane.
- Climate change, which entails adaptation to new conditions and water composition.
- Using panty liners. They interfere with air access to the genitals, increasing humidity.
- Vitamin deficiency entails a decrease in the body's resistance and a deterioration in the condition of the skin and mucous membranes.
- Wearing underwear made of synthetic fabrics, narrow and tight. The most common culprit for thrush is thongs.
- The diet is rich in confectionery and carbohydrate dishes, strong coffee, carbonated drinks, yeast baked goods, spicy and fatty delicacies, ketchup and mayonnaise.
- Metabolic disorders. A striking example is diabetes mellitus. It not only weakens local immunity, but also increases the amount of carbohydrates in cells, which is a good breeding ground for microorganisms.
- Obesity - favorable conditions for the proliferation of fungi are created in the folds of the body.
- Chronic stress, severe mental and physical stress, overwork, lack of sleep.
- Sexual intercourse with a dry vagina and other actions that can lead to microtraumas on the genital mucosa. Through them, Candida can penetrate deep into the tissues.
- Chronic stress, severe mental and physical stress, overwork, lack of sleep.
- Smoking causes vasospasm and impairs blood circulation, including in the genitals.
The action of these factors leads to a decrease in the number of lactobacilli that create a protective microfilm. They produce less lactic acid, and an alkaline environment is formed in the vagina. Fungi and other bacteria penetrate the cells of the mucous membrane and thin skin of the external genitalia. There they begin to actively reproduce, feeding on glycogen and destroying host cells. If left untreated, the inflammatory process gradually spreads.
What is oral candidiasis?
Oral candidiasis (also called oral thrush) is an infection of the mouth caused by the yeast-like fungus Candida. These microorganisms are part of a healthy microflora, but under certain circumstances their reproduction disrupts the favorable environment and becomes a source of disease processes. Inflammation and plaque on the tongue, ulcers on the mucous membrane and discomfort in the mouth - this disease is called oral candidiasis.
Infants are most susceptible to this disease, but at this age it is treated faster and is tolerated almost painlessly. Oral thrush is often observed in adults after 50 years of age, when the immune system is already weakened. Oral candidiasis is less common in men than in women. Recently, the percentage of cases has increased significantly, which is associated with uncontrolled use of medications: weakening of cellular immunity increases the risk of oral candidiasis after antibiotics, or rather their improper use. Microbiology, the science of microorganisms, studies the essence of oral candidiasis. And she successfully copes with her task, at the moment this disease has been studied in detail, and doctors know all the methods of treating and preventing infection.
Symptoms of candidiasis in women
The pathology is characterized by specific manifestations that allow the disease to be quickly and accurately diagnosed.
As a rule, a woman herself can determine the presence of candidiasis (see photo) by the following symptoms:
- Pain and discomfort during urination and sexual intercourse. This symptom is due to a decrease in the protective functions of the mucus of the urethra and vagina;
- Burning itching in the genital area. It is worth noting here that experts categorically prohibit scratching the affected area too much, as there is a risk of damaging the inflamed layer of the mucous membrane. In this case, favorable conditions are created for the penetration of fungi into deep tissues. In addition, when scratching, vaginal discharge can fall on a healthy surface, which will cause additional inflammation and spread of the disease;
- Vaginal discharge, which can be described as “cheesy” (hence another name for the disease “Thrush”). The discharge is usually clearly visible on dark-colored underwear and consists of mucus with many white dense lumps;
- A specific smell from the genitals, which has a slight sour milk tint. As a rule, the smell is noticeable only by the patient herself, but this is enough to become a tangible problem for a woman. On a subconscious level, the patient is afraid that the people around her may also feel it, hence the symptom of candidiasis in women such as emotional imbalance.
If a woman, having suspected the development of candidiasis, promptly sought help from a specialist and faithfully followed all his recommendations, the prognosis of the disease is very favorable. But, if the patient does not pay attention to the symptoms of the disease for a long time or ignores the doctor’s instructions, the fungi continue to actively multiply.
Classification of oral candidiasis
This disease is usually divided into several types, each of which has its own characteristic features. Experts distinguish between acute and chronic oral candidiasis.
Acute pseudomembranous candidiasis
Characteristic of infants with weakened immunity. Oral candidiasis, or oral candidiasis, can be triggered by a previous infectious disease or gastrointestinal disorder. The disease is transmitted through a pacifier or dishes; the disease manifests itself in the form of a light or grayish coating on the mucous membrane. At the initial stage, plaque is painlessly removed; with the development of candidiasis of the oral mucosa and pharynx, it thickens and spreads in the oral cavity. It is almost impossible to remove plaque on the tongue without causing bleeding.
Acute atrophic candidal stomatitis
Accompanied by peeling of the integument, dryness and burning of the mucous membrane, it is painful for the patient to eat and touch the infected area. With this form of oral candidiasis, the infection can spread further - to the larynx, pharynx and even the esophagus.
Chronic hyperplastic candidiasis of the oral cavity
It is characterized by a change from a whitish coating to a grayish-yellow one, after removal of which slight bleeding occurs. Along with plaque, plaques and thickenings appear that cannot be cleaned off or removed; they go away on their own during the treatment process.
Chronic atrophic candidiasis of the oral cavity
It is diagnosed when inflammation spreads to the skin and cracks appear in the corners of the mouth. In this case, the tongue becomes a shiny, rich pink color, and the vessels are clearly visible on it. Then the infection spreads to the internal organs. This type of oral candidiasis can occur due to improper installation of dentures, plates and crowns, which rub and injure the mucous membrane.
Diagnostics
Diagnosis of vaginal candidiasis in women is based on the patient’s complaints, laboratory test data and the clinical picture of the disease.
The main methods for diagnosing thrush are:
- Culture seeding of secretions - the method is based on seeding material taken from the mucous membrane of the genital organs onto a nutrient medium. In addition to Candida fungi, using this research method, it is possible to identify pathogens of sexually transmitted infections, as well as determine their sensitivity to antibiotic drugs;
- Microscopic examination - this method is one of the simplest and most reliable ways to identify fungi of the genus Candida. The study consists of collecting material (a smear from the vagina and mucous membranes of the genital organs), which is examined under a microscope for the presence of Candida fungi;
- Colposcopy - using this method, you can detect signs of inflammation of the vaginal mucosa and accurately determine the presence of curdled discharge.
Additional methods for diagnosing the disease include general urine and blood tests, determination of blood glucose levels, identification of pathogens of other infections with a similar clinical picture using PCR (polymerase chain reaction).
Forms and symptoms of the disease
Candida mushroom
Intestinal candidiasis can take different forms, depending on the cause of the active proliferation of the fungus. Among all forms, they most often suffer from candidal dysbiosis, which is known as non-invasive candidiasis. This form of the disease is expressed by damage to the intestinal mucosa. It occurs through the active reproduction and growth of the Candida fungus or if the patient suffers from individual hypersensitivity. The form of fecal candidiasis never develops as an independent disease. It occurs as a complication of peptic ulcers.
The most complex and rare type is considered to be the diffuse or invasive form. When it develops, the patient experiences loose stools, in which there are traces of blood, and erosive-pseudomembranous colitis. This form usually develops in HIV-infected patients and those suffering from cancer. It can develop in people who regularly use glucocorticosteroid drugs, immunosuppressants and cytostatics. The main symptoms of intestinal candidiasis:
Treatment of candidiasis in women
The treatment regimen for candidiasis in women is always individual and depends on the degree of neglect of the fungal infection, the state of the immune system and test results. It is possible to repeat the treatment course, in combination with antibacterial and antiprotozoal drugs for combined infections.
Preparations for the treatment of candidiasis in women at home:
- Natamycin (Pimafucin) is No. 1 for pregnant women with thrush.
- Nystatin (tablets, vaginal suppositories) has fairly low antifungal activity. Included in combined local remedies (for example, Terzhinan), suitable for combined fungal/bacterial infections.
- Miconazole (combined drug Klion-D) is a fast-acting drug (recovery in 1 week), used for candidiasis, bacterial vaginosis, trichomoniasis.
- Clotrimazole - for topical use (ointment, suppositories, vaginal tablets). Use at the very beginning of the disease or in combination with oral medications is recommended. Treatment course - 2-4 weeks.
- Fluconazole (Mikosist) - one 150 mg tablet is sufficient for acute manifestations. For prolonged candidiasis, take three times a week.
- Ketoconazole is an effective new generation remedy (ointment, tablets). Treatment of the acute form is 5 days, chronic - 10 days.
Local treatment with home remedies may also include:
- Douching with soda is effective with antifungal therapy, but the duration of use is limited to 7 days (dries out the mucous membrane);
- Decoctions of medicinal herbs with an anti-inflammatory effect (chamomile, sage), when used judiciously (no more than a week), will speed up recovery, but are not a panacea for thrush.
During treatment, abstinence from sexual intercourse is required. If a partner has symptoms of a fungal infection, mutual treatment is necessary.
Causes of oral candidiasis
A healthy person is still a carrier of fungi of the genus Candida, since they are part of the microflora and calmly coexist with other microorganisms without causing harm. But any change in the balance in the body can lead to rapid proliferation of bacteria and the development of disease. A weakened state of immunity plays a key role in the etiology of oral candidiasis, but any of these reasons can be the starting point for the onset of the disease:
- pregnancy;
- immunodeficiency states;
- infectious processes;
- long-term treatment with antibiotics or improper use of medications;
- injuries and damage to the oral mucosa;
- insufficient oral hygiene;
- contact with an already sick person.
Will folk remedies help?
Folk remedies for candidiasis can only provide temporary relief; they cannot fight the causes of the disease. Traditional methods should be used exclusively as auxiliary and only on the recommendation of a doctor.
For vaginal candidiasis, you can wash yourself with a weak soda solution, water with the addition of tea tree oil, eucalyptus, or chamomile decoction (douching is not recommended, especially for expectant mothers). You can use the same products to rinse your mouth if candida has become active in it, or wipe the skin affected by the fungus. For intestinal candidiasis, you can drink a decoction of wormwood root or tincture of juniper fruits.
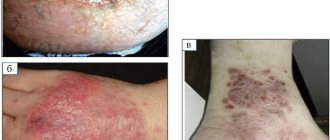
Candidal dermatitis in an adult
Candidal dermatitis in adults, unlike children, develops more often in the armpits, inguinal folds, under the mammary glands, less often between the fingers and in the folds of the skin in obesity (as shown in the photo), and in this case, treatment also consists of eliminating provoking factors and the use of antifungal drugs.
In bedridden patients, dermatitis caused by these fungi develops on the back.
Cases have been described in which candidiasis developed under the ring on the finger in patients with reduced immune system function.
In young mothers who are breastfeeding, an inflamed nipple with very severe soreness can also be caused by candidiasis. This makes feeding the baby much more difficult. The infection is most often transmitted from the baby's mouth, especially if he has candidiasis of the oral mucosa. Some researchers believe that cutaneous candidiasis is the main cause of nipple pain associated with breastfeeding.
Prevention
To reduce the risk of thrush, you should follow your doctor's recommendations:
- Wear comfortable cotton underwear.
- It is not advisable to use tampons for more than three hours at a time. Panty liners should be changed every two to three hours.
- Maintain intimate hygiene regularly (wash yourself at least twice a day). In this case, it is also advisable to use special gels for the intimate area based on lactic acids. These products will create favorable microflora on the mucous membranes.
- You should not use colored, much less scented, toilet paper or napkins.
- When treating with antibiotics, it is important to take special bifidobacteria to maintain intestinal microflora.
- You should minimize the consumption of sweets and starchy foods.
- In hot weather, you should not stay in a wet swimsuit for a long time.
- Avoid casual sex. If this happens, be sure to use a condom.
- Enrich your diet with fruits and vegetables, as they contain healthy vitamins. You can also take additional vitamin complexes.
- If you notice the first signs of candidiasis, you should immediately consult a doctor before the disease progresses to a more advanced form.
- Visit your gynecologist regularly for preventative check-ups. At the same time, it is also important that the sexual partner undergoes all tests.
- Avoid stress and severe nervous tension.
- Control your weight and prevent obesity.
- You should not self-prescribe oral contraceptives (pills). They must be selected by a doctor. The same applies to taking hormonal medications.
You should not douche unless urgently necessary, so as not to once again wash out the microflora from the vagina. In general, gynecologists do not recommend that women often douche. This is an extreme measure permissible in case of serious inflammatory processes.
Prevention of oral candidiasis
The occurrence of this disease is a very unpleasant and painful phenomenon, fortunately, it is quite easy to avoid by following the recommendations. One of the main causes of infection is weakened immunity, so the basic rule for preventing the disease is to treat any disease at the right time and take medications strictly as prescribed by the doctor. To avoid candidiasis of the oral cavity, pharynx and larynx, hygiene, visiting a good dentist, professional ultrasonic cleaning and other preventive measures will help. Oral candidiasis in women is often due to hormonal imbalance; if you have symptoms of the disease, you should pay attention not only to the affected area, but also to the condition of the body as a whole.