Your child has microsporia
To children, the world can seem like one big playground full of adventure. But their desire to play in the ground, pet animals, touch other people's things can lead to infection with various infectious and parasitic skin diseases. Children are especially susceptible to this because their immune systems are not yet fully developed. Summer, holidays, children's holidays in camps, outside the city, lead to a seasonal rise in these diseases. Currently, one of the common skin infections is microsporia. Microsporia affects mainly children of preschool and school age, less often adults. Microsporia is caused by a fungus that gets on children's skin called Microsporum. The fungus is very stable in the external environment. In hair, skin flakes, wool, dust, it retains the ability to infect for several years.
How can your child become infected?
Infection occurs through direct contact with a sick animal (cats, kittens, less often dogs), or objects infected with hair or scales (combs, hats). It is possible to transmit microsporia from sick family members, but this happens less frequently. There have been cases of children becoming infected after playing in the sandbox. However, if you follow the rules of personal hygiene, even if the pathogen spores come into contact with the skin, the disease can be avoided.
How does the disease manifest in a child?
After an incubation period of 5-7 days on average, foci of infection appear on smooth skin or scalp. Microsporia can appear on any part of the skin, but more often on exposed parts of the body. In mild forms of the disease, round lesions form on the skin, clearly defined, covered with scaly nodules and blisters along the periphery. They often form bizarre shapes, like a “ring within a ring”. At the same time, vellus hair may be affected, which complicates the treatment of the disease. The number of lesions ranges from single to several dozen. Size from 0.5 to 3 cm. When the scalp is affected, 1-2 large lesions are formed, round in shape, with clear boundaries and abundant pityriasis-like peeling. The hair breaks off at a height of 6-8 mm above the skin level (hence the name of the disease - ringworm), because the hair in the lesion appears to be trimmed. There may be slight itching in the affected area. The general condition of children is usually not disturbed. With a decrease in immunity, a child may experience complicated forms of microsporia - infiltrative and suppurative forms. The infiltrative form is characterized by the development of severe inflammation in the lesion. The suppurative form is characterized by the formation of dense foci, round in shape, consisting of deep abscesses (cavities filled with pus). Nearby lymph nodes increase in size. The child's general condition may worsen and the temperature may rise. If a child has suffered microsporia in a mild form, then no traces of the disease remain on the skin or scalp. After a complicated form of microsporia, scars may remain on the skin, and focal baldness may remain on the scalp.
Before treatment, visit a doctor.
If a suspicious rash appears on a child’s skin or scalp, consult a dermatologist without first lubricating the affected areas, as this may complicate diagnosis. Correct diagnosis is half the success in treatment. Skin lesions with microsporia can be confused with other types of lichen, psoriasis, eczema, and hair loss may not be caused by a fungal infection. The diagnosis of microsporia is established on the basis of external signs and must be confirmed by microscopic examination and isolation of the pathogen (growing on a nutrient medium). An important diagnostic criterion will be the greenish glow of the affected hair in the rays of an ultraviolet quartz lamp. A similar study is also used in veterinary medicine, so if you have any doubts about the health of your furry pet, take him to the doctor too, but to a veterinarian. As in children, ringworm in pets (dogs, cats, etc.) can appear as patches of hair loss and skin inflammation. However, many animals infected with microsporia have no symptoms and appear completely healthy and safe. This phenomenon is called colonization.
How to cure microsporia or ringworm in a child?
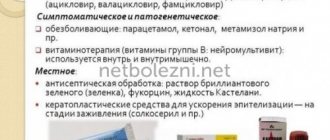
If the doctor confirms that your child has microsporia, he will be able to prescribe you the correct treatment, without which the disease can take a very long time to develop, can cause complications and can spread to other people. Uncomplicated, single lesions on the skin, without damage to vellus hair, can be treated on an outpatient basis, using only external antifungal agents. During treatment, you should not bathe your child in the bath; wash only in the shower, trying to avoid areas with rashes and using antifungal shampoo for washing. Be sure to provide your child with individual bath and bedding items, and iron clothes with a hot iron after washing. Disinfect all toys with an available antiseptic or boiling water.
Numerous foci of microsporia on smooth skin, with damage to vellus hair, damage to the scalp, and complicated forms are an indication for treating a child in a hospital. In addition to external therapy, systemic antifungal drugs are used for treatment. The dose and frequency of taking systemic antimycotics is prescribed by the doctor, taking into account the child’s weight, his general condition, and the manifestations of the disease. How do you know if treatment for ringworm is helping?
In order to determine how the treatment is going, it is necessary to take control tests from the lesions for fungi.
If the tests show that there are no living fungi in the scrapings, this will mean that the treatment was effective.
Typically, the number of fungal spores in the skin and hair is significantly reduced 2 weeks after the start of treatment. The complete disappearance of fungi occurs later. Sometimes, despite active treatment, the release of fungal spores can continue for several months.
If tests show that, despite treatment, fungi are still present in the skin tissues, the doctor may advise either prolonging treatment, prescribing you other antifungal medications, or increasing the dosage of the drug.
Is there any other way to quickly cure ringworm?
Unfortunately, there are no faster and easier methods for treating ringworm.
Can ringworm go away without treatment?
There are cases when ringworm went away on its own. However, more often than not, it does not go away without treatment and spreads to other areas of the skin.
In a child with ringworm, if left untreated, the disease may persist into adulthood.
Can ringworm reoccur?
The human body is not able to develop immunity against the fungi that cause ringworm, so both adults and children can develop the disease again if they become infected with the fungi again.
Ringworm can also recur if treatment is not completed and if viable fungal spores remain in the skin tissue and hair.
Is there a (vaccine) shot for ringworm?
Unfortunately, an effective vaccine against ringworm in humans has not yet been developed.
Carefully following your doctor’s recommendations will help you quickly cope with the disease, and following preventive measures will prevent infection.
How to prevent infection with microsporia?
Considering that the main source of microsporia infection are stray animals, parents, and caregivers. teachers should explain to children that they should not pet or play with stray cats and dogs. To prevent microsporia, you must follow the following rules:
Keep children's hands, body, and hair clean. Do not allow children to wear other people's things, hats, or use other people's combs. Make sure that children wash their hands thoroughly after playing outside, after contact with pets, especially if they are walking outside, and do not take them to bed. Under no circumstances should you play with homeless animals. If you decide to bring a cat or dog into your home, you should definitely check them with a veterinarian. Do not throw sick cats and dogs outside. This contributes to the spread of the disease among animals and can become a source of infection for children. Be carefull.
Solar lichen: causes and symptoms of the disease
29.01.2021
In summer, most people like to lie in the sun. Sometimes, after lying down like this, strange white spots appear on the body. They begin to peel off. What is this and what causes it?
This disease is called solar lichen . The causative agents of the disease are fungal microorganisms that live on the skin. In their normal state they are harmless.
After prolonged exposure to the sun, the fungus becomes active and affects areas of the body. The skin is affected mainly in the warm season.
This disease, which is classified as dermatological, is not considered contagious. A person can be a carrier of the fungus but not have symptoms of the disease.
The main causes of the disease:
- problems with the vegetative-vascular system;
- problems with the endocrine system and excess weight, diabetes ;
- frequent colds;
- problems with the liver and bile ducts;
- increased sweating;
- synthetic clothing;
- love for solariums;
- using sunscreen;
- lack of personal hygiene;
- use of drugs that weaken the immune system .
If you have sun lichen, you should not expose your body to tanning, as this can cause an exacerbation of the disease.
Symptoms of the disease are visible to the naked eye; it is indicated by the appearance of asymmetrical spots with uneven edges. Their color may vary. This is the first stage of the disease.
After some time, the spots may darken and merge into one whole. They will be conspicuous because the tan does not stick to them. This is already the second stage. The spots do not become inflamed, red, or swollen, but scales form on them, causing itching. If you scratch them, they begin to peel off.
Spots appear mainly on the chest , back , sides, stomach , and neck . In children and adolescents, the main places of localization are the head, lower and upper limbs, and armpits.
Solar lichen is considered a beach disease, so at the first symptoms you need to stop being in the sun. This disease has a fairly long incubation period, which can last from two weeks to three months. lichen appears in both autumn and winter.
To make a correct diagnosis for this disease, the doctor needs to conduct a thorough visual examination of the skin. In addition to the examination, it is necessary to undergo a general blood and urine , and blood biochemistry tests. And only after that the doctor will prescribe treatment.
A stool test may be required . Also, if necessary, special studies are carried out in the form of the Balzer iodine test, when a little iodine is applied to the lichen . If it really is ringworm , it will change color to brown. Another examination is carried out using fluorescent lighting. The light stream is directed onto the formed spot. If it changes its color and turns green or red, then the diagnosis is confirmed. The test for the presence of Beignet's symptom involves scraping off the top layer of the epidermis. The results are compared with the symptoms of leukodermatitis, leprosy, Gibert's disease, syphilitic roseola, and a diagnosis of solar lichen .
To avoid becoming the owner of solar lichen , prevention is needed. To avoid getting burns, take sunbathing in the morning and evening, use a protective cream, wear clothes made from natural fabrics, do not visit the solarium, and eat fresh fruits and vegetables. Do not use antibacterial soap or gel constantly, watch your heart and blood vessels .
Solar lichen does not stain, although it is not dangerous, so treatment should be timely.
Published in Dermatology Premium Clinic