Factors causing the disease
This disease is chronic and can be transmitted at the genetic level. However, among the reasons for its appearance or exacerbation, doctors name several factors:
- weakening of the immune system and increased infections;
- exposure to third-party chemicals (medicines, household and industrial preparations);
- the body’s own synthesis of dangerous components due to stressful situations;
- existing diseases (allergies, gastrointestinal disorders, damage to the mucous membrane, diabetes).
Accurate identification of the most likely causes of the disease subsequently determines the most effective method of treating lichen ruber.
Forms and complications
Skin manifestations of lupus erythematosus include three groups, each including specific skin manifestations:
- acute cutaneous lupus erythematosus (localized, generalized and toxic epidermal necrolysis-like);
- subacute cutaneous lupus erythematosus (ring-shaped, papulosquamous, drug-induced, erythrodermic, poikilodermic, vesiclobulous, Rowell syndrome);
- chronic cutaneous lupus erythematosus (discoid, edematous, panniculitis, pernioid, lichenoid).
The identification of these forms is due not only to the duration of the skin disease, but also reflects the connection with systemic lupus erythematosus.
Most often, the manifestation of systemic disease is acute forms, while the discoid form is observed only in 5-15% of all cases. The longer skin manifestations exist in isolation, the lower the risk of developing a systemic form of the disease. The risk of systemic disease in the presence of cutaneous manifestations is higher in women and children.
Lupus erythematosus rashes can occur in children (antibodies are passed on to the fetus) from mothers with systemic lupus erythematosus. This form is called neonatal lupus, occurs during the first two months of a child’s life and may be the first sign of systemic lupus erythematosus in the mother.
The systemic lupus erythematosus complex may also include other changes in the skin and its appendages that are not specific exclusively to this disease.
Proven methods for treating lichen ruber
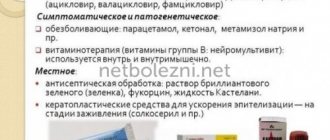
Therapeutic methods are the main method of treatment and depend on the stage of the disease. At the same time, an integrated approach is being implemented aimed at blocking both the causes themselves and the unpleasant consequences of deprivation:
- impaired functioning of the immune system, which is the cause of the manifestation of lichen, is leveled with the help of immunosuppressants;
- the main means of treating lichen planus are hormonal drugs that reduce the supply of components to the foci of immune inflammation that cause the development of ulcers;
- an integral stage of recovery procedures will be the administration of anti-allergenic drugs and vitamin A, which promotes the effective healing of eroded layers of the skin or mucous membrane;
- in severe forms of the disease, antibiotics and synthetic interferons and interferonogens are prescribed in the treatment of lichen ruber.
In addition to taking medications, their analogues in the form of ointments are used, as well as physiotherapeutic procedures (UV and laser irradiation, magnetic therapy). As part of an integrated approach, folk remedies based on natural substances are effective.
Our center’s specialists will be able to determine the optimal and effective treatment. They have the appropriate equipment and sufficient experience to make a detailed diagnosis of the factors causing lichen planus.
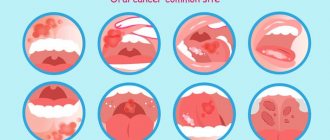
Lichen planus is a chronic polyetiological disease with rashes of papules on the mucous membranes and skin. Isolated lesions of lichen planus of the oral mucosa are observed in 75% of cases. This is one of the most common diseases of the oral mucosa.
The appearance of lichenoid rashes in the oral cavity is usually associated with emotional stress, neuropsychic shocks, and negative emotions. Disturbance of neuroendocrine regulation (early onset of menopause) is important.
The erosive-ulcerative form of lichen planus of the oral mucosa, being a precancerous disease, requires close attention and qualified treatment from the dentist. If a dentist identifies a total lesion of the oral mucosa with an erosive-ulcerative form of lichen planus, the patient is referred for inpatient treatment to a skin disease clinic.
In the hospital, as a rule, the patient receives large doses of corticosteroid drugs and other medications by mouth. At the same time, less attention is paid to the local treatment of erosive and ulcerative lesions of the oral mucosa [1-6].
The purpose of the study is to develop an effective method for treating the erosive-ulcerative form of lichen planus in a clinic with total damage to the mucous membrane of the oral cavity, gums and lips.
Material and methods
Clinical examination and treatment of patients was carried out at the Department of Diseases of the Oral Mucosa of the Department of Hospital Therapeutic Dentistry, Periodontology and Geriatric Dentistry.
We observed 7 patients (1 man and 6 women) aged from 46 to 71 years with an erosive-ulcerative form of lichen planus (see table).
Complaints upon admission
Patients complained of an unusual appearance of the oral mucosa, loss of taste, burning sensation, pain when eating and brushing teeth, roughness and tightness of the oral mucosa.
All patients had anxiety-hypnotic syndrome, negative psycho-emotional states with a tendency to depression, and cancerophobia. The disease progressed with alternating periods of remission and exacerbation. Exacerbation was always preceded by stress.
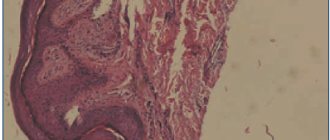
When examining the skin of 3 patients, single papules were revealed on the skin of the forearms of the hands. When examining the oral mucosa, multiple papular rashes were revealed on the dorsal surface of the tongue, the mucous membrane of the cheeks, lips, and the vestibular surface of the gums (Fig. 1, 2).
Figure 1. Lichen planus, erosive-ulcerative form. Patient A., 52 years old.
Figure 2. Lichen planus, erosive-ulcerative form. Patient B., 46 years old.
On the mucous membrane of the transitional folds of the cheeks and the ventral surface of the tongue, against the background of bright hyperemia, sharply painful extensive erosions and ulcers were detected (Fig. 3)
Figure 3. Lichen planus, erosive-ulcerative form. Patient G., 68 years old.
Treatment method
The essence of the method lies in the combined use of steroid drugs - both as a general course (prednisolone) and locally (diprospan). A set of therapeutic measures was carried out in the oral cavity. In addition, after consultation with a neuropsychiatrist, patients were prescribed daily antidepressants: fluoxetine 20 mg, 1 capsule in the morning or Cipralex - 10 mg, 1 tablet in the morning.
The course of treatment with antidepressants depended on the duration of the disease, the severity of psycho-emotional changes and was 3-6 months.
Successful treatment of patients in our group without prescribing oral prednisolone is currently not possible. But our task was to use this drug in gentle doses.
This scheme was proposed earlier by Prof. A.L. Mashkelleyson:
1. Prednisolone 0.005 g
Regimen: 1st week - 4 tablets per day, every other day;
2nd week - 3 tablets per day, every other day;
3rd week - 2 tablets per day, every other day;
4th week - 1 tablet per day, every other day.
2. Delagil 0.25 g 1 tablet 2 times a day, daily, course 4 weeks.
3. Vitamin PP 0.05 g 1 time per day, after meals, course 4 weeks.
4. Vitamin A, oil solution, 8-10 drops on rye bread 2 times a day, course 4 weeks.
Local treatment
We attached significant importance to this stage of treatment. Traumatic factors were eliminated, hygiene correction, professional hygiene, and replacement of prostheses made of dissimilar metals were carried out. Candidiasis was excluded. Antiseptic treatment of erosions and ulcers was carried out, followed by rubbing in prednisolone ointment, and after 10 minutes - Cholisal or Kamistad gel.
With preliminary premedication (sedatives, antihistamines), diprospan 1 dose and 4 ml of a 2% lidocaine solution (without a vasoconstrictor) were administered under elements of damage to the oral mucosa (foci of exudation and hyperemia, erosion, ulcers) with an insulin needle.
If necessary, the injection of diprospan was repeated after 4-6 weeks.
Characteristics of drugs
1. Cipralex, fluoxetine
Daytime antidepressants. Eliminate depressive reactions of various origins, panic disorders, anxiety, phobias. Helps improve mood.
The therapeutic effect develops after 3-4 weeks of continuous use. Does not cause sedation.
Fluoxetine
20 mg, 1 capsule in the morning, regardless of meals. Then the dose is gradually increased to 2 capsules - taken twice in the morning. The course of treatment is 3-6 months.
Cipralex
- 10 mg, 1 tablet in the morning.
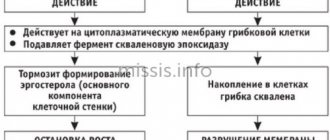
2. Diprospan
Diprospan* is a glucocorticosteroid drug. International (nonproprietary) name: betamethasone*.
, Belgium.
Dosage form: suspension for injection. 1 ml of diprospan suspension contains 6.43 mg of betamethasone dipropionate and 2.63 mg of betamethasone sodium phosphate. The combined composition of the drug has significant advantages when used in clinical settings. One of the components of the drug (betamethasone sodium phosphate) is highly soluble and easily absorbed from the injection site, which provides an anti-inflammatory and analgesic effect within 1-3 hours. The other component of the drug (betamethasone dipropionate) is poorly soluble and is slowly absorbed from the depot formed at the injection site. The latter ensures a prolonged (up to 4-6 weeks) effect of the drug after administration.
Diprospan has high glucocorticosteroid activity, but unlike its predecessors (hydrocortisone, prednisolone, kenalog) it has a number of advantages:
- slight mineralocorticosteroid effect, rapid and at the same time prolonged powerful anti-inflammatory and analgesic effect;
— does not cause local fine-crystalline reactions;
- does not have a local degenerative effect on tissue;
- prescribed both once and repeatedly (if indicated).
3. Prednisolone
- a synthetic analogue of the steroid hormone of the adrenal cortex hydrocortisone. Glucocorticosteroids have anti-inflammatory, desensitizing, antiallergic, antishock and antitoxic effects.
Prescribed for neurodermatitis, dermatoses, eczema, allergic shock, etc. When treating the erosive-ulcerative form of lichen planus, it is used in combination with delagil. Prescribed with 2.5 mg and gradually reduce the dose until the drug is completely stopped.
Release form: tablets containing 0.001 g and 0.005 g of prednisolone.
4. Hingamin (delagil)
- antimalarial drug. Chingamine quickly causes the death of asexual erythrocyte forms of all types of plasmodium. The spectrum of action of hingamine is not limited to the effect on malarial plasmodium. It has an inhibitory effect on the synthesis of nucleic acids, the activity of certain enzymes, and immune processes. As a result, the drug has found wide use in the treatment of collagenosis (systemic lupus erythematosus, scleroderma, rheumatoid arthritis) and dermatoses (lichen planus). The drug is well and quickly absorbed and slowly released from the body.
Release form: tablets of 0.25 g; powder; ampoules of 5 ml of 5% solution.
In the treatment of erosive-ulcerative forms of lichen planus, it is used in combination with steroid drugs, 0.25 g 2 times a day for 1 month.
5. Nicotinic acid (vitamin PP, vitamin B3)
- belongs to the B vitamins. Nicotinic acid plays a significant role in the life of the body. It is a prosthetic group of codehydrase enzymes I and II, which act as hydrogen carriers and take part in redox processes.
Nicotinic acid is prescribed to normalize redox processes in the body and dilate blood vessels. For these purposes, vitamin PP is prescribed in the treatment of lichen planus.
Release form: powder and tablets of 0.05 g and ampoules containing 1 ml of 0.17% sodium nicotinate solution, which corresponds to 0.1% nicotinic acid. When treating lichen planus, vitamin PP is prescribed 0.05 g 1-2 times a day after meals for 1 month. Also injections of vitamin PP solution under the affected elements.
When using nicotinic acid orally on an empty stomach, redness of the face and upper half of the body, and dizziness may occur. Persons with hypersensitivity to nicotinic acid should be prescribed nicotinamide.
6. Retinol (vitamin A)
normalizes metabolic processes in the epithelium, the function of cell membranes, stimulates the regeneration of epithelial cells.
Vitamin A is found in animal products (butter, egg yolk, liver).
The daily requirement for vitamin A is 1.5 mg, or 5000 IU, for an adult.
When treating lichen planus, 8-10 drops of an oil solution of vitamin A are prescribed orally 2-3 times a day for a course of 1.5 months; locally in the form of applications of an oil solution of vitamin A to the affected areas 2-3 times a day for 15 minutes for a course of 1.5 months.
7. Oral gels Cholisal, Kamistad
Anti-inflammatory, analgesic effect.
Treatment results and discussion
After completion of the course of treatment, the patients had no complaints. When examining the oral mucosa, the disappearance of foci of exudation, hyperemia, complete epithelization of erosions, ulcers, and a significant decrease in lichenoid rashes were noted (Fig. 4).
Figure 4. Lichen planus, erosive-ulcerative form. Patient B., 46 years old. After treatment.
In 2 patients, due to stress, an exacerbation occurred 1-1.5 months after treatment (exudation, hyperemia and single small erosions appeared on the mucous membrane of the cheeks). These patients received a repeated course of general and local treatment.
When examining a group of patients 6 months after completion of the course of treatment, there were no complaints. Single papules were detected on the unchanged oral mucosa. The psycho-emotional state of the patients improved noticeably.
The treatment method we offer avoids hospitalization, which is a significant advantage. In addition, the effectiveness of local administration of diprospan makes it possible to prescribe gentle doses of prednisolone and reduce the risk of complications.
With local administration of diprospan with lidocaine, pain symptoms are quickly eliminated, which, in combination with the effect of daytime antidepressants, leads to a noticeable improvement in the psycho-emotional state of patients.
Thus, the effectiveness of treatment of the erosive-ulcerative form of lichen planus with total damage to all parts of the oral mucosa increases significantly due to the combined use of steroid drugs, as well as local therapeutic measures in the oral cavity. Our experience confirms the real possibility of treating patients with this disease in a clinic setting.
Symptoms of lichen planus in adults
Signs and symptoms of shingles last for weeks or months, and periodic relapses can occur for years, flaring up and dying down. The appearance of the lesions depends on their location.
In cutaneous LP, the lesions can be present anywhere on the skin, usually on the wrists, legs, palms and soles or trunk, and are 2 to 4 mm in diameter with angular edges, purple in color, and distinctly shiny under transverse light. These lesions tend to be symmetrically distributed and may also coalesce into rough, scaly patches. In rare cases, blisters may form. Moderate to severe itching is common, common, and difficult to treat.
There are several variants of cutaneous LP, which can present in different ways. The lesions may become large, scaly and warty (lichen hypertrophis), especially on the lower legs. New spots may appear at the site of minor damage to the skin, such as a superficial scratch (Koebner phenomenon). Sometimes degeneration (atrophy) of the skin can occur while lesions persist (lichen lichen), and some patients experience a lack of sweating due to degeneration of the sweat glands (anhidrosis).
Skin diseases
What diseases do dermatologists treat: KP’s guide to skin ailments
Unusual darkening (hyperpigmentation) or lightening (hypopigmentation) of the skin may occur in areas where wounds have healed.
Between 50 and 70% of patients experience symptoms related to the mucous membranes, moist, pink skin that lines the inside of the mouth, vagina, and esophagus. LLP on mucous membranes may appear as red, painful ulcers or lesions that have a reticulate, white pattern. Oral symptoms often occur before skin lesions develop. Oral symptoms may appear first, consisting of dryness and a metallic taste or burning sensation in the mouth, which may be the only sign of the disease.
Hair loss, although not common, can be one of the consequences of LP, which is called planopillaris. When hair loss occurs, it may affect small patchy areas of the scalp (atrophic symmetrical alopecia) or cause bald patches (frontal fibrosing alopecia). If tinea is not treated, hair loss becomes permanent due to scarring.
Nail lesions are present in 10 to 25% of patients with LP and tend to appear as roughness, vertical ridges or cracks, and thinning of the nail. This can eventually lead to scarring of the nail.
Trouble swallowing or pain when swallowing may indicate esophageal ringworm. It is important to treat esophageal disease because over time it can lead to a narrowing of the esophagus, called an esophageal stricture.
Some cases of the cutaneous form resolve over time, while the oral, genital, nail, and esophageal forms are more persistent and may worsen over time. Patients with LP have an increased risk of squamous cell carcinoma, especially of the oral mucosa, and should be monitored periodically.