According to official international statistics on the prevalence of fungal infections
For many years in a row, they have been ranked second among all skin diseases. They not only reduce the quality of life and cause discomfort, but also provoke allergic reactions, chronic inflammatory processes and many other pathologies.
Due to the peculiarities of their microbiological nature, fungal diseases can be actively transmitted from a carrier to a healthy person, and in addition to the skin, they can affect the nail plates, hair, internal organs and cause various pathogenic changes in them. Some fungi are prone to relapses, have a fairly long incubation period and very similar external manifestations. At the same time, some types of mycoses are treated only with oral medications, others - with cutaneous forms, so it is strictly forbidden to self-medicate and contact specialists at the first symptoms.
Dermatologists
- Ayvazyan Linda Volodyevna
Experience: 5 yearsDermatovenerologist, mycologist, trichologist
Rating: 0/5 — 0 votes
Make an appointment
- Osipova Daria Sergeevna
Experience: 14 years
Deputy chief physician for medical work. Dermatovenerologist
Rating: 0/5 — 0 votes
Make an appointment
At the Kutuzovsky Children's Center in Moscow, they perform tests for nail fungus with highly accurate results and at reasonable prices. The research is carried out using modern methods. The results will be ready soon. The price of nail scraping for fungus is indicated on the website.
References
- Russian Society of Dermatovenereologists and Cosmetologists. Federal clinical guidelines for the management of patients with trichophytosis. M.: 2015.
- Federal clinical guidelines. Dermatovenereology 2015: Skin diseases. Sexually transmitted infections. — 5th ed., revised. and additional - M.: Business Express, 2016. - 768 p.
- Verma S, Madhu R. The great Indian epidemic of superficial dermatophytosis: An appraisal. Indian J Dermatol 2017;62:227-36.
- Shen JJ, Jemec GBE, Arendrup MC, Saunte DML. Photodynamic therapy treatment of superficial fungal infections: a systematic review. PhotodiagnosisPhotodynTher. 2020;101774. doi:10.1016/j.pdpdt.2020.101774
Indications for analysis
Diagnosing nail fungus by visual signs is difficult. The clinical picture is similar to other lesions, and treatment must be different in all cases.
The doctor recommends getting tested for nail fungus if you have the following symptoms:
- Unnatural color of the nail plate. Diseased tissues lose transparency. The nail becomes yellow or turns brown. At the very beginning of the disease, the lesion may look like a small point, and as the fungus grows, the process spreads to the entire plate, to the skin, to neighboring fingers.
- Changes in nail density and mobility. Some types of fungus cause softening and delamination of the plate. Loose growths form. It is necessary to do a nail fungus test if part of the plate has moved away from the finger or has become noticeably thicker.
- Changing the shape of the plate. Fungi do not always lead to visible tissue changes. Patients often turn to a dermatologist with complaints of discomfort while wearing shoes. This occurs due to the deformation of the diseased nail - it becomes convex.
Risk groups and prevention of fungal infections
Fungal pathogens are found in minimal quantities on the skin of any person. But uncontrolled use of medications, especially hormones and antibiotics, can provoke their active growth and subsequent lesions. It should also be taken into account that deep mycotic infections can enter the body through open wounds. Compliance with sanitary rules for treating any injuries associated with a violation of the skin minimizes the risk of disease with systemic and visceral microfungi.
High humidity and constant above-zero temperatures are an ideal environment for the life and reproduction of microscopic fungi. Accordingly, the risk group a priori includes employees and visitors of swimming pools, fitness clubs, bath complexes, spa salons, as well as workers in laundries and catering establishments.
People with weakened immune systems, a depressed nervous system, a tendency to allergies, critical weight loss and metabolic disorders are also prone to fungal infections. Therefore, the most effective prevention is strengthening the immune system, impeccable adherence to personal hygiene rules and systematic examinations by a therapist and dermatologist.
Preparation for scraping
The doctor can take a test directly at the appointment if the basic requirements are met:
- Nail plates without decorative cosmetics.
- During the last month, the affected area was not treated with antifungal ointments and other drugs. Otherwise, scraping for nail fungus will give a false negative result. The study will have to be repeated.
- The nail was not trimmed for 6-10 days.
- There was no contact with water or detergents for 3 days.
Other problems
Nails change color not only due to fungal infection. The cause may be injury and lack of vitamins. This also happens when internal organs malfunction and due to diseases:
- Brittle nails are a sign of zinc and iron deficiency. Fragility can also indicate thyroid problems and a predisposition to diabetes. But it is possible that excessive fragility is your physiological feature.
- White spots and stripes are the consequences of microtraumas or a signal that you need to adjust your diet, check for heart failure or nervous exhaustion.
- Small depressions that strew the plate indicate psoriasis or arthritis.
- Deformations of the nail plate and grooves indicate that you are not eating well enough. These are common consequences of strict diets.
- Spoon-shaped, curved nails indicate problems with the endocrine system and a lack of iron.
- Nails are white at the base and almost brown at the tips - a symptom of kidney failure.
How the study is performed
To test for nail fungus, laboratory staff first dissolve the biological material in alkali. The keratin from the plate should go into the liquid phase. Then a preparation is prepared, which is examined through a microscope. Modern equipment allows us to examine the spores and mycelium of a fungal infection and make an expert opinion on the presence of the disease.
The advent of light microscopes has significantly accelerated the diagnosis of mycoses. Previously, a patient could take a scraping for nail fungus and wait for the culture result only after 3 weeks.
The price of a nail fungus test includes only an unambiguous conclusion about the presence or absence of infection. If more accurate information is needed, the doctor may prescribe PCR tests or other studies.
Methods for diagnosing fungal infections
The Northwestern Center for Evidence-Based Medicine offers traditional and innovative research methods. We carry out the following analyses:
Microbiological methods
Microscopy
– the most accessible and simplest diagnostic method. The study is aimed at confirming infection with superficial mycosis, for which biological material is taken from the patient, which is potentially considered infected: scraping of a pathologically changed nail or skin, eyelash, hair. Refers to qualitative analyzes and allows only to establish or refute the fact of infection. The study takes several days: the resulting material is processed (stained) in a certain way and submitted for microscopic examination to identify the elements of the fungus (spores, hyphae). Microscopy allows you to quickly confirm mycosis, but the type of pathogen and its quantitative concentration are established only for yeast-like and mold species. Therefore, it is often supplemented with cultural research (bacterial culture). The results of microbiological studies must be interpreted by the treating specialist.
Enzyme-linked immunosorbent assay (ELISA)
Linked immunosorbent assay
– a modern and highly reliable method for identifying fungi in a patient’s venous blood. It is a qualitative and quantitative method and can be used as a primary diagnosis and act as a confirmatory analysis of superficial and visceral mycoses.
The method is based on the detection and identification of immunoglobulin protein to a specific pathogen. Antibodies and antigens provide reliable information about infection with aspargillosis, candidiasis, cryptococci and dimorphic microfungi. The test result is interpreted as “positive” (there is an infection) or “negative” (there is no fungal infection). In some cases, the study may give a questionable result; as a rule, this happens if the patient has recently taken antibacterial drugs.
The study takes from 1 to 5 days. If it is necessary to identify the dynamics of the disease, ELISA is carried out every 14 days.
PCR
A highly accurate research method based on the polymerase chain reaction and taking no more than 3 days. It can be used to register any fungal pathogens, but has one drawback - targeted research. This means that the laboratory must obtain information about the specific species of microfungus whose spores and hyphae need to be identified. Blood, sputum, prostate secretion or urine can be provided for analysis, but in the last three options it is necessary to ensure maximum purity of the biological material. The most effective and appropriate in the complex diagnosis of systemic and visceral forms of fungal diseases. The study provides qualitative and quantitative results that are interpreted only by the attending physician.
Serological method
Classic studies in which IgG prepitins, enolase, proteinase and mannoprotein antigens are more often detected. The study is variable and can be based on the agglutination reaction, titration and RSC. They allow you to obtain information only about the fact of carriage of a mycotic infection or indicate a previously suffered fungal disease. The analysis may be based on blood serum testing. With extensive serodiagnosis, microfungus can be detected in other physiological fluids of the patient.
The results are interpreted by the treating specialist. In this case, the serological method is often used as a control study for subsequent adjustment of therapy and determining the effectiveness of treatment.
How often should you get tested?
A scraping is taken at the initial visit to the doctor to make a diagnosis. The doctor tells you how much a nail fungus test costs and what information he wants to get. Based on the results of the study, treatment is prescribed. If the lesion is small, repeat testing may not be necessary.
If the fungus has already led to deformation of the nail, a change in its structure, treatment control will be required. To do this, scraping is done several times at the discretion of the doctor. Based on the test results, the doctor will be able to adjust the treatment for the fastest and most sustainable results.
Tests for skin fungus
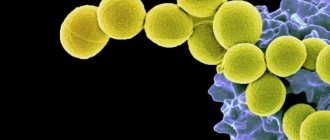
Fungal skin diseases (dermatomycosis) are the most common among skin diseases. Fungi have been known since ancient times; they are a special type of microorganisms that combine features of both plants and animals, and fungi feed on organic substances. They are tenacious, capable of forming spores and persisting in the environment for a long time, and grow very slowly. Therefore, fungal diseases can occur without manifestations for a long time, and their detection is not an easy task for doctors.
Mostly dermatophyte fungi are causative agents of superficial fungal diseases, in particular such as microsporia, trichophytosis (ringworm), epidermophytosis. They constantly live on the skin and hair of humans and animals, some in the soil. Human contact with fungi occurs. However, the skin is normally a powerful protective barrier and does not allow fungi to exhibit pathogenic properties.
The following factors contribute to the development of fungal skin diseases:
- mechanical damage to the protective barrier of the skin: cracks, microtraumas, including those resulting from cosmetic procedures.
- failure to comply with the rules of personal hygiene at home and when visiting public saunas and baths, fitness rooms, if individual towels, slippers, and hats are not used.
These factors are not leading; the skin will not allow the enemy to penetrate if the immune system works well. A decrease in local and general immunity of the body is a decisive trigger. This is facilitated by:
- Genetic causes (congenital immunodeficiencies)
- Lack of vitamins and microelements
- Chronic skin diseases
- Endocrine diseases: diabetes mellitus primarily, thyroid dysfunction, obesity, other hormonal problems
- Long-standing chronic diseases (gastrointestinal tract, lungs, heart; tuberculosis, AIDS)
- Long-term use of antibiotics, glucocorticoids, antitumor drugs.
If the fungus has overcome all the obstacles in its path, a disease develops. The peculiarity of skin fungi is damage to the stratum corneum (surface) layer. Fungi feed on the keratin that is part of it. Skin, nails and hair are affected.
How do fungal skin diseases manifest?
Since only the superficial layers of the skin are involved, manifestations may include:
- Itching and peeling skin without spots
- The formation of red spots with clear edges in the form of one or multiple foci, usually accompanied by peeling and itching
- Nails become thicker, deformed, and split
- Hair loss due to trichophytosis
- Inflammation of hair follicles with crusting and flaking
Manifestations are typical for many skin diseases. The examination data does not allow us to determine whether there is a fungal infection of the skin or not.
To establish a diagnosis, the following laboratory methods are used:
Microscopic examination of skin, nail plates and hair for the presence of pathogenic fungi (performing time 2 days)
An important point for the correctness of the study is to take material at the border of healthy and affected tissues, where there is a higher probability of detecting active growth of fungi. The microscopic method allows you to see a pathological fungus under a microscope or exclude its presence, but does not allow you to determine the type of pathogen. Identification of fungal mycelium is a criterion for confirming active mycosis. The presence of only spores requires detailed study and confirmation by other methods.
Culture for fungi (causative agents of mycoses) (up to 30 days) is a more accurate study. Skin scrapings, nails and hair are placed in special media enriched with nutrients specifically for skin fungi. The doctor observes the growth of fungi for up to a month, since they grow very slowly and it is this period that allows an adequate examination and not to miss the disease. Thanks to culture, the specific type of dermatophyte fungus is determined, which makes it possible to prescribe the correct antifungal drug.
Please note that the malasezia furfur fungus, the causative agent of dandruff in animals and humans, does not grow in crops. This is his peculiarity!
In case of fungal diseases, determination of sensitivity to antifungal drugs is carried out only for scientific purposes in order to introduce a new medicine, since this is a long, labor-intensive process and it is impractical in medical practice. The fact is that known antifungal drugs act on certain types of fungi, and when a fungal disease is confirmed, the doctor will not wait for further progression of the process for another month, but will prescribe a drug depending on the type of fungus determined as a result of the analysis.
How to properly prepare for research?
Skin scrapings are performed only by a doctor. Hair and nails can be collected independently and placed in a special container, if possible at the border of healthy and affected tissue. The study is carried out before starting to take antifungal drugs or 2 weeks after the end.
Get examined competently and in a timely manner with the KDL laboratory!
Diagnosis and choice of doctor
Nails are a derivative of the skin, so the examination should begin with a visit to a dermatologist. At the first stage, the doctor will conduct a visual examination. Next, you will need to undergo general tests and conduct laboratory tests directly on the nails.
At the medical center, they will do a microscopic examination of the plates for the presence of pathogenic fungi, take a scraping and conduct a screening. All types of diagnostics are carried out in our own laboratory in the shortest possible time - from two working days. The clinic is attended by an experienced dermatologist who will find the cause of the problem. If necessary, refer you for consultation to other specialists.