The article was prepared by a specialist for informational purposes only. We urge you not to self-medicate. When the first symptoms appear, consult a doctor.
Bone calluses appear after a fracture during bone tissue restoration. Such calluses are not a pathology; they are small areas of compaction. Bone calluses should not be confused with regular calluses.
What is a callus
A callus is a conical thickening of the skin that occurs in areas of constant friction or pressure. Most often, calluses appear on the feet (heel, big toe, side of the foot) and on the hands. In men, a callus may appear on the penis due to frequent wearing of too tight underwear.
The main symptom of the appearance of callous formations is the formation of tubercles of rough skin. Depending on the location and appearance, there are several types of calluses:
- dry;
- wet;
- bone.
A dry callus is a small area of thickened, dead skin that is yellowish in color. A wet callus has a thinner surface and is often filled with lymphatic fluid. Callus occurs during the process of bone regeneration after fractures. Separately, bloody calluses, core calluses, and calluses are also distinguished.
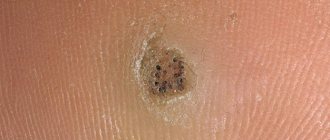
Core (root) callus is a type of dry callus and is distinguished by the presence of a thickened keratin core. The external manifestation of a root callus is similar to that of a plantar wart, so a dermatologist can make an accurate diagnosis after performing a dermatoscopy.
Calluses (corns) are wide, flat thickenings of the skin that do not have a hard center. Corns on the feet and hands rarely cause pain when pressed.
A callus with blood is a type of wet callus filled not only with lymph, but also with blood. A callus occurs when blood vessels are too close to the surface of the skin that has been subjected to friction.
Symptoms
Signs of a fracture and secondary fusion with the formation of periosteal callus are:
- local pain that subsides;
- crepitus – a characteristic crunching sound, especially when trying to move a limb;
- disappearance of pathological mobility;
- distortion of the shape and structure of the bone during the formation of a paraosseous callus, which may look like a large protrusion.
Callus after a clavicle fracture
After a clavicle fracture, a natural process of formation, first of osteodin, then of callus, also occurs, which usually takes up to 2 months. The causes of fractures are most often falls, sports injuries, road accidents, and are also possible in newborns during birth.
Callus after a clavicle fracture
After the collarbone has completely fused, the callus should resolve, but in some cases this does not happen, as in the photo of the callus presented above.
Causes of calluses
In response to constant friction and pressure, cells begin to synthesize increased amounts of keratin, the skin's protective protein. With calluses, keratin can form a plug in the deep layers of the skin. The main reasons for the formation of calluses on the feet and hands are:
- wearing shoes of the wrong size;
- foot deformities (hammer toes, bunions, bone spurs);
- chafing of the skin due to professional activities (musicians, weightlifters, artisans);
In tight shoes, the skin of the foot is strongly compressed, and in too loose shoes, it slips and rubs, which can cause internal (core) calluses to develop. Calluses on the foot due to toe deformities occur due to improper weight distribution. Due to frequent rubbing of the skin of the hands with professional instruments (strings, bars), calluses appear on the hands.
What to do if a bunion grows on your foot?
The problems for owners of the unfortunate bone are not only cosmetic. Patients often complain that it is difficult for them to choose shoes and that their legs quickly get tired when walking. In addition, hallux valgus is often accompanied by such troubles as the formation of painful calluses and corns. Conclusion? Something definitely needs to be done.
Let’s say right away that the answer to a question like “Is it possible to cure a bunion with iodine?” negative. This also applies to other home remedies; they can only temporarily reduce pain.
The first step is a visit to an orthopedic doctor. He will conduct the necessary diagnostics and prescribe treatment, which can be conservative or surgical. Today, doctors have enough tools in their arsenal that allow them to do without surgery. Surgical intervention is necessary only in very advanced cases.
Treatment of a hallux valgus defect is long and difficult. It consists of selecting the right orthopedic insoles, prescribing physiotherapy, anti-inflammatory and painkillers, and massage sessions. In addition, the doctor will recommend a complex of physical therapy. In order for therapy to lead to results faster, it is advisable to go to the clinic in the early stages of the disease.
Dry and wet calluses
Dry calluses are keratinized areas of skin that form in places where bone presses on the skin of the feet (tops of the toes). If you frequently wear tight shoes, dry subungual callus may form.
Wet (water) calluses are whitish-gray in color and have a softer texture because they form in areas of increased sweating on the feet and hands. Water calluses often form between the fingers and toes. If a wet callus on the foot is damaged, an infection can enter the wound, so it is important to treat the damaged area of skin with antiseptic agents.
What can the patient do?
A lot also depends on the patient. Good support for treatment will be:
- wearing comfortable, non-tight shoes with low heels;
- constant use of orthopedic insoles;
- alternating activity and rest - especially important for those who work on their feet;
- weight loss if necessary.
These measures are also good for preventing hallux valgus. One last useful thing: walking barefoot on pebbles, sand, and uneven surfaces has a good effect on the condition of the feet.
You can get professional help for hallux valgus in our medical center. Come, we use modern methods with proven effectiveness in diagnosing and treating bunions!
Callus
Callus formation is an important step in the process of bone tissue repair after injury because it helps connect the parts of the damaged bone. After a fracture, the callus is enriched with calcium and gradually turns into normal bone tissue.
Due to insufficient immobilization or poor circulation at the fracture site, callus may form too slowly (delayed fracture consolidation). Its slow formation can cause the bone to heal incorrectly and cause pain.
Causes
Diseases that contribute to the development of bone calluses, disruption or slowdown of the processes of true fusion:
- old age;
- endocrine pathologies, for example, hyperparathyroidism and diabetes;
- osteoporosis;
- obesity;
- pregnancy;
- radiation sickness;
- tuberculosis;
- syphilis;
- amyloidosis and chronic inflammatory diseases;
- general exhaustion;
- severe anemia ;
- hypoproteinemia;
- avitaminosis.
How to get rid of calluses?
To get rid of calluses, it is enough to temporarily eliminate activities that cause chafing of the skin. You can remove dry calluses manually: you need to steam the skin of your hands and remove rough areas using pumice. In addition, the surgeon may recommend the use of keratolytic agents, which soften the skin. You cannot remove calluses on your own with the help of keratolytics if you have diabetes or pathologies of the immune system, since after removal a wound may form through which an infection can enter the body
You should see a doctor if the callus is painful to step on or touch, as this symptom may indicate the presence of a heel spur, a calcified growth on the surface of the bone. Removal of the callus core is performed by a doctor because removing the callus at home is ineffective and unsafe.
To quickly cure a water callus and avoid its damage, it is necessary to reduce the contact of the inflamed skin with the shoes: you can put a foam insert or a cotton ball between your toes. If the water callus bursts, the doctor prescribes the use of wound healing agents with an antiseptic effect.
Callus removal is performed surgically using local anesthesia. First, the surgeon cuts off the keratin growth on the skin, and then pulls out the rod. To speed up the healing process and prevent the wound from becoming infected, it is recommended to wear a sterile dressing for several days after the callus removal procedure. The surgeon also prescribes local use of antiseptics for two to three weeks after removal of the callus.
Tests and diagnostics
The main way to identify callus is x-ray examination. When collecting data, the patient’s complaints, medical history and the nature of the dysfunction of the limb are taken into account. In this case, it is necessary to trace the fracture line.
In severe diagnostic cases, radiographs are additionally repeated in various positions, as well as CT and MRI.
The speed and quality of callus formation become quite important for the prognostic picture. Osteodic calluses that form on the 10-20th day after a fracture are X-ray negative. Radiographically, callus becomes visible from about 4 weeks due to the fact that the tissue in it calcifies. Severe callus can be detected 3 months after injury.
Callus or wart?
A wart is a small growth that is caused by the human papillomavirus (HPV). Calluses and warts may be similar in appearance. A wart can be distinguished by its more granular structure and location (warts can appear on any part of the body). To accurately make a diagnosis (callus or wart) and select treatment, the surgeon can conduct a dermoscopic examination and additionally prescribe a test for human papillomavirus (HPV).
Mechanism of infection
A callus with pus most often appears when the blister is not treated and antiseptic rules are not followed when treating it. An open callus is a gateway to infection, so it must be isolated from the surrounding aggressive environment.
Purulent exudate (liquid inside the callus) consists of dead leukocytes that protect the body from pathogenic bacteria and dangerous infections. Its appearance indicates that the immune system is working properly. But in our body there is a single network of blood vessels, thanks to which oxygen and nutrients reach the organs and tissues. The same transport system can lead to the spread of infection, which can lead to sepsis (blood poisoning), embolism (blockage of blood vessels) and gangrene.
Treatment with professional methods
It is recommended to ask your doctor how to treat a purulent callus. This disease is dealt with by specialists in purulent surgery; only a professional will be able to properly open and drain a festering blister in order to prevent infection. If improperly processed and incompletely pumping out the contents, purulent calluses can recur, and the infection can spread through the blood vessels throughout the body. After the procedure, broad-spectrum antibiotics are prescribed to prevent infection.
Three main ways to remove purulent callus in a medical institution:
- If the callus is cored, the root is drilled out by a surgeon using a specially selected cutter of a certain size. Antiseptic drugs are instilled into the resulting wound to prevent re-festering.
- The laser immediately coagulates (cauterizes) nearby blood vessels, so pathogens do not spread through the blood vessels. Healing time is 3-5 days
- Cryotherapy is the most effective treatment method. During the procedure, healthy skin is not affected; only the purulent callus and its contents are removed. Usually carried out in advanced cases when a lot of pus has accumulated.
Removal of callus of the first toe Hallux Valgus (one foot)
Hallux Valgus is a deformity of the first toe. There are many reasons for the problem: the main reason is wearing “wrong” shoes (too narrow shoes, high-heeled shoes), flat feet and foot deformities, hereditary causes. There are 3 degrees of the problem, and if in the primary stage it is possible to solve the problem with non-surgical methods, then in case of serious deformation there is only one way - surgery on the big toe.
The callus removal operation is performed under local anesthesia. Our clinic uses low-traumatic techniques. Traces from the manipulation are invisible, but, as with any operation, rehabilitation is necessary. Since the procedure is performed on the foot, you need to understand that restrictions will apply to shoes, walking, and physical activity.
During the consultation, the plastic surgeon assesses the extent of the problem and prescribes additional studies to exclude contraindications to the procedure. For the patient’s comfort, this operation can be performed in 2 stages: first on one leg, after a month on the other. This will allow the patient to spend the rehabilitation period more comfortably. Most often, the procedure is performed in the summer, when wearing open shoes is possible.
Main stages of the operation:
- Treatment of the surgical area with iodopyrone solution. Local anesthesia of the surgical area through a thin needle. Only at this stage can the patient feel discomfort from anesthesia injections. The further procedure is completely painless.
- A small incision is made in the area of the first toe. Dissection of tissues and separation of correction zones.
- Correction is carried out using special equipment (including ultrasound).
- A cosmetic suture is applied. The operation takes only 30-45 minutes.
Next, the patient is sent home with recommendations for further behavior. In the first month, it is important not to injure your foot, not to wear narrow closed shoes, and to give up heels (wearing high-heeled shoes forever is not recommended). The sutures are removed after a few days, it is important not to put stress on the foot - restrictions on physical activity also apply to walking.
The procedure is performed for both women and men. Most often, it is in women over 40 years of age that the problem of hallux valgus manifests itself. Rostov is a city with a fairly warm climate, so operations to correct callus in our clinic are carried out in late spring - autumn.
You should not neglect the problem, because it is not only aesthetic in nature, but also physiological. Many patients begin to experience pain in the foot area, which gets worse every year. All you need to do is sign up for a consultation with our specialists and solve the problem forever.
Tips to avoid infection
A purulent callus requires long-term and unpleasant treatment, so it is better to avoid its appearance. To do this, just follow these simple tips:
- Choose comfortable shoes and socks of the appropriate size,
- Give preference to shoes made from natural materials, do not wear synthetic socks,
- Pay attention to the health of the skin on your feet: lubricate with Vaseline the places most susceptible to rubbing calluses.
- If a blister appears, do not neglect treatment: be sure to treat it, cover it with a band-aid to prevent infection,
- Watch your weight - obese people have a higher risk of developing purulent calluses.