Papilloma viruses are the only group of viruses today for which scientists have proven the induction of cancer tumors. Moreover, HPV is the most common sexually transmitted infection; more than half of adults are infected with it. Find out how the papilloma virus manifests itself and how to treat it.
Appointment with a gynecologist - 1000 rubles. Appointment with a urologist - 1000 rubles. Removal of tumors - from 500 rubles. Consultation with a doctor based on the results of ultrasound and tests - only 500 rubles. (at the request of the patient).
MAKE AN APPOINTMENT, TEST OR ULTRASOUND
What is papillomavirus, papillomas, condylomas
The content of the article
Human papillomavirus infection (HPV) belongs to the genus A of the Papovaviridae family and is transmitted primarily through sexual contact, infecting epithelial (cover) cells - the skin, mucous membrane and urogenital area. Infection of the skin and genital organs occurs through microtraumas. The papilloma virus is contained in the urethra, Bartholin's glands and seminal fluid. The development of malignant tumors of the penis, vagina, and cervix is associated with human papillomavirus.
HPV strains, of which science knows more than 100, behave differently in the cell. Some exist separately from chromosomes, others are able to integrate into the cell genome (they most often cause complications). When the viral DNA is inserted into the nucleus of the host cell, it controls the cell's genetic material, leading the cell to malignant transformation. During the replication cycle, the human papillomavirus genome expresses 8–10 protein products. Oncogenicity is determined by proteins E6 and E7. It is difficult to kill the infection - the virus remains viable at a temperature of 50 degrees. From 30 minutes.
The virus infects stem cells located in the basal layer, and they transmit the infection to the surface epithelial cells. Superficial dividing immature cells are especially susceptible to HPV, which explains the high risk of oncogenes affecting the vulva, lower part of the vagina and cervix.
The most common visual manifestation of papillomavirus is papillomas. The formation got its name from the Latin papilla - nipple + Greek oma - tumor. Papillomas can develop into cancer. The development of oncology can be prevented by monitoring the development of papillomas and removing them in a timely manner.
A type of papillomavirus in women and men is genital and flat condylomas that develop on the genitals. They must also be removed.
A complication of the virus is a precancerous condition - cervical dysplasia and its logical conclusion - cervical cancer. You can avoid cancer by treating dysplasia. Treatment also involves removing the affected layer of cells.
Screening - general examination
Many women are interested in what HPV screening is. First of all, it should be pointed out that this is a qualitative analysis that allows you to detect cervical cancer in the early stages, as well as find out about the presence of dangerous types of viruses in the body of a particular person.
In women, HPV screening is done directly during a gynecological examination. In this case, the doctor takes a smear, which is subsequently tested in a laboratory. If a human papillomavirus infection is detected as a result, the woman should undergo a more thorough examination, including to identify pathological changes in tissue.
Several other methods are actively used today to establish the diagnosis of IF.
- PCR. Its purpose is to identify the DNA of the pathogen in biological material: blood, urine, secretions. Therefore, it is possible to find out which stamp is present.
- Genotyping. Helps determine whether the infection has an initial form or a chronic one.
- Digen test. Quantitative method indicates the amount of virus.
It is up to the doctor to decide which test to use and when exactly to screen for HPV.
How papillomavirus is transmitted, risks
Papillomavirus enters the human body in different ways, the probability of infection is 60%. You can get an infection in the following ways:
- Sexually, regardless of the type of sexual relations - oral, genital and anal. The presence of genital warts in a partner guarantees infection by 98-100%.
- Contact household - in the case of using a shared towel, washcloths, etc. The virus can also be transmitted through saliva during a kiss.
- Through wounds - a violation of the integrity of the skin and mucous membranes - an open gateway to the body.
- Infection of a child during the passage of the birth canal - children suffer from rare forms, papillomas grow in the nasopharynx and sinuses. Recent studies have shown that children born by cesarean section also become infected - this may indicate that the virus is able to penetrate the placenta.
Infection does not always guarantee the development of the disease. HPV causes disease in the body in 50% of cases, the rest are limited to carriage of the infection: a strong immune system can keep the virus in numbers that are not dangerous to the body. The incubation period ranges from a year to 20 years, with an average of 3-5 years.
The development of the disease is provoked by hormonal imbalances, immunodeficiency states, and sexually transmitted infections (STDs, STIs). Any condition that reduces immunity increases the risk - pregnancy, bad habits, chronic diseases, stress, etc.
It should be understood that infection of epithelial cells is a necessary but not sufficient factor for the development of oncology. According to Professor V.A. Molochkov, a well-known and respected scientist in the world of medicine, a number of other factors are necessary for the development of irreversible neoplasia:
- active expression of genes E6, E7 of highly oncogenic types hpv16 and hpv18;
- induction of estradiol metabolism to 16-OH;
- multiple damage to chromosomal DNA in an infected cell.
The first stage of CIN I neoplasia is expressed by active copying of the virus and its asymptomatic course. Tumor development is stimulated by the interaction of papillomavirus with cytomegaloviruses, trachomatis, mycoplasmas, ureaplasmas, and herpes simplex virus type 2.
Reasons for virus activation
A jump in the development of infection is observed under certain conditions:
- hormonal changes in a woman’s body, for example, during pregnancy, lactation, and menopause;
- excessive physical activity;
- chronic fatigue;
- alcohol abuse, smoking;
- frequent illnesses;
- chronic diseases;
- STD;
- regular stress;
- lack of vitamins and nutrients;
- taking antibiotics;
- abortions.
With frequent changes of sexual partners or unprotected sexual intercourse, the infection enters the body, but begins to develop if at this stage the person’s immunity is reduced. For this reason, HPV may not manifest itself for a long period.
As soon as immunity is significantly reduced, the virus begins to actively multiply, which provokes the appearance of excess tissue in the genital area.
The above factors contribute to a decrease in immunity. By themselves, they are not the cause of the development of HPV genotype 66.
Important numbers: the statistics are scary
- In the last 10 years, the number of people infected with hpv
has increased 12-fold. - HPV ranks second after genital herpes among all female infections and is found in 70% of adult women.
- Papillomavirus is the cause of all cases of cervical cancer.
- HPV is associated with 50% of anogenital cancers.
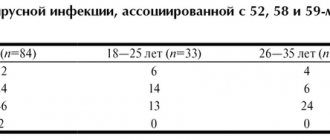
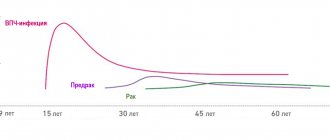
- The greatest risk of infection is between the ages of 18 and 25. The peak age for development of cervical dysplasia is 30 years, and cervical cancer is 45 years.
Why diagnose a disease?
Timely detection of the virus in women or men makes it possible to save a person from death. It is very difficult to identify the presence of carcinogenic types, because the problem may not manifest itself from the outside for a long time.
Having received accurate results, the doctor can find out whether condylomas pose a threat, whether they lead to the appearance of degenerated tumors, and whether they should be removed at all.
Timely diagnosis helps prevent the development of cancer, and if it is present, select the most effective control regimen.
Who should be screened?
All women over 30 years of age should be tested for HPV. If no carcinogenic types are found in them, then it is worth repeating such an analysis at least once every 2-3 years.
You also need to donate blood to determine the virus:
- during pregnancy;
- with severely reduced immunity;
- if a person is struggling with signs of having HPV;
- after unprotected contacts, blood transfusion.
Also, all people who have already been diagnosed with the disease should undergo such an analysis from time to time.
Types of HPV
Scientists know more than 100 types of papillomaviruses. A third of them infect the human urogenital tract, affecting the skin and mucous membranes of the genital organs. A fifth of the viruses in this group have not yet been studied and may well present new unpleasant surprises.
The papilloma virus is classified according to its oncogenicity and area of damage:
- Non-genital - nasopharynx, mouth, sinuses, vocal cords, lungs;
- Affects the organs of the urinary system - ureters and bladder, urethra, renal pelvis;
- Genital in women - affects the mucous membranes of the external genitalia, the vestibule of the vagina and the vagina itself, the perianal area, the cervix, the perineum;
- Genital in men - affects the glans penis, foreskin, frenulum, coronary sulcus, shaft of the penis, scrotum, groin skin, pubis, perineum, perianal area. The external opening of the urethra in men is affected in 20-24% of cases.
Based on oncogenicity, HPV can be divided into:
- HPV low risk - type 6,11,42,43,44;
- HPV average risk 31,33,35,51,52,58;
- HPV high risk 16,18, 45, 56.
The most dangerous types of HPV papillomavirus (hpv) - those belonging to the high cancer risk group - are 16, 18, 31, 33, 35, 39, 45, 51, 52. They cause genital cancer.
How dangerous the papillomavirus is for men and women can be understood by looking at the table of diseases associated with HPV activity.
Is screening reliable?
Today it is difficult to find a more reliable and affordable way to detect the HPV virus than screening. It only takes a few days for specialists to point out the presence of potentially dangerous factors.
Modern private clinics have all the necessary equipment, indicators and tools that allow the test to be carried out with the highest quality possible. For ease of use of the PCR method and ease of interpretation of the results, recalculation into Digene units occurs. Therefore, the probability of error is very low.
Diseases caused by HPV (table)
| Disease, clinical manifestation | Type hpv |
| Skin diseases | |
| Plantar warts | 1,2,4 |
| Common (simple) warts | 2, 4, 26, 27, 29, 57 |
| Butcher's warts | 7 |
| Flat warts | 3, 10, 28, 49 |
| Verruciform epidermodysplasia (hereditary disease - verrucous dysplasia) | 2, 3, 5, 8, 9, 10, 12, 14, 15, 17, 19, 20, 36, 37, 46, 47, 50 |
| Diseases of the genital mucosa | |
| Flat condylomas, cervical dysplasia | 6, 11, 16, 18, 30, 31, 33, 39, 40, 42, 43, 51, 52, 55, 57, 61, 62, 64, 67 |
| Condylomas acuminata | 6, 11, 42, 54 |
| Cervical cancer, genital cancer, vaginal cancer, anal cancer | 16, 18, 31, 33, 35, 39, 45, 51, 52, 54, 56, 66, 68 |
| Diseases of the mucous membranes | |
| Epithelial hyperplasia of the oral mucosa | 13, 32 |
| Neck, lung and head cancer | 2, 6, 11, 16, 18, 30 |
| Respiratory tract papillomatosis | 6, 11, 30 |
One patient can be infected with several types of papillomavirus at the same time, which is usually the case.
So what is it: HPV 16 genotype in women?
All papillomaviruses are conventionally divided into three main groups depending on their oncogenic danger:
- non-oncogenic, causing flat/plantar/vulgar warts (types 1, 3, 2, 4, 41, 10, etc.), not capable of causing malignant transformations
- low risk, causing the development of anogenital warts (otherwise called genital warts), resembling characteristic cauliflower buds, epidermoplasia verrucous, laryngeal papillomatosis (types 5, 17, 12, 6, etc.), can extremely rarely, under very “favorable” conditions, cause malignant process
- high risk, capable of causing neoplastic changes in women in the area of the uterine cervix, bowenoid papulosis (HPV types 16 and 18, 33, 31, 39, 35, 58, 56, 45, 68, 59, 52, 51), have been proven to provoke the overlap of various factors oncological processes
Thus, the answer to the question of whether HPV 16 infection is dangerous for a woman’s health has been determined: it is this type of virus that poses a serious threat.
However, the presence of a pathogen does not mean the presence of a disease.
In addition, HPV infection has an interesting feature: the ability to self-heal.
That is why in a situation where a certain amount of HPV type 16 DNA is detected in women during laboratory tests, it is important not to panic.
You just need to follow your doctor's recommendations and undergo regular examinations with a gynecologist.
Symptoms of papillomavirus
HPV infection can be asymptomatic or give the following symptoms:
Genital warts (genital warts)
Fibroepithelial (skin) neoplasms with a thin stalk or a broad base. They can be single or merge, forming a growth that looks like a cauliflower head. Condylomas can become inflamed and bleed when injured, as they contain blood vessels that feed them.
Condylomas can be found on the clitoris, labia minora, urethra, vagina, cervix, around the anus and in the anus. Exophytic forms of OC are a consequence of the activity of benign types of the HPV virus - 6, 11. Endophytic condylomas (flat and inverted) grow on the cervix and initially do not give symptoms. Detected during extended colposcopy. Genital warts affecting the lips, tongue and palate are visible during routine examination.
People with HIV and during pregnancy develop very large genital warts. Giant Buschke-Levenshtein condyloma is not uncommon.
- Anal warts.
Anal warts can be found up to the dentate line of the rectum. At first they do not cause discomfort, but over time they itch, hurt, and smell unpleasant. - Urethral warts.
In women, the external urethral opening is affected in no more than 8%. Such warts are easily identified by a gynecologist. Deep damage to the urethra (urethra) cannot be determined visually, but the disease gives symptoms of sluggish urethritis. Urethral warts in men cause a split urine stream associated with a narrowing of the urethral opening.
Flat condylomas
Flat condylomas do not protrude above the surface of the mucous membranes, which is why they got their name. These formations have a high oncogenic potential. Most often, flat condylomas are located on the cervix and vaginal mucosa. Flat condylomas can only be detected by colposcopy.
Dysplasia, cervical cancer
Dysplasia is a tissue pathology associated with the modification and degeneration of cells. This is a precancerous condition. There are 3 degrees of the disease, all of which are detected by colposcopy. Stages 2 and 3 require surgical treatment. Cervical dysplasia is preceded by cervical erosion.
Cervical cancer is a consequence of dysplasia. It is the most common tumor of the female reproductive organs. It may be asymptomatic or cause pain, bleeding and other symptoms characteristic of problems with the female reproductive system.
Collection of biomaterial and preparation
The material that is taken for HPV analysis is epithelial cells, which are taken from the cervical canal in women, and from the urethra in men. For this purpose, a small diagnostic brush is used, which is inserted into the endocervix or into the urethra. After removing the brush, epithelial cells settle on its villi. The instrument with the resulting biopsy is lowered into a sterile container and sent to the laboratory. For the patient, the collection of material does not cause any particular discomfort, but if HPV is detected in the analysis, then the benefits of it significantly outweigh the discomfort.
You need to prepare specifically for an HPV test. Before the examination, you are not allowed to use antibacterial and antiseptic products for intimate hygiene, douche, use vaginal suppositories, or have intimate relations for two days. If the patient is undergoing antibacterial therapy or taking anticoagulants, you need to notify the doctor about this, the drugs may distort the result. Before collecting biomaterial, you need to urinate.
Papilloma virus - diagnosis
Human papillomavirus can be detected in its early stages only by laboratory methods. The infection can be detected visually only when condylomas or papillomas appear. If HPV is suspected, the following are prescribed:
- Gynecological examination
or examination by a urologist with taking smears for an HPV test. If condylomas are detected, urethroscopy is performed. In case of cervical erosion, the gynecologist must take a smear for oncocytology. - If HPV is detected, a colposcopy is required - examination of the vagina and cervix with a gynecological microscope - colposcope. The doctor uses special tests to exclude hidden pathologies.
- Colposcopy with biopsy.
Indicated for all women with neoplasia. At the same time, coloring and exposure to suspicious areas is carried out. A sign of APC may be whitish areas formed after treatment with vinegar, uneven accumulation of iodine when exposed to Lugol's solution, a mosaic pattern, and protrusions of the epithelium. - Histological and cytological examination
- assessment of the cellular composition, and the cells themselves, for atypicality (cancer). - PCR – search for traces of papillomavirus DNA. This is the most accurate and diagnostically informative analysis that detects the papilloma virus in men and women and specifies its type.
To assess the viral load, a quantitative HPV test is recommended, which determines the critical concentration of the virus associated with the risk of malignancy of tumors. The analysis is also carried out to assess the effectiveness of treatment.
What to do if dangerous types of HPV are identified?
The risk of detecting dangerous types of HPV in an individual person is low.
In most people, no variant of this virus is detected at all.
If the patient is infected, then with a high probability it is a harmless type of HPV.
Low-oncogenic varieties are much more common.
If you are unlucky and have been diagnosed with highly oncogenic HPV, you need to look at its quantity.
If it is small, no treatment is required.
Most likely, your body has already begun to get rid of the virus, and soon it will no longer be detected.
It's worse if its concentration is high.
In this case, the following is necessary:
- additional tests;
- treatment;
- dynamic observation.
A smear is taken from the patient for oncocytology.
Most often, this study is carried out not after HPV genotyping, but simultaneously with this test.
Based on the results of these two tests, a decision can be made about the need for colposcopy.
It is needed to identify areas of altered epithelium (precancerous processes).
In turn, the results of colposcopy (examination of the cervix) may require a biopsy.
This is a procedure in which a piece of tissue is taken and sent for histological examination.
Based on its results, both a malignant tumor and a precancerous process of stages 1-3 can be diagnosed.
Stage 1 is reversible, while stages 2-3 require cauterization to prevent cancer.
But precancerous processes develop very slowly.
If antiviral treatment is carried out in time, the virus disappears from the body and the cervical epithelium is restored.
Patients must be monitored.
They are tested every six months to assess whether the concentration of the virus is increasing or decreasing.
To eliminate it, antiviral and immunomodulating drugs are used.
Treatment of papillomavirus
Unfortunately, medicine is not yet able to completely rid the body of the virus. Therefore, the task of the doctor and the patient is to deal with the consequences in a timely manner. It is recommended to remove all warts and treat precancer and cancer stages. According to recent studies in the USA, the human immune system is able to cope with HPV on its own within 2 years after infection in 90% of cases. If this does not happen, treatment is strictly necessary. Papillomas are removed using the following methods:
- Surgical removal
is an outdated but effective method. Recommended in exceptional cases. - Electrocoagulation
– cauterization of affected areas with electric current. Not everyone likes the method, as it can also affect healthy tissue. - Laser coagulation
- laser cauterization - is the most modern and effective method that gives a minimum of complications. - Cryodestruction with liquid nitrogen
differs from other methods in that the pathological growth is affected by cold. Requires a lot of experience from the doctor. - Chemical cauterization
- the doctor acts on the diseased area with concentrated acids or alkalis. The method can also affect healthy skin - the chemical will leave a scar. - The radio wave method
is the most expensive, but the best. Does not cause pain, complications, bleeding. Does not leave scars.
You can read more about methods for removing tumors in the “Low-traumatic operations” section.
After removal, antiviral treatment and means to restore and strengthen the immune system are prescribed.
How to prevent disease
Considering that HPV does not manifest itself at the incubation stage, it will be difficult to detect the virus without additional examination. To avoid infection and the development of the disease, you should follow simple rules:
- casual sex should be avoided;
- It is recommended to use barrier contraception during sex;
- Frequent changes of sexual partners are undesirable.
Intimate hygiene and maintaining a high level of immunity - these factors also help prevent the development of the disease.
Prevention of papilloma virus
You can prevent the appearance of warts by maintaining personal hygiene. You should not touch other people's papillomas, condylomas, etc. You can protect yourself from genital warts by barrier contraception (using a condom), but if the formations are on external tissues, this will not help. The most effective method of protecting against HPV is strengthening the immune system.
Girls and boys are recommended to get vaccinated against HPV. The vaccine prevents the occurrence of cervical cancer, vulvar cancer, vaginal cancer, genital warts and other diseases associated with papillomavirus. There are three types of vaccines against papillomavirus. In Russia, the drug Gardasil is recommended, directed against 4 types of hpv (16, 18, 6, 11).
The vaccine is given three times, starting at age 9 and before the start of sexual activity. Women can get vaccinated up to 26 years of age, but the drug will not work against viruses that are already in the body.
Where does HPV type 16 come from in women?
According to WHO, up to 80% of the population is infected with HPV.
But only about 10% of those infected have clinical manifestations.
The answer to the question of how HPV 16 is transmitted to women is well known: the main route of infection is sexual contact.
Including anal-genital and oral-genital, with an infected partner.
HPV has a very high prevalence: almost 80% of women by the age of 50 have been infected at least once.
At the same time, the virus has a tendency to self-eliminate.
So it is not possible to establish the probability of infection after a single contact.
This is why it is so important not to neglect preventive measures during casual sexual acts.
Infection of a child by the mother at the time of birth is possible with viruses of types 6 and 11 - the cause of such a disease in children as respiratory papillomatosis.
No other types of virus, including HPV type 16, usually cause problems during pregnancy in either women or newborns.
There are only isolated cases of infection of newborns by mothers with bowenoid papulosis.
Therefore, routine HPV testing is not recommended by any international/national guidelines.
The incubation period varies from three months to several years.
It is possible to become infected with several types of viruses at the same time.
After entering the body, the virus infects the tissue covering the surface of the body and organs - the epithelium, namely its inner part (basal layer).
The virus inside the cell may not affect chromosomes or integrate into the genome.
The last option, the so-called. the malignant form is manifested by the appearance of cells with altered DNA, which multiply and form a tumor.
Thus, if a woman is a carrier of HPV type 16, 18, 6, 11 or others, the following conditions are possible:
- latent course of infection, when the virus does not affect cellular DNA, women have no clinical manifestations, and infection is detected only by PCR
- the appearance of such clinical manifestations as condylomas, warts, papillomas, the virus does not change the cellular genome, but provokes increased cell proliferation (the problem is detected by the presence of symptoms, PAP test, PCR method)
- the development of neoplastic changes (dysplasia), when the virus made a change in the DNA of the cell and caused corresponding changes in the latter (such changes are called koilocytosis), the situation is confirmed by PCR, PAP test, histological and colposcopic examination
- carcinoma, when the pathogen has changed the cellular genome and caused the formation of a large number of altered (“atypical”) cells – invasive cancer (the diagnosis is confirmed by PCR, Pap test, histological and colposcopic studies)
In most situations (up to 90%), the body heals from the virus within about 2 years.
The development of symptoms is observed only in 1-5% of infected people.
With regard to HPV 16, causes of severe clinical symptoms in women include:
- early onset of sexual activity
- having multiple sex partners
- multiple pregnancies/births before age 20
- smoking
- chronic cervicitis
- decreased immune defense, for example, due to concomitant HIV infection (with a normal functioning immune system, cancer in an infected woman can develop in 15-20 years, while in an HIV-infected woman - in 5-10 years, while HIV also increases the likelihood HPV infection)
Where is papillomavirus treated in St. Petersburg, prices
You can contact the Diana private clinic in St. Petersburg for diagnosis and treatment of papillomavirus. We use modern methods approved in the best European clinics, and the prices for specialist services are quite affordable.
Here you can get tested for the human papillomavirus and remove any tumors. Removal of formations associated with HPV is carried out using the latest Fotek radioknife with a coagulator that prevents bleeding. Price for removal of condylomas, papillomas, etc. — from 500 rub. We also offer the HPV vaccine with Gardasil.
What does advanced screening show?
For a more complete examination and diagnosis, as well as in case of suspicion of several types of HPV at once, it is appropriate to ask for extended HPV screening. This one contains information about 15 types of viruses. Essentially, this is a quantitative method that makes it possible to detect DNA. The main feature that distinguishes HPV HCR screening is its 100% specificity of determination.
Having received the results of the polymerase chain reaction PCR, the doctor has the opportunity to more successfully select a treatment regimen.
Extended testing, cervical screening is deciphered using a special parameter - control of material collection.