Good afternoon, dear parents and teenagers! Acne appears on the back of a teenager - today we will tell you what to do and how to cure it. Internal changes associated with growing up, which actively occur in the human body during puberty, entail external consequences that cannot be ignored, and sometimes they cause a lot of inconvenience to a teenager.
Adolescence is almost always accompanied by severe acne. The areas most affected by acne are the back, face and chest.
While a rash on the face is easier to deal with, acne on a teenager’s back may not be so easy to treat.
But it is still possible to cope with them. So, let's look at what to do if a teenager has pimples on his back.
Causes of acne on the back during adolescence
Adolescence is a special time when the child’s body, under the influence of various numerous hormones, is completely rebuilt and matures.
It is because of hormonal imbalance in adolescence that the first “fuzz” on the lip begins to appear, the voice “breaks”, and of course, most teenagers develop pimples on the back and more.
The first and main reason for the appearance of acne on the back in adolescents is the increased work of the exocrine glands, which is provoked by the intensive production of hormones.
The mechanism for the appearance of acne on the skin is as follows: the sebaceous gland secretes too much secretion, and the hole (pore) becomes clogged with scales of dead epidermis, the same sebum and dust, as a result, sebum accumulates inside the pore and bacteria actively multiply in it, which leads to inflammation .
Along with the increased work of the exocrine glands, there are things that contribute to the formation of acne on the back of a teenager. Here's what can make your acne worse.
- Poor nutrition.
- Lack of hygiene.
- Synthetic clothing.
- Unsuitable care products.
- Too much sugar in the diet.
Therefore, in order to get rid of acne on the back, you will need not only local treatment, that is, the use of ointments or creams, but you also need some changes in diet, clothing, and possibly in the choice of hygiene products. Let's look at how to get rid of teenage acne on your back.
ACNE IN TEENAGERS
Juvenile acne (blackheads) is the most common skin disease in children and adolescents. The onset of the disease usually occurs in girls aged 12-14 years, in boys at 14-15 years old - due to late puberty. Currently, the myth that the development of acne depends on the nature of nutrition, age hygiene, and sex life has been debunked. Acne is a disease of the sebaceous glands and hair follicles, the functioning of which is associated with the exchange of sex hormones. It is generally accepted that the skin is the main link in the metabolism of sex steroid hormones, and the main “targets” for them are the epidermis, hair follicles and sebaceous glands. Changes in the functional activity of the endocrine system in adolescents at different periods of puberty have their own characteristics. At each stage of development, the sequential inclusion and functioning of endocrine glands, hormones and biologically active substances occurs. They are in close interaction with the synthesis of testosterone (Te) and sex steroid binding globulin (SSBG) secreted by hepatocytes. In addition, the mechanisms of central regulation of the hypothalamic-pituitary system change, which affects the secretion of sex steroid hormones. During puberty, with acne, the ratio between androgens and estrogens is disrupted, and there are twice as many androgens as in healthy individuals. Thus, in the development of acne, the leading role is given to Te and its metabolite - dihydrotestosterone (DTT), the biosynthesis of which is 20-30 times higher compared to healthy people, and in boys this process is more intense than in girls. At the same time, the biosynthesis of some skin enzymes also increases: the activity of 3-hydroxydehydrogenase and 5-reductase is also significantly increased compared to the norm. The latter converts free Te into DHT, which is the main hormone involved in the hypersecretion of the sebaceous gland.
Hypersecretion of sebum is a consequence of high levels of androgens and increased sensitivity of the sebaceous glands to them.
Of decisive importance in this regard are: the direct effect of the increased content of androgens in the blood on the hair follicles and sebaceous glands; increasing the sensitivity of target cells, sex steroid receptors, to circulating androgens; a combination of these two factors.
The secretion of sebum and the size of the sebaceous glands are stimulated by free testosterone of testicular or ovarian origin, dehydroepiandrosterone and androstenedione of adrenal origin. Progesterone, a precursor to testosterone, estrogens and adrenocorticosteroids, has the same effect. Progesterone enhances the secretion of the sebaceous glands due to androgenic and antiestrogenic activity. This fact explains the increase in sebum secretion and the appearance of acne elements before menstruation in women.
An increase in the level of androgens in the blood can be of a temporary physiological nature, for example, during the premenstrual period in women.
Sometimes high levels of free testosterone are caused by decreased levels of sex hormone binding globulin (SHBG). This protein, to which 65% of Te circulating in the blood binds, is synthesized in the liver. The rest combines with albumin, and only 2% of circulating total testosterone remains in the active, unbound form. Therefore, markers of latent hyperandrogenism in males are an increase in the free fraction of Te, and not total testosterone, and a decrease in PSSG (N. E. Kushlinsky, V. A. Samsonov, S. A. Masyukova, I. V. Salamova, 1996).
In women, an important pathogenetic link in hyperandrogenism is the disruption of androgen binding by specific sex steroid binding globulin (SSB), and its concentration is two times higher than in men. This sex difference is explained by the fact that estrogens stimulate, and androgens inhibit, the production of dry eye hormones.
Genetic factors are the trigger point in the development of acne, and, according to K. N. Suvorova (2000), different expressivity and allelic variations of genes that determine the development of the sebaceous glands and their functional ability, and the level of enzymes and hormones to a large extent determine the severity of clinical manifestations . In addition, there is a message about the presence of a nuclear R-factor that determines genetic predisposition. These facts can probably explain the fact that some patients develop quickly passing physiological acne, while others develop more severe forms. According to numerous studies, the likelihood of developing acne in adolescents, if there is a disease in the family or among relatives, ranges from 50-70%.
In addition to androgenic stimulation, hypersecretion of sebum by the sebaceous glands, in most patients the onset of acne is accompanied by hyperkeratinization of the base of the follicle, which leads to blockage of the follicular duct by horny scales and the formation of a microcomedone or a clinically visible closed one (white head); or open (black head). Subsequently, damage and rupture of the duct occurs, with the subsequent development of perifocal inflammation. Retention hyperkeratosis of the acrocrone of the follicle and hyperplasia of the follicular epithelium are decisive in the development of the disease.
Blockage of the sebaceous gland duct entails the cessation of air access, and the resulting oxygen-free conditions are optimal for the proliferation of P. acnes, which is why closed comedones are called a “time bomb.” P. acnes is normally found in sebaceous glands and follicles. The skin also contains staphylococci (epidermal and aureus), micrococci, fungi of the genus Candida and Pytirosporum ovale. Moreover, the number of colonies of microorganisms is proportional to the severity of acne elements: comedones - open and closed, papules, pustules. The outcome of inflammation, as well as the predominance of one of the pathogenetic factors, largely determines the variety of clinical forms of the disease.
An important aspect is the participation of P. acnes in the development of inflammation: they synthesize various chemoattractants that attract leukocytes to the site of inflammation, lipases and a number of enzymes that lead to damage to the follicle wall. They are capable of inducing the production of anti-inflammatory cytokines by mononuclear cells: IL-8, IL-1, TNF, etc., and synthesize antigens that stimulate the production of antibodies, the number of which is increased in patients with acne compared to healthy people. P. acnes produces vasoactive amines like histamine, which increase inflammation. If comedones and papular-pustular rashes are characterized by a high contamination of P. acnes, then with nodular-cystic rashes the amount of P. acnes is minimal. The formation of conglobate acne is probably associated not so much with the number of microorganisms as with a delayed-type hyperreaction (DTH) in the dermis, which may explain the high therapeutic effect of isotretinoin.
The uniqueness of propions largely determines the characteristics of the resolution of inflammatory acne elements. Unlike most strepto- and staphyloderma, inflammatory acne elements resolve more slowly, despite intensive treatment. Torpidity to therapy is due to the resistance of P. acnes to destruction by neutrophils and monocytes, persistence in phagocytic cells, where microorganisms remain viable for a long time, despite antibiotic therapy. In addition, overproduction of sebum does not make it possible to create the necessary concentration of the antibiotic in the ducts of the sebaceous gland. This may explain the prescription of long courses of antibiotics in the treatment of acne.
Thus, genetic predisposition, androgenic stimulation, increased sebum secretion and follicular hyperkeratosis lead to blockage of the sebaceous gland duct with comedones. As a result of the proliferation of P. acnes and the formation of inflammation around the follicle and sebaceous gland, non-inflammatory and inflammatory acne elements (papule, pustule, nodule) are formed. Depending on the nature of the inflammation and the spread of the pathological process in the dermis, the lesions can thicken, infiltrate or abscess with the formation of cysts, which determines the variety of clinical manifestations of the disease. During therapy or spontaneously when acne elements resolve, spots, depigmented scars, hypertrophic or disfiguring keloid scars remain.
Often in adolescents, the onset of the disease is accompanied by the appearance of non-inflammatory and inflammatory acne elements, which are regarded as “physiological” acne. They accompany the pubertal hormonal crisis and, due to their insignificant manifestation (comedones, single papular-pustular acne elements), can spontaneously and completely disappear without treatment. “Clinical” acne occurs in 15% of patients and requires treatment lasting from several months to a year or more or until spontaneous remission is achieved, usually occurring by age 25.
According to the modern classification, the following clinical varieties of juvenile acne are distinguished (G. Plevig, A. Kligman, 1993, 2000).
- Comedonal acne.
- Papular-pustular acne.
- Conglobate acne.
- Inverse acne.
- Lightning acne.
- Mechanical acne.
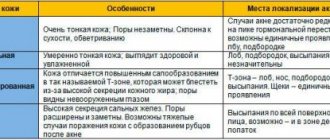
The development and course of dermatosis depend on the following factors: family (genetic) predisposition, clinical form of the disease, skin type and color. When conducting clinical diagnostics, it is necessary to take into account the following features of acne:
- type of rash (inflammatory or non-inflammatory);
- the number of rashes and their prevalence, size and location;
- severity of complications (pigmentation, excoriation, scars);
- assessment of psychosocial status (anxiety, depression, social maladjustment, etc.);
- if necessary, bacterial culture with determination of sensitivity to antibiotics, studies of hormonal status, skin biopsy for differential diagnosis with other dermatoses;
- patients with severe and often recurrent forms of acne should be examined for the presence of concomitant pathology;
- measurement of the level and rate of sebum excretion (SES);
- creating a trusting relationship between doctor and patient.
In the pathogenesis of acne, primary and secondary factors leading to the development of the disease are distinguished.
Basic principles of treatment: it is necessary to reduce the secretion of the sebaceous gland, reduce inflammation, reduce the colonization of the skin by Propionbacterium acnes and other microorganisms, normalize the mitotic activity of keratinocytes and eliminate blockage of the sebaceous gland duct.
Treatment in many cases is a difficult task, and the use of various therapeutic methods and cosmetics leads only to clinical remission, less often to cure. The choice of therapy is determined not only by the severity of acne, but also by the general condition and psycho-emotional characteristics of the individual.
Currently, recommendations and an algorithm for the pathogenetic treatment of various forms of acne have been developed (XX World Congress of Dermatology, Paris, 2002).
The main objectives in treatment are:
- preventing the formation of comedones (preventive measures and tips for caring for “problem” skin);
- removal of comedones (acne toilet, comedo extraction, tretinoin, retinoic acid, adapalene, salicylic acid, resorcinol);
- reduction in sebum production (retinoids systemically and externally, hormonal drugs - antiandrogens, estrogens, etc.);
- prevention of the opening of comedones, pustules and the development of inflammation (systemic antibiotics and antibacterial drugs for external use);
- combination therapy (systemic antibiotics and topical retinoids or sequential use of glucocorticoids, systemic retinoids, for severe forms of acne);
- preventing the appearance of scars (early initiation of treatment, retinoids, eliminating the possibility of mechanical injury to acne elements);
- improving the appearance of scars only after achieving stable clinical remission (peeling, resurfacing, introduction of implants, corticosteroids; laser therapy, etc.).
The choice of treatment method depends on the following factors: the clinical form of the disease, the nature of acne elements (non-inflammatory, inflammatory), severity (mild, moderate, severe), depth, localization and extent of the process (see Table 1).
For example, comedonal acne is best treated with topical retinoids, while for mild inflammatory acne, retinoids, topical antibiotics, VPO, etc. are indicated. In addition to the severity of acne lesions, complications of dermatosis in the form of scar formation, pigmentation, and also psychosocial problems.
In practice, systemic and topical retinoids are the first choice drugs and were first used for the treatment of acne about 30 years ago by Stuttgen and Baer. First, second and third generation retinoids have general and local effects and are capable of causing a specific biological response as a result of binding and activation of retinoic acid receptors - RAR (retinoid acid receptor).
The mechanism of action of retinoids is to inhibit the processes of keratinization (keratinization), reduce sebum secretion, and also the activity of R. acnes and increased proliferation of epithelial cells of the skin and sebaceous glands, thus affecting all parts of the pathogenesis of the disease.
Indications for external therapy are: mild non-inflammatory and inflammatory forms of acne, as well as non-inflammatory forms of moderate severity.
It is possible to use it in combination with systemic medications for moderate and severe forms of inflammatory acne.
The group of synthetic retinoids of the new (third) generation includes adapalene (Differin), a derivative of naphthoic acid, which has not only the properties of retinoids, but also an anti-inflammatory effect.
The anticomedogenic-comedolytic effect of differin is based on selective interaction with nuclear γ-receptors of epithelial cells (RAR-γ), as a result of which the processes of differentiation of keratinocytes in the infundibulum of the sebaceous gland are improved and the production of sebum is normalized (duct blockage is prevented), as well as the proliferation of skin corneocytes. Thus, differin prevents the formation of microcomedones and promotes the removal of the “keratin plug” (comedogenic and comedolytic effect).
The anti-inflammatory effect of differin has also been studied in vitro and in vivo. It has been established that the drug inhibits the release of cytokines (markers of inflammation) - IL-1, IL-8, IL-12 - through competitive binding to TLR2 receptors of monocytes. In addition, inhibition of lipoxygenase and arachidonic acid, which is involved in the regulation of lipid metabolism in the skin, is observed. The unique pharmacological properties of differin explain its advantages (anti-inflammatory effect, better tolerability) over trans-retinoic and retinoic acid.
One of the disadvantages of external retinoids is their weak effect on hypersecretion of the sebaceous glands, which requires, in some cases, the administration of systemic retinoids (isotretinoin) in adequate doses for severe forms of acne. The drugs are prescribed for a long time (up to three months or more), as well as for prophylactic purposes to prevent the appearance of new acne elements.
For the treatment of conglobate acne, the basic drug is isotretinoin-roaccutane at 0.5-1.0 mg/kg of body weight per day until a total cumulative dose of 120 mg/kg is reached. In addition, treatment with antibiotics gives temporary results, and frequent relapses are observed after their discontinuation. In adolescence, the use of antibiotics should be limited to short courses of no more than four to six weeks, so the emphasis is on the use of topical drugs with multidirectional effects, especially for mild to moderate juvenile acne.
For mechanical acne (pathomymia), psychological rehabilitation, the establishment of trusting relationships with adolescents and the prescription of sedatives in combination with topical pathogenetic drugs are necessary.
For severe fulminant and inverse acne, treatment begins with the prescription of glucocorticoids (prednisolone) in a daily dose of 20-30 mg with a gradual dose reduction by 0.05 mg every five days until the drug is completely discontinued. Prednisolone is prescribed in combination with antibiotics (according to antibiotic sensitivity), and then switched to isotretinoin in adequate doses: 0.5-1.0 mg/kg body weight per day until a total cumulative dose of 120 mg/kg is reached.
Systemic therapy (oral antibiotics, isotretinoin), often in combination with topical medications, is indicated for the treatment of patients with moderate to severe acne. Basic antibiotics are tetracyclines: tetracycline - daily dose of 500 mg twice a day, tetracycline monohydrate - 0.1 mg twice a day, minocycline - 0.1 mg twice a day; macrolides: erythromycin 500 mg twice a day, josamycin: 500 mg twice a day. Alternative drugs for antibiotic intolerance are cotrimoxazole 480 mg twice or timethoprim 100-200 mg from 14 to 21 days. If one antibiotic is ineffective, in some cases it can be replaced with another. However, long-term antibiotic therapy may cause P. acnes resistance, rendering treatment ineffective.
When treating with isotretinoin, it should be remembered that young men with damage to the trunk respond worse to treatment with small doses, so they should be prescribed a starting dose of 1.0 mg/kg, and in older people and sensitive (white) skin - 0.5 mg/kg day, with mandatory monthly biochemical monitoring.
On the pharmaceutical market for topical (external) therapy, various commercial companies offer modern drugs with comedogenic, keratolytic, antibacterial, anti-inflammatory and antiandrogenic properties. One of their disadvantages is their weak effect on hypersecretion of the sebaceous glands, which in some cases requires the use of systemic retinoids (isotretinoin) in adequate doses. The drugs are prescribed for a long time (up to three months or more), as well as for prophylactic purposes - to prevent the appearance of new acne elements.
The basic drugs for external treatment of acne, as well as for systemic treatment, are retinoids, as well as antibacterial drugs - benzoyl peroxide (Baziron AC), local forms of antibiotics (clindamycin, erythromycin, tetracycline, mupirocin, fusidic acid) and systemic antibiotics; alternatives are azelaic acid, hyaluronic acid.
Azelaic acid - a natural dicarboxylic acid (skinorene) has an antimicrobial and anti-inflammatory effect, normalizes keratinization processes, blocks 5-α-reductase and the conversion of testosterone to 5-dihydrotestosterone.
In cosmetology, β-hydroxy acids (salicylic acid) are used, as well as resorcinol in small concentrations (1-3%), α-hydroxy acids (AHA) - malic, tartaric, citrus, lactic and glycolic acids. It should be remembered that topical antibiotics are not recommended to be combined with systemic antibiotics.
The antibacterial drug baziron AS, containing benzoyl peroxide, does not develop resistance in microorganisms, so it can be used for long courses of treatment, as well as as maintenance therapy. In addition, the risk of developing microbial resistance to antibiotics is reduced when they are combined with benzoyl peroxide [8]. Water-based gel for external use, Baziron AS, in addition to antibacterial and anti-inflammatory, also has comedolytic and moisturizing effects. The combined preparation Baziron AS contains an “acrylic copolymer - glycerin” system, which ensures controlled absorption of sebum and skin hydration: the gel is indicated for all skin types, including sensitive ones.
An important place in the rehabilitation of patients with acne and the prevention of the development of complications is given to compliance with recommendations for facial skin care (acne-toilet) using maintenance therapy with topical retinoids, cleansing lotions, gels that do not have a comedogenic effect. Each of these drugs for topical and systemic action has its own advantages and side effects, so it is very important to follow the recommendations given by your doctor.
S. A. Masyukova , Doctor of Medical Sciences, Professor Z. S. Bekmagomaeva, S. A. Razumova, N. V. Gunina SIUV MO RF, Moscow
Acne on the back of a teenager - how to get rid of it
Visit to a dermatologist
For some reason, many parents have formed the strong opinion that teenage pimples are as natural as breathing.
Many people believe that if a teenager has acne on his back, he should simply “outgrow” it, and that everything will go away over time.
There is no doubt - of course it will pass, but only if you let everything take its course, there can be dire consequences, including the need for surgical intervention.
Therefore, you should not ignore teenage acne, and at the same time there is no need to panic - no one has ever died from acne on the back.
Just take your actively growing child by the hand and go for an examination to a dermatologist, who will prescribe you the appropriate treatment based on the severity of the rash.
As a rule, in the case of acne on the back in adolescents, topical antibacterial drugs are prescribed, as well as ointments based on zinc oxide.
In some cases, when there is too much inflamed acne, severe pimples break out on the back of a teenager and have a “core” inside, an intramuscular antibiotic is prescribed, as well as local ichthyol ointment, or balsamic liniment according to Vishnevsky.
In some cases, when there are medical indications, a course of autohemotherapy may be prescribed - intramuscular venous blood transfusion.
Normalizing nutrition will help
To treat acne in a teenager, you will need to follow a diet for at least some time. No strict restrictions, but only normalization of nutrition.
That is, if your offspring ate French fries, chips, and deep-fried foods, then this has to end.
It is necessary to exclude from the diet all deep-fried or high-fat foods. Fried and at the same time fatty foods help to strengthen the work of the already active sebaceous glands.
In addition, it is necessary to exclude spicy foods - they irritate the sweat glands. What enhances their work? Another important dietary prohibition is sweet foods.
It is better to eliminate sugar altogether for a while, and instead offer the teenager fructose or honey.
Cosmetic professional procedures
Caring for teenage skin should be comprehensive. In addition to home procedures, you can also use the services of beauty salons if possible.
Today, more than a dozen different professional procedures are provided for the effective treatment of teenage rash.
There are cheaper options, but there are also those that not everyone can afford.
For example, chemical peeling for problem areas of the skin is an effective and inexpensive procedure that works both for the prevention and treatment of acne, and costs tens of times less than a session of equally effective mesotherapy.
Here are some salon treatments that are most popular and effective in combating teenage pimples and acne.
- Cryotherapy.
This is a relatively “young” method in cosmetology, which allows you to almost completely get rid of acne in just 5-7 sessions. This method is based on the use of liquid nitrogen, the temperature of which is about -250 degrees.
Performing this procedure at home is impossible, as appropriate equipment is required.
- Peels – chemical and mechanical.
Either one or the second version of peelings can be performed both at home and in a beauty salon.
The principle of both peeling options is based on the removal of keratinized scales of the epidermis, which clogs the pores, which provokes the appearance of sebaceous plugs, which, when inflamed, form acne on the back of a teenager.
Chemical peeling allows you to cleanse the skin of dead epidermal cells using various acids, while mechanical peeling cleanses it using abrasive particles.
- Ozone therapy.
Recommended to enhance the effect of treatment with antibacterial ointments, as an adjuvant. Ozone therapy is a procedure that is used in the treatment of various diseases, and not only skin diseases, therefore only a doctor can prescribe any specific type of ozone therapy.
Types of teenage acne
Acne
Acne belongs to the category of serious inflammatory diseases of the skin (sebaceous glands and hair follicles), which require complex and lengthy treatment. The results of such treatment directly depend on the accuracy of compliance with all doctor’s recommendations.
The first manifestations of acne can make themselves felt during the period of active puberty in boys and the first menstruation in girls:
- comedonal form - characterized by the appearance of “closed” pimples on the forehead, chin, and sometimes on the wings of the nose;
- papulopustular – a more severe form of acne, which is characterized by the appearance of purulent blisters and severe inflammation on the face. If timely measures for treatment are not taken, the result is the appearance of deep, healed scars (like chickenpox).
Inflammation of skin areas and the formation of deep purulent formations cause the proliferation of dangerous bacteria. The vital activity of this bacterium is supported by sebum, which is produced in excess during the period of hormonal changes in adolescents.
Are there drugs that can effectively fight acne? Of course, today there is a treatment that gives excellent results. However, such appointments can only be made by specialists after conducting research and analyses.
Photo source: shutterstock.com
Acne
Acne, according to experts, is a less serious skin disease. The cause of acne (black spots on the skin of the body with inflamed areas) is the excessive production of sebum, which, when mixed with skin particles, forms a kind of shell. This shell clogs the pores, where a new portion of sebum accumulates, after which a sebaceous plug is formed. Under the influence of ambient oxygen, the sebaceous plug darkens and turns into a black dot. And the bacteria present on the skin causes inflammation of such a plug and the appearance of acne. Most often, acne is located on the back, face, and chest.
How to treat the rashes themselves and how to deal with their consequences?
Acne on the back of a teenager: how to get rid of it using folk remedies
First of all, acne soap works great against acne on the back, shoulders, face, and chest. It contains healing microelements from the Dead Sea, and is not expensive.
“Grandma’s” remedies for teenage acne.
Our grandparents did not run to dermatologists if such a nuisance as acne appeared on their skin. They used the power of nature and centuries of experience to overcome this problem, and were very successful in coping with all this even without visiting salons.
Therefore, today we can use the gifts of nature in tandem with the experience of our ancestors. Here are some folk remedies that have proven themselves to be effective and safe for several centuries.
Honey
Since ancient times, people have known about the antibacterial properties of honey and actively used this natural remedy to treat various inflammatory processes. And today honey is used as a powerful antibiotic; moreover, its effectiveness in the fight against microbes and fungi has been proven in scientific research.
Honey can be used to lubricate teenage acne on the back, or as a base for a homemade scrub. If you use honey internally, along with pollen, you can strengthen your immune system, which is also useful in the treatment of acne.
Plantain
Plantain is also known as an antibacterial and regenerative agent. Using a paste of fresh plantain leaves and stems, you can speed up the healing of pimples and also avoid the appearance of unsightly scars.
It is also recommended to use a decoction of dry plantain leaves to wipe acne.
Chamomile
The classic method of treating almost all skin diseases is the use of baths based on chamomile decoction. Chamomile is a powerful antibacterial agent that also has a drying effect.
With the help of warm baths based on a decoction of chamomile flowers, you can normalize the functioning of the sebaceous glands.
Yeast compress
A yeast compress helps normalize sweating and activate the body's defenses. Previously, bread sourdough was used for compresses against acne; today such a wonder is very difficult to obtain, so you can use ordinary live yeast.
Yeast (50 grams) must be diluted in warm water (also 50 grams), apply the resulting mixture to natural fabric. The compress should be tied to the problem area of the skin and left for 2 hours, and then rinsed off.
To get an effective result to quickly cure acne on a teenager’s back, it is advisable to use the above methods in a comprehensive manner.
In addition, it is important not to forget about the need to frequently cleanse the skin using antibacterial agents and wear clothes made of natural fabric.
If acne on a teenager’s back, despite various treatment and preventive measures, gets worse and is accompanied by other symptoms, such as fever, then be sure to consult a doctor as soon as possible - perhaps it’s not acne at all.
Acne on the back of a teenager, what to do?
Acne vulgaris in adolescents
What are acne vulgaris?
Acne vulgaris (acne) is a disease that can affect approximately 80% of young people from 14 to 30 years old. It manifests itself as inflamed nodules that can “pop up” on the skin of the face, chest, neck and back. The disease is very common; however, only 20% of patients consult a doctor; For the rest, acne vulgaris occurs in a mild form and is often considered a physiological condition. The peak of the disease falls at puberty - 14-16 years, in girls slightly earlier than in boys, which is explained by the earlier onset of puberty); rashes continue, as a rule, until 20-25 years.
How are they formed?
During puberty, our body begins to produce a huge amount of sex hormones. These hormones increase the activity of the sebaceous glands, which have the ability to clog pores, resulting in comedones (plugs). Due to the presence of comedones, sebum simply does not have the opportunity to be released onto the surface of the skin; sebum production continues at the same time. As a result of these processes, bacteria that are very viable begin to develop in the clogged follicle. They provoke the process of inflammation, and it happens that the follicle ruptures. Leukocytes begin to fight inflammation, which simultaneously destroy bacteria and die themselves. The result is the appearance of pus.
The main reasons for the development of rashes.
- Poor nutrition (spicy, salty, a lot of sweets, alcohol), dry eating increases the activity of the sebaceous glands.
- Stress can increase the severity of the condition and cause new acne. In turn, acne itself causes stress, and squeezing it out worsens a person’s appearance. Surveys of a large number of patients suffering from acne have shown that many of them experience feelings of shame, embarrassment and anxiety, and lack of self-confidence. Severe acne can cause anger and anxiety.
- Premenstrual exacerbations. About 70% of girls note an exacerbation of inflammatory phenomena 2-7 days before menstruation. It is possible that this is due to changes in the hydration of the follicular epithelium in the premenstrual period.
- Hormonal changes, diseases associated with the endocrine system, as well as changes associated with age can cause acne.
- Sweating. 15% of patients noted the negative impact of humidity on the course of the disease, especially in cases where a person lives in a humid, warm environment;
- Ultraviolet irradiation. Many patients and doctors are convinced that sunlight has a positive effect on acne. There is no scientific evidence for this. It is possible that the improvement is due to the psychological effects of tanning.
- Hereditary predisposition is of undoubted importance in the occurrence of acne vulgaris, the severity of its course, localization, prevalence and sensitivity to therapy. According to dermatologists, in 45% of schoolchildren with acne vulgaris, one or both parents also noted acne, while at the same time, acne vulgaris was observed only in 8% of schoolchildren whose parents did not have acne. A hereditary predisposition to the appearance of acne vulgaris has also been confirmed by genetic studies on twins.
- Smoking has a negative effect on the progression of acne.
What types of acne are there?
Acne comes in different forms and manifests itself in different ways:
- In the form of black dots - hard horny scales that impede the access of sebum. The outer part of the cork fills with dust and becomes brown or dark. Acne usually appears on the nose, forehead and chin, as well as on the back and chest.
- Whiteheads (millet acne) are pinpoint nodules comparable in size to grains, occurring due to stretching of the gland and sebum retention. They are usually located on the cheekbones and eyelid area. Such acne occurs one at a time or in groups.
- Acne vulgaris (ordinary) appears as a result of constant inflammation of the sebaceous glands. They usually form in adolescents during puberty. The condition of the skin worsens due to poor hygiene and abuse of unhealthy foods.
- Pustular acne with a purulent cap is usually red in color and appears as a result of damage to the epidermis and the release of harmful organisms to the outside. The main reason for the formation of pustules is squeezing out acne.
- Phlegmonous acne is a tumor. They are formed as a result of damage to a large number of sebaceous glands. Phlegmonous acne grows together and turns into abscesses or ulcers. At the site of their opening, scars form.
- Conglobate acne is round in shape and is connected by a staphylococcal bacillus. This is the most dangerous acne, affecting the side of the cheeks, back, and neck. This disease stimulates the formation of nodes, which consist of individual bulges. After healing, a scar remains in their place.
What are some tips for preventing acne vulgaris?
- Advice one. You can't sunbathe. We often hear that in the sun, acne on the chin and body disappears on its own. Sometimes this really happens, but everything is not as simple as it seems. Sun exposure causes increased sebum production, which is undesirable.
- Tip two. You can't wash your face often. Of course, no one is calling for uncleanliness, but the appearance of acne on the face has nothing to do with sterility. But excessively frequent washing guarantees drying of the skin, which reduces its resistance to infection. You should wash your face only twice a day, but your hands, as a possible source of infection that can cause acne on the chin, should really be washed more often.
- Tip three. You can't squeeze it out. Despite all the warnings from dermatologists, the number of people who want to squeeze acne on the body is not decreasing. This is strictly forbidden, since any attempt to squeeze out acne on the face causes the infection to penetrate into the deeper layers of the skin, aggravating the inflammation. In addition, infection is transmitted to non-inflamed elements of acne, initiating new lesions.
- Tip four. Do not use alcohol products. Alcohol products are intended only for spot treatment, and with prolonged use, necrosis of the epidermis occurs.
- Tip five. The most important. You cannot let the disease take its course; acne is not just pimples on the face or body, but a serious illness. The sooner you contact a dermatologist, the faster the result will be achieved. A dermatologist will evaluate the condition of your skin and prescribe treatment depending on the stage of acne.
Doctor - dermatovenerologist Strapko E.V.