the problem of comedones on the skin of the face and body, and not only during teenage hormonal changes. Those with oily skin have to cope with this problem all their lives using any available means. In our article we will tell you what comedones are, why they appear and how to get rid of them.
What are comedones and what are they like?
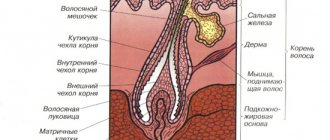
Epidermal cells are constantly renewed throughout a person's life. And during the normal course of this process, the keratinized cells are exfoliated on their own, and the sebaceous ducts perform the function of secreting sebum ( sebum ). Sebum forms a hydrolipidic protective film on the surface of the skin.
However, in some cases, dead cells are not removed on their own, but form a stratum corneum that clogs the sebaceous ducts. Sebum can also become thicker for a variety of reasons, including being full of toxins. Due to the subcutaneous plug, a capsule is formed in the sebaceous gland, which creates an ideal environment for the development of bacteria. All this leads to inflammation, which is called comedones.
Risk factors
In addition to the main reasons, there are a number of factors that increase the risk of developing comedones. The most significant include:
- Hereditary predisposition.
- Frequent stress and emotional overstrain, lack of sleep.
- Natural fluctuations in hormonal levels, including during puberty and the transition to menopause.
- Endocrine diseases: hyperthyroidism, diabetes mellitus type 1 and 2, polycystic ovary syndrome, hyperandrogenism.
- Poor nutrition: excessive consumption of flour and confectionery products, whole milk products, fatty and fried foods.
- Smoking and excessive consumption of alcoholic beverages.
- Pathologies of the gastrointestinal tract: gastritis, peptic ulcer of the stomach and duodenum, dysbacteriosis.
- Friction or pressure on the skin, such as the use of mobile phones, helmets, tight collars and backpacks.
Pregnancy and the onset of menopause
One of the important triggering factors for comedones is hormonal imbalance.
Quite often this is due to a change in the ratio between male and female sex hormones (androgens and estrogens). Natural hormonal changes in the body, for example, occur during pregnancy and at the beginning of menopause. The sebaceous glands are also part of the endocrine system and are controlled by androgen receptors. Steroid sex hormones (dihydrotestosterone) are responsible for the synthesis of sebum. As a result of sharp fluctuations in the ratio of androgens and estrogens, the synthesis of sebum is stimulated, and the division of cells in the stratum corneum of the skin increases, which often leads to the formation of comedones.
Let's look at the main types of comedones
Open comedones are the so-called blackheads. They are pores clogged with oxidized sebum and keratinized cells with melanin particles. Because of this, they have a dark shade and dense structure.
Closed comedones are small white subcutaneous nodules. They are formed when the sebaceous ducts are blocked by dead skin cells and sebum. Unlike blackheads, in closed comedones the plug is formed subcutaneously, and the duct does not have an exit to the outside. Papules quite often become inflamed, also cause pain, and a reddish tint appears around them.
Both types of comedones spoil the appearance, form irregularities, pigment spots, and depressions (as a consequence), and improper treatment and removal can cause the appearance of new lesions.
Many comedones form acne - a disease of skin rashes.
It is important not to confuse closed comedones with milia (epidermal cystic formations), sebaceous adenomas (benign skin formations characteristic of adulthood) and allergic rashes. Getting rid of these types of skin diseases is possible only in a beauty salon, under the supervision of a doctor.
Classification of comedones
In clinical practice, comedones are divided into 2 types:
- Open. They are plugs of sebum and skin cells that block the entrance to the hair follicle. Oxidizing upon contact with air, they become black, which is why they look like black dots with a diameter of 0.5-1.0 mm.
- Closed. Clogged hair follicles, which, due to the secretion accumulated in them, expand, forming small cysts. On the skin they look like nodules about 1 mm in diameter, white or reddish.
Since comedones are one of the manifestations of acne, in clinical practice the American Academy of Dermatology classification is used to assess skin lesions. It includes 4 degrees of disease severity:
- I degree. The presence of comedones and up to ten papules - small pink blisters, sometimes with a black dot in the center.
- II degree. A combination of comedones and papules, with the appearance of no more than 5 pustules - pustules.
- III degree. Combination of comedones and papulopustular rash. In this case, no more than five nodes appear on the skin.
- IV degree. Severe inflammation of the skin with the formation of painful nodes and cysts.
Also, to assess the severity of comedonal lesions, the Cook scale² can be used, which evaluates the severity of the pathological process in points:
- 0 points. The presence of several small comedones or papules, which are noticeable only upon careful examination.
- 2 points. There are 1-2 open or 20-30 closed comedones on the skin. At the same time, up to ¼ of the surface of the facial skin is covered with small papules in a total number of up to 6-12 pieces.
- 4 points. Small papules or comedones are observed on more than ½ of the facial skin. There may also be several pustules and large comedones protruding above the surface of the skin.
- 6 points. About ¾ of the face is covered with papules and/or large open comedones, which are combined with many pustules.
- 8 points. Skin rashes are located on almost the entire surface of the face, large pustules appear.
Figure 1. Open and closed comedones. Image: mikrostoker/Depositphotos
What causes comedones?
In fact, there are many reasons for the formation of comedones, and to combat them you need an integrated approach. Therefore, it is necessary to exclude all possible provoking factors , change your lifestyle, and aim for constant support of your health. It is certainly possible to improve the situation, but you need to understand that the external manifestation of a problem always has internal causes that should be studied and eliminated, and this is a slow and systemic process.
So, let's name the main reasons for the appearance of comedones:
- hormonal imbalance (age-related changes, pregnancy or disruption of the glands);
- genetic predisposition;
- poor nutrition;
- lack of hygiene;
- poor environmental conditions;
- prolonged stress;
- lack of sleep;
- incorrectly selected cosmetics (which leads to allergies or clogged pores);
- bad habits;
- poor nutrition and poor drinking habits (which leads to indigestion).
Symptoms of comedones
Early signs of comedones are roughening of the skin and visually noticeable enlargement of pores, which is often combined with increased oiliness and a tendency to peeling. In this case, the color of the skin often changes - it may acquire a grayish or greenish tint.
Next, comedones are formed directly. Externally, depending on the type, they appear as black dots or white nodules. The last few protrude above the skin level and are prone to inflammation, which leads to redness of the skin and moderate pain when touched.
Most often, comedones are located on the skin of the face, upper chest and back. The quantity depends on the individual characteristics of the body, concomitant diseases and can range from 3-7 to 100-150 pieces.
Stages of the appearance of comedones
- Sebum accumulates in the hair follicle and gets stuck in the duct due to, among other things, a dense keratinized layer of cells (hyperkeratosis).
- The release of toxins from the deep layers of the dermis becomes more difficult.
- Sebum thickens and becomes filled with toxins and bacteria.
- The duct expands under the pressure of harmful substances accumulated in it.
- Further stages of development differ depending on whether an open or closed comedon appears:
- Or a dark plug when sebum oxidizes and melatonin (pigment) appears.
- Or the papule remains under the skin, causes internal inflammation and eventually breaks out (closed comedon).
Complications of comedones
With prolonged exposure to trigger factors, as well as improper treatment, comedones can lead to various dermatological complications. The most common among them are:
- Ostiofolliculitis. Inflammation of the hair follicle or sebaceous gland. Externally it resembles a subcutaneous node. In this case, the skin over the boil becomes thinner, becomes bluish, and a white dot appears in the center - a purulent core.
- Intradermal cysts. They are a subcutaneous cavity formation and are the result of purulent melting of inflamed comedones. After healing, a rough connective tissue scar is left.
Is it possible to squeeze out comedones?
Despite the fact that one of the treatment options for this pathology is facial cleansing with mechanical removal of comedones, you cannot squeeze them out yourself. Possible complications:
- Post-inflammatory erythema. Redness of the skin, a residual phenomenon after inflammatory skin lesions. It occurs as a result of damage to local blood vessels or due to strong pressure on the skin, including when trying to squeeze out a comedone on your own.
- Pyoderma. When manually removing a comedonal rash, there is a high risk of introducing infection (pathogenic staphylococci and streptococci) into the damaged follicles. In addition to ostiofolliculitis, such actions can provoke the appearance of a boil, carbuncle, various forms of impetigo and other variants of pyoderma.
- Scarring. Rough mechanical impact on comedones, especially closed forms, often leads to deep skin damage and the formation of persistent connective tissue scars that look like pink or whitish stripes or spots.
How to get rid of closed comedones on the face
To completely get rid of comedones, it is necessary to take comprehensive measures: consult a dermatologist or cosmetologist, and also follow all instructions at home.
So, at home you need :
- make therapeutic masks containing blue clay, as well as light peelings and scrubs for home use;
- include antioxidants : fresh fruits and berries, spinach, lettuce leaves, green tea - this will help remove toxins from the body;
- use cosmetics containing keratolytics .
Keratoloitics are necessary to thin the stratum corneum of the skin, which increases the risk of comedones. Among them:
- salicylic acid 2-4% (cosmetics with a high percentage of acid are suitable for the skin of the back, neck, etc.);
- fruit acids AHA (or hydroxy acids), because they oxidize the pH of sebum, which prevents the proliferation of bacteria;
- retinol (including in peelings) - as a rule, is prescribed for external use for a long period, up to six months, with a gradual increase in the amount of the drug and the frequency of application. Suitable for the treatment of acne and multiple comedones. Oral systemic retinoids are prescribed by a doctor if necessary.
The use of keratolytics has a complex effect on the epidermis: cleansing, softening, antiseptic, brightening, stimulating the removal of the stratum corneum, opening comedones and cell renewal.
However, their use also thins the skin, making it more sensitive and unprotected, including from the sun. The cosmetologist chooses the appropriate remedy for each clinical situation and the duration of its use. He will also suggest the optimal sunscreen and tell you about other methods of skin protection.
Let's consider the options for solutions and treatment procedures that modern professional cosmetology can offer.
Diagnostics of comedones
The diagnosis is established by external examination of the affected areas of the skin by a dermatologist. If necessary, dermatoscopy is performed - examination using magnifying glasses of a dermatoscope.
Interviewing the patient also plays an important role, helping to identify existing risk factors and concomitant diseases. If the latter are present, additional consultations with related specialists (for example, an endocrinologist), laboratory or instrumental studies may be prescribed.
Differential diagnosis of comedones is carried out with other skin diseases that may have similar manifestations. These include:
- Hyperplasia of the sebaceous glands.
- Warts.
- Milia.
Treatment procedure using the M22 device
The treatment principle is based on the targeted action of light rays in the range of 311 nm. The phototherapy procedure is absolutely painless and safe, and at the same time very effective. There is no long recovery period required after it. Additional advantages are that one session only takes about 30 minutes, and the effect is targeted only to problem areas.
In addition to the treatment of comedones and acne, there is also photorejuvenation, pigmentation treatment, lifting, and also has an antiseptic effect. The necessary parameters are set on the device: wavelength and depth of exposure, radiation intensity, intervals between flashes and their duration. Before the procedure, the cosmetologist cleanses the skin, applies a conductive gel and protects the eyes of himself and the patient with special glasses.
The M22 hardware procedure is recommended not only for the treatment, but also for the prevention of acne.
Treatment of comedones
Therapy must be comprehensive. This involves treating not only skin lesions, but also eliminating the cause of their appearance, for example, prescribing hormonal therapy for endocrine pathologies. The fight against comedones directly includes the use of medications and mechanical removal of acne.
Drug therapy
An effective method of treating comedones is the use of comedolytics (retinol, retinoic acid, zinc, salicylic acid). These are medications that can prevent blockage of the hair ducts, normalizing the growth of skin cells and the secretion of sebum.
Mechanical removal of comedones
A dermatologist or cosmetologist can remove comedones mechanically. In this case, a Uno spoon or a Vidal needle is used. As a preliminary preparation, skin cleansing can be carried out - chemical peeling and microdermabrasion. Their goal is to remove particles of dust, bacteria and sebum from the surface of the skin, thereby preventing the development of complications. After the procedure, special cosmetics with anti-comedogenic properties are applied to the skin.
Other methods of cleaning the skin are also used:
- Disincrustation. It involves removing comedones using weak current discharges.
- Ultrasonic cleaning. The technique is based on the use of ultrasonic waves that gently cleanse pores. Helps improve the overall condition of the skin.
- Vacuum cleaning. The essence of the technique is to remove plugs using a vacuum.
You can’t squeeze out comedones yourself! Only a cosmetologist or dermatologist can remove comedones. Photo: kukuruzaphoto / freepik.com
Chemical peeling
As mentioned above, light peelings can be carried out at home, however, more intense and, of course, effective chemical peels can only be carried out within the walls of a cosmetology clinic under the strict supervision of a cosmetologist to avoid skin burns. Chemical peeling exfoliates dead skin cells, tightens pores, and has an antiseptic and brightening effect.
Let's look at the most popular types of chemical peels.
Milk peeling is suitable for very sensitive skin. It can be done at any time of the year. Lactic acid is found in pickles and lactic acid fermentation products. In addition to it, the composition includes urea and a complex of amino acids. This peeling gently exfoliates and at the same time moisturizes the skin, and also stimulates the growth of new cells,
Almond can be on a gel or water-alcohol basis, and can also contain not only the main component (mandelic acid), but also other types of acids. Used to improve skin quality, regulate sebum production, reduce the appearance of wrinkles and age spots.
Azelaine peeling normalizes keratinization in the follicle ducts and sebum production, has an exfoliating, antibacterial and anti-inflammatory effect. It contains nonandioic, 1.7-heptanedicarboxylic acid, which is found in wheat, barley, lilac and other plants.
Glycolic and salicylic peels (AHA and BHA) are often performed simultaneously. In tandem, they have the maximum therapeutic effect: they not only cause the death of old cells, cause their desquamation, but also stimulate the production of natural collagen, as well as skin regeneration. They also discolor pigment spots and post-acne, improve metabolic processes.
Other manifestations of comedonal acne
Large closed comedones (over 3 mm), which are localized in the cheek area and above the joints, are called microcysts or macrocomedones. They not only cause aesthetic inconvenience, but under certain conditions they can transform into more severe forms of acne.32
Small multiple closed comedones can be localized in groups. When you touch the skin with your hand, you can clearly feel the roughness. Typically, external treatment of this type of acne is supplemented with systemic medications.32
How to avoid comedones
- maintain hygiene , including regularly changing face towels and bed linen;
- avoid touching your face with your hands;
- normalize nutrition (avoid sweet, fatty, floury, fried foods and fast food), maintain a drinking regime, take vitamins;
- maintain a sleep schedule and try to avoid overwork and stress;
- do not neglect physical activity - this helps speed up metabolic processes, saturate cells with oxygen and remove toxins;
- to refuse from bad habits;
- use medications and medicinal products prescribed by a cosmetologist;
- monitor hormonal levels and avoid any changes;
- avoid prolonged exposure to the open sun;
- Do not self-medicate and do not use unproven methods of traditional medicine.
Features of nutrition and skin care
Nutritional correction for comedones involves excluding from the diet foods that increase sebum production. First of all, these are foods with a high glycemic index or fast carbohydrates. These include:
- Confectionery.
- Chocolate.
- White bread and pastries.
- Sweet carbonated drinks.
- Dairy and fermented milk products: milk, kefir, yogurt, fermented baked milk, cottage cheese, cheese.
- Trans fats: fast food and processed foods.
- Alcohol, coffee.
Why do comedones “love” those with a sweet tooth?
Consumption of large quantities of confectionery products is associated with a sharp increase in blood glucose levels, which entails a response increase in the production of insulin by the pancreas.
The hormone insulin takes part in the activation of androgen receptors in the sebaceous glands, while simultaneously increasing the level of dihydrotestosterone. As a result, sebum production increases, which is one of the provoking factors for the appearance of comedones. Whole milk and refined foods also contribute to a sharp increase in glucose and insulin levels. Figure 2. Products that provoke the appearance of comedones. Image: artcherich/freepik.com
We also note a number of products that can help to cleanse the skin faster and prevent the appearance of new comedones. This list includes:
- Products rich in zinc: chicken and beef liver, boiled beef tongue, roast beef, pumpkin and watermelon seeds, pine nuts.
- Fatty varieties of sea fish rich in omega-3 fatty acids: mackerel, tuna, sardines, salmon, cod liver.
- Vegetables and berries: carrots, sea buckthorn, parsley, celery, raspberries, blueberries, black currants.
Caring for problem skin at home should take into account the following tips and recommendations:
- Regular cleansing of the skin with special products for excessive oiliness. At the same time, cosmetics should not foam, contain alcohol or surfactants. You can also use toners containing comedolytics for additional cleansing and moisturizing.
- When using creams, you should give preference to products with a more liquid texture, without intense fatty components.
- Application of peelings and polishing agents. These procedures and medications allow you to maintain the effects of the treatment at home. In this case, you should choose products with a low concentration of active ingredients and avoid harsh scrubs.
Hollywood Secrets
Many people, including world-famous people, are prone to skin problems. They use different approaches to combat acne and comedones. For example, Megan Fox makes oxygenating and restorative face masks and cleanses her skin daily morning and evening. Cameron Diaz gave up fast food, and Rihanna gave up alcoholic drinks (these products provoke acne). Victoria Beckham eats salmon every day, Scarlett Johansson washes her makeup brushes once a week and never goes to bed with makeup on her face.
How to properly care for skin with open and closed comedones
If the skin is prone to oiliness and the formation of closed and open comedones, it requires special care. Necessary:
- wash your face and use alcohol-free tonics and lotions containing acids;
- minimize the use of foundation and other cosmetic products that clog pores;
- do self-massage and tone the skin with contrasting washes and showers;
- use sunscreen cosmetics;
- monitor cell renewal, use home peelings and special brushes for washing, do not bring the skin to a critical condition;
- moisturize and nourish the skin from the outside to avoid drying and peeling. Restoring the water balance of the epidermis is extremely important for successful treatment;
- squeeze out pimples yourself
- regularly , undergo all prescribed procedures and follow recommendations.
Cosmetology procedures for removing comedones in the salon
A corrective home routine can be supplemented with salon beauty treatments on a regular basis or courses. Procedures and salon care are selected individually by a cosmetologist based on the type, condition and needs of your skin. Aesthetic procedures do not replace the basic steps of regular home care: daily cleansing, toning, moisturizing and mattifying will help oily, problem skin stay clear and look healthy for a long time.
List of salon treatments for comedones:
- Cleaning (mechanical, ultrasonic, hardware);
- Peels of various types and depths of exposure (superficial, medium, deep);
- Phototherapy – the procedure reduces acne, smoothes post-acne (pigmentation and scars);
- Biodermabrasion or Microdermabrasion (resurfacing) - procedures fight hyperkeratosis and enlarged pores, improve microcirculation, help skin cells regenerate faster, reduce post-acne, and are suitable for treating non-inflammatory forms of rashes.
How to cleanse your face of comedones
To get rid of closed comedones, you will need to perform 2 mandatory steps:
Mechanical skin cleaning
A widely known and not always popular procedure. In the case of white comedones, it is irreplaceable .
Resorption or dissolution of closed comedones with external means is impossible. Only mechanical intervention can remove existing blockages.
The disadvantage of this method is that the effect is temporary . New elements will appear later, because... the skin functions as before.
It is carried out at least once a month until the complete disappearance of white comedones, which is only possible with concomitant external therapy.
* Read more about the most popular procedure - skin cleansing and options for its implementation here .
External use of retinoids
The drugs of choice for closed comedones are retinoids.
Retinoids are a well-studied group of substances derived from vitamin A, used in dermatology to treat problem skin with acne, and in cosmetology to correct age-related changes and hyperpigmentation.
How retinoids work:
- Retinoids naturally affect the processes of keratinization and exfoliation of skin cells - eliminate hyperkeratosis;
- They normalize the production of sebum - quantity and composition - preventing the retention of secretions inside the pores.
In accordance with the Federal Clinical Guidelines for the Management of Patients with Acne, 2015, retinoids are the first-line drugs for acne correction , including the initial stages.
Benefits of Retinoids
Why else are retinoids attractive in terms of choice for eliminating white comedones:
- Physiological – they are a substance familiar to the skin, because the body itself supplies vitamin A to the skin in low concentrations;
- Have no toxic effect;
- Penetrates well into the skin, reaching the necessary layers.
Folk remedies
Traditional medicine will help combat this problem. Herbal decoctions and various masks made from natural ingredients have a positive effect on the skin, no worse than expensive pharmaceutical products.
Effective remedies against closed comedones:
- Chamomile. Take 2 tablespoons of dried chamomile, pour a small amount of boiling water. Wait 30 minutes, strain, apply the paste on your face, keep for 15 minutes, do this every day. After a week, you will notice that the comedones have decreased in size, and over time, the grass will disappear completely.
- Protein treatment. Take one fresh chicken egg, separate the white from the yolk, beat it with 1 tablespoon of sugar, divide the mixture into 2 equal parts. Apply the first half to your face, wait until it dries completely, then do the same with the second half of the mass. Rinse off the mask with cool water, and do not forget to lubricate the skin with a nourishing cream after the procedure. Such manipulations remove impurities, cleanse pores, and promote the opening of grains;
- Vitamin mask. Grate carrots, zucchini, cucumber (in equal quantities), add 1 tbsp to the mixture. spoon of olive oil, mix thoroughly. Spread the resulting paste onto your face in a thin layer, wait 10–15 minutes, then rinse with warm water;
- Salt. Take a glass of boiled water, dilute a finely grated piece of antibacterial soap in it, add 1 tablespoon of fine salt. Soak a cotton pad in the solution, rub it into problem areas on the skin for no more than three minutes, do not overdo it, this method should be used very carefully so as not to damage the skin;
- Citrus tonic. Dilute 1 spoon of lemon or grapefruit juice with 1 glass of boiled water. Moisten a cotton pad with this product and wipe the areas where the grains accumulate. Use this remedy morning and evening.
Do not expect lightning-fast action from these recipes; for high-quality results, it should take 2-3 weeks. Don't be alarmed if it takes longer to bleed on your nose than in all other areas; this is a natural process.
What products to use for skin with closed comedones
Therapy with external agents includes the use of 2 types of agents:
Sunscreen with SPF based on mineral photo filters.
The sun's rays activate the sebaceous glands, which increases the number of blockages. The choice should be made in favor of physical photo filters - mineral screen .
Chemical photo filters are contraindicated. Their operating principle is based on converting the energy of UV rays into heat, which additionally activates the work of the sebaceous glands.
Examples:
Mineral cream SPF 30 with zinc DermaQuest based on micronized zinc oxide 18.6% is a universal sunscreen for all family members!
- Does not penetrate deep into the skin and does not cause blockages
- Safe and hypoallergenic
- Blocks up to 97% of sun rays
- In 2022, the composition is enriched with BlueLight filters against blue light
Tone cream SPF30 with zinc for the face DermaQuest - for those who do not like pale skin color. An analogue of mineral cream with SPF30, which contains pigments that give the skin a light tan.
CBD “Blue Light” face cream SPF 30 DermaQuest is a complete day cream with the functions of protecting the skin from UV rays and blue light.
- Indicated for sensitive, irritated and dry skin
- Nourishes and moisturizes
- Restores, heals and soothes irritated skin
The advantages of modern creams with SPF are not only photoprotection, but complete care products that do not require the application of additional creams in the morning.
Why doesn't the medicine help?
Many patients ask dermatologists and cosmetologists this impatient question after several weeks of treatment with the recommended drug. Doctors usually explain that there are several reasons to consider a medicine ineffective:
- the medicine was taken continuously and in the indicated dosage;
- the use complied with the instructions attached to the drug;
- if it was used only in the place where acne appeared;
- When using the medicine, all hygienic rules were observed.
If comedones on the nose or other part of the face have not disappeared a week after starting to take the drug, this is quite natural. At the first stage, the medicine prevents the occurrence of new acne. The old ones disappear on their own, but this takes time, at least a month. It is advisable to change medications only if an allergic reaction occurs.
How effective a particular medicine is can be assessed no earlier than after two months. You should not take two drugs at the same time, as it is difficult to know which of them is truly beneficial. And we can talk about the ineffectiveness of treatment only after two months, when it becomes clear that there is no improvement and new foci of acne appear. In this case, you need to contact your doctor again.
Skin cleansing
First of all, at home, you need to thoroughly cleanse your facial skin with a special cosmetic product using a sponge or sponge. Hygienic care begins with applying the cleansing composition to damp skin, then rubbing without pressure until bubbles appear and removing with a wet sponge. This helps cleanse the epidermis of particles of fat, layers of dead cells and dirt.
Every week you need to exfoliate with fruit acids or use a scrub to cleanse the skin of dead cells. Masks with bodyaga or clay also help expand pores and renew the epidermis. However, when using a peel or scrub, they can only be done once a week. If masks are the only method in the fight against closed comedones, then in a day or two.
At home, vegetable masks made from carrots, cucumbers, zucchini and apples will help cope with closed comedones. The vegetables are finely ground, using a grater or a blender, and if they do not contain acids, then lemon juice is added. The composition is supplemented with vegetable oil, most often olive oil. But in the advice of cosmetologists and reviews of many women, you can read that this oil can clog pores. In this case, you need to use a cosmetic vegetable oil suitable for your skin.
Reviews
Some reviews from women about the treatment of comedones:
- Elena, 34 years old, Lipetsk: “I had a mechanical cleaning at a beauty salon. But first I was treated because my comedones broke out due to hormonal imbalance. The endocrinologist immediately warned: first level the background, and then do something about the acne, otherwise everything will be useless. Chemical peeling somehow didn’t inspire confidence in me, so I did a brosage. The result satisfied me."
- Marina, 27 years old, Ufa: “I can’t imagine how people used to live without scrub and peeling. I always have at least three jars of different scrubs. And peeling with AHA acids is my favorite procedure. The skin glows, no pimples, comedones, rashes. Just wonderful. But, really, I agree that you need to look for “your” cosmetologist.”
- Irina, 22 years old, Moscow: “Zinerit is what helped me. For two weeks, however, I walked around with a red face, everything was so actively removed. But after a month, not even a memory of acne remained. And I had both closed and open ones. But if you have dry skin, you should use a moisturizer other than Zenerite.”
- Rita, 26 years old, Obninsk: “I suffered from acne at school. Then it passed, like most people. And about six months ago I caught the flu, got sick, and then somewhere I got a skin infection. My whole face was covered in sleep. Baziron saved me; she wiped her face twice every day. It didn’t take long for everything to finally go away, but after two months I got rid of comedones.”
Getting rid of closed comedones is not that difficult, especially if they are not caused by hormonal changes. However, the relative safety of such rashes should not be a reason to neglect this problem. Closed comedones, unlike open comedones, become inflamed much more often.
Drug treatment
Closed comedones need to be treated comprehensively. First, it is necessary to identify the cause of their appearance and cure them, and then deal with cosmetic skin defects.
Preparations for the treatment of acne and comedones are aimed at reducing the activity of the sebaceous glands, eliminating comedones and skin defects from their occurrence. Medicines can be for both internal and external use.
The most used medications for comedones:
- Zerkalin (ointment) is a product related to antibiotics. Production - Croatia. Able to treat acne and other similar formations on the skin. Effectively fights comedones.
- Roaccutane (in capsules) is a drug aimed at suppressing acne and comedones. Made in Switzerland. Contains beeswax, soybean oil. The drug should be started at small doses and gradually increased.
- Zincteral (tablets) – catalyzes metabolic processes. Manufacturer Poland.
- Series of cosmetics – Hollyland. It produces drugs in the form of ointments, lotions, and masks for the treatment of problem skin. The drugs were produced in Israel.
Any drug may have side effects or incompatibility with other drugs. Before using medications, you should consult your doctor about the advisability of their use.
Prevention and advice
You need to remember this constantly and throughout the entire course of treatment with medications, cosmetics or folk remedies, adhere to the following simple recommendations.
- Use facial cleansers (milk, toner, lotion) daily, scrubs or gommage weekly.
- Self-squeezing of comedones is strictly prohibited, which in 95% of cases leads to their inflammation, which must be treated with antibiotics.
- Choose the right line of cosmetics for skin care.
- Do not leave decorative cosmetics on your face overnight.
- Limit the amount of fatty, fried, spicy, pickled, salty, sweet, flour foods in your diet.
- Stop long-term use of medications.
- It is useless to fight comedones if you smoke a lot or abuse alcohol. It's time to say goodbye to bad habits for problem skin.
- Try to be less likely to be influenced by stressful situations.
- Treat existing stomach diseases.
- Move to an area with a better environmental situation.
All these measures are not only an effective fight against comedones, but also the prevention of this cosmetic defect. It won't be easy to change your life, but it is necessary if you want to look stunning.