the problem of comedones on the skin of the face and body, and not only during teenage hormonal changes. Those with oily skin have to cope with this problem all their lives using any available means. In our article we will tell you what comedones are, why they appear and how to get rid of them.
What are comedones and what are they like?
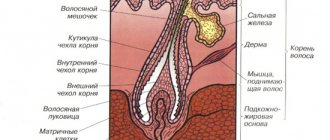
Epidermal cells are constantly renewed throughout a person's life. And during the normal course of this process, the keratinized cells are exfoliated on their own, and the sebaceous ducts perform the function of secreting sebum ( sebum ). Sebum forms a hydrolipidic protective film on the surface of the skin.
However, in some cases, dead cells are not removed on their own, but form a stratum corneum that clogs the sebaceous ducts. Sebum can also become thicker for a variety of reasons, including being full of toxins. Due to the subcutaneous plug, a capsule is formed in the sebaceous gland, which creates an ideal environment for the development of bacteria. All this leads to inflammation, which is called comedones.
Furuncle
A boil on the eyelid is one of the most dangerous lumps. The disease causes purulent necrotic inflammation of the ciliary follicle, sebaceous glands, and surrounding connective tissue. The main cause of boils is staphylococcus.
Typically, the localization of the boil is the part of the upper eyelid close to the eyebrow. Much less commonly, a lump appears on the edge of the eyelid, very close to the eye.
In its development, the disease goes through the following stages: first, a small painful nodule appears and the surrounding tissues swell (sometimes both the eyelid and the entire side of the face swell); after a few days, a yellowish abscess appears at the top of the nodule. Then the node fluctuates, the abscess opens with emptying of the contents. On the eyelid, after opening the boil, a plug (rod) remains, consisting of purulent masses and necrosis products, which after some time spontaneously comes out. As a rule, a small scar remains at the site of the boil.
A painful lump and swelling are not the only signs of a boil; the patient often feels weakness, headache and fever.
Treatment of a boil must be carried out by a doctor who will prescribe the necessary medications (antibiotics, sulfonamides, painkillers) and, if necessary, open the abscess. It is prohibited to squeeze out boils yourself.
Let's look at the main types of comedones
Open comedones are the so-called blackheads. They are pores clogged with oxidized sebum and keratinized cells with melanin particles. Because of this, they have a dark shade and dense structure.
Closed comedones are small white subcutaneous nodules. They are formed when the sebaceous ducts are blocked by dead skin cells and sebum. Unlike blackheads, in closed comedones the plug is formed subcutaneously, and the duct does not have an exit to the outside. Papules quite often become inflamed, also cause pain, and a reddish tint appears around them.
Both types of comedones spoil the appearance, form irregularities, pigment spots, and depressions (as a consequence), and improper treatment and removal can cause the appearance of new lesions.
Many comedones form acne - a disease of skin rashes.
It is important not to confuse closed comedones with milia (epidermal cystic formations), sebaceous adenomas (benign skin formations characteristic of adulthood) and allergic rashes. Getting rid of these types of skin diseases is possible only in a beauty salon, under the supervision of a doctor.
Chalazion
The lump caused by this disease is considered one of the most common problems. In another way, it is also called “hailstone” and “cold barley”. The cause of chalazion on the eyelid is blockage of the sebaceous glands. When the outlet for sebaceous secretion is blocked, the contents that are constantly being formed cannot find a way out and accumulate inside the duct. After some time, the sebaceous secretion stretches the duct and gradually hardens. If you touch such a bump, you can easily feel the dense capsule of the chalazion, which, like a ball, rolls under your fingers.
The chalazion develops slowly, painful sensations on palpation appear only when the accumulated secretion has formed a capsule. But even in the case of a practically painless course, it is better not to delay the treatment of chalazion, so that a cyst does not form. In addition to pain, chalazion may be accompanied by local redness of the conjunctiva. In its acute period, the following are possible: suppuration, granulation (excessive tissue growth), the occurrence of a fistula through which pus drains.
Naturally, chalazion rarely resolves. As a rule, such a lump needs to be treated, which is what an ophthalmologist does. In this case, treatment can be conservative or surgical. Usually, at an early stage, the doctor may prescribe UHF therapy, certain eye drops and mercury ointment. Painful chalazions at a later stage are treated with corticosteroid injections (directly inside the capsule), ointments and drops (sodium sulfacyl, ofloxacin, hydrocortisone, dexamethasone, levofloxacin and tetracycline ointment). If drug treatment does not produce the desired effect, the question of surgery is raised. Chalazion removal is performed on an outpatient basis under local anesthesia. The entire procedure lasts 10–15 minutes, after which the patient goes home.
What causes comedones?
In fact, there are many reasons for the formation of comedones, and to combat them you need an integrated approach. Therefore, it is necessary to exclude all possible provoking factors , change your lifestyle, and aim for constant support of your health. It is certainly possible to improve the situation, but you need to understand that the external manifestation of a problem always has internal causes that should be studied and eliminated, and this is a slow and systemic process.
So, let's name the main reasons for the appearance of comedones:
- hormonal imbalance (age-related changes, pregnancy or disruption of the glands);
- genetic predisposition;
- poor nutrition;
- lack of hygiene;
- poor environmental conditions;
- prolonged stress;
- lack of sleep;
- incorrectly selected cosmetics (which leads to allergies or clogged pores);
- bad habits;
- poor nutrition and poor drinking habits (which leads to indigestion).
Xanthelasma
This type of eyelid bump looks more like a flat plaque. A connection between the development of such formations and chronic metabolic disorders has been revealed. Most often, xanthelasmas appear in women suffering from diabetes, hypercholesterolemia, and pathologies of the endocrine system.
These flat formations only partially rise above the skin and have a yellowish tint. They can be located not only on the eyelid, but also in the area around the eyes. In most cases, xanthelasmas appear on the skin in groups. They do not resolve on their own. Cosmetic removal is possible, but it should be understood that if the cause of their formation is not eliminated, it can lead to the appearance of new plaques. You should focus on treating the underlying disease, and only after that seek cosmetic help.
Stages of the appearance of comedones
- Sebum accumulates in the hair follicle and gets stuck in the duct due to, among other things, a dense keratinized layer of cells (hyperkeratosis).
- The release of toxins from the deep layers of the dermis becomes more difficult.
- Sebum thickens and becomes filled with toxins and bacteria.
- The duct expands under the pressure of harmful substances accumulated in it.
- Further stages of development differ depending on whether an open or closed comedon appears:
- Or a dark plug when sebum oxidizes and melatonin (pigment) appears.
- Or the papule remains under the skin, causes internal inflammation and eventually breaks out (closed comedon).
How to get rid of closed comedones on the face
To completely get rid of comedones, it is necessary to take comprehensive measures: consult a dermatologist or cosmetologist, and also follow all instructions at home.
So, at home you need :
- make therapeutic masks containing blue clay, as well as light peelings and scrubs for home use;
- include antioxidants : fresh fruits and berries, spinach, lettuce leaves, green tea - this will help remove toxins from the body;
- use cosmetics containing keratolytics .
Keratoloitics are necessary to thin the stratum corneum of the skin, which increases the risk of comedones. Among them:
- salicylic acid 2-4% (cosmetics with a high percentage of acid are suitable for the skin of the back, neck, etc.);
- fruit acids AHA (or hydroxy acids), because they oxidize the pH of sebum, which prevents the proliferation of bacteria;
- retinol (including in peelings) - as a rule, is prescribed for external use for a long period, up to six months, with a gradual increase in the amount of the drug and the frequency of application. Suitable for the treatment of acne and multiple comedones. Oral systemic retinoids are prescribed by a doctor if necessary.
The use of keratolytics has a complex effect on the epidermis: cleansing, softening, antiseptic, brightening, stimulating the removal of the stratum corneum, opening comedones and cell renewal.
However, their use also thins the skin, making it more sensitive and unprotected, including from the sun. The cosmetologist chooses the appropriate remedy for each clinical situation and the duration of its use. He will also suggest the optimal sunscreen and tell you about other methods of skin protection.
Let's consider the options for solutions and treatment procedures that modern professional cosmetology can offer.
How to cleanse your face of comedones
To get rid of closed comedones, you will need to perform 2 mandatory steps:
Mechanical skin cleaning
A widely known and not always popular procedure. In the case of white comedones, it is irreplaceable .
Resorption or dissolution of closed comedones with external means is impossible. Only mechanical intervention can remove existing blockages.
The disadvantage of this method is that the effect is temporary . New elements will appear later, because... the skin functions as before.
It is carried out at least once a month until the complete disappearance of white comedones, which is only possible with concomitant external therapy.
* Read more about the most popular procedure - skin cleansing and options for its implementation here .
External use of retinoids
The drugs of choice for closed comedones are retinoids.
Retinoids are a well-studied group of substances derived from vitamin A, used in dermatology to treat problem skin with acne, and in cosmetology to correct age-related changes and hyperpigmentation.
How retinoids work:
- Retinoids naturally affect the processes of keratinization and exfoliation of skin cells - eliminate hyperkeratosis;
- They normalize the production of sebum - quantity and composition - preventing the retention of secretions inside the pores.
In accordance with the Federal Clinical Guidelines for the Management of Patients with Acne, 2015, retinoids are the first-line drugs for acne correction , including the initial stages.
Benefits of Retinoids
Why else are retinoids attractive in terms of choice for eliminating white comedones:
- Physiological – they are a substance familiar to the skin, because the body itself supplies vitamin A to the skin in low concentrations;
- Have no toxic effect;
- Penetrates well into the skin, reaching the necessary layers.
Treatment procedure using the M22 device
The treatment principle is based on the targeted action of light rays in the range of 311 nm. The phototherapy procedure is absolutely painless and safe, and at the same time very effective. There is no long recovery period required after it. Additional advantages are that one session only takes about 30 minutes, and the effect is targeted only to problem areas.
In addition to the treatment of comedones and acne, there is also photorejuvenation, pigmentation treatment, lifting, and also has an antiseptic effect. The necessary parameters are set on the device: wavelength and depth of exposure, radiation intensity, intervals between flashes and their duration. Before the procedure, the cosmetologist cleanses the skin, applies a conductive gel and protects the eyes of himself and the patient with special glasses.
The M22 hardware procedure is recommended not only for the treatment, but also for the prevention of acne.
Chemical peeling
As mentioned above, light peelings can be carried out at home, however, more intense and, of course, effective chemical peels can only be carried out within the walls of a cosmetology clinic under the strict supervision of a cosmetologist to avoid skin burns. Chemical peeling exfoliates dead skin cells, tightens pores, and has an antiseptic and brightening effect.
Let's look at the most popular types of chemical peels.
Milk peeling is suitable for very sensitive skin. It can be done at any time of the year. Lactic acid is found in pickles and lactic acid fermentation products. In addition to it, the composition includes urea and a complex of amino acids. This peeling gently exfoliates and at the same time moisturizes the skin, and also stimulates the growth of new cells,
Almond can be on a gel or water-alcohol basis, and can also contain not only the main component (mandelic acid), but also other types of acids. Used to improve skin quality, regulate sebum production, reduce the appearance of wrinkles and age spots.
Azelaine peeling normalizes keratinization in the follicle ducts and sebum production, has an exfoliating, antibacterial and anti-inflammatory effect. It contains nonandioic, 1.7-heptanedicarboxylic acid, which is found in wheat, barley, lilac and other plants.
Glycolic and salicylic peels (AHA and BHA) are often performed simultaneously. In tandem, they have the maximum therapeutic effect: they not only cause the death of old cells, cause their desquamation, but also stimulate the production of natural collagen, as well as skin regeneration. They also discolor pigment spots and post-acne, improve metabolic processes.
Barley
Styes are more common than chalazions. This type of lump on the lower or upper eyelid is caused by inflammation of the follicle (bulb) of the eyelash. This also clogs the sebaceous gland duct. Styes develop over several days or even hours and can occur in both adults and children. More often, the systematic appearance of barley is observed in people with weakened immune systems or who have changed their place of residence to an area with a more severe climate, as well as in people exposed to constant stress factors.
Based on their origin, there are two types of barley. Inflammation can be external (when the sebaceous gland suppurates) and internal (when the source of inflammation is located in the membolic gland).
The development of external styes is characterized by subjective sensations similar to a foreign body entering the eye. The initial stage may also be accompanied by stabbing pain. External stye visually manifests itself as redness and swelling of the eyelid. The internal one is usually not so noticeable, but it causes even more discomfort and pain.
Without treatment, barley develops within a few days into an abscess, which opens with the release of purulent contents. This brings relief, but an open wound is dangerous due to the possibility of re-infection.
It is better to start treating barley without waiting for the abscess to spontaneously break through. This allows you to get rid of the painful lump faster and with less risk of complications. If you still don’t have the courage or time to visit an ophthalmologist, you should remember that prolonged suppuration of the eyelid is very dangerous. If the stye does not open for more than two weeks, surgical treatment is necessary. An ophthalmic surgeon will remove the abscess under local anesthesia and give recommendations for further treatment of the eyelid. Most often, therapy for developing or already opened barley includes drops and ointments that contain antibiotics (albucid, gentamicin, erythromycin, tetracycline ointment).
How to avoid comedones
- maintain hygiene , including regularly changing face towels and bed linen;
- avoid touching your face with your hands;
- normalize nutrition (avoid sweet, fatty, floury, fried foods and fast food), maintain a drinking regime, take vitamins;
- maintain a sleep schedule and try to avoid overwork and stress;
- do not neglect physical activity - this helps speed up metabolic processes, saturate cells with oxygen and remove toxins;
- to refuse from bad habits;
- use medications and medicinal products prescribed by a cosmetologist;
- monitor hormonal levels and avoid any changes;
- avoid prolonged exposure to the open sun;
- Do not self-medicate and do not use unproven methods of traditional medicine.
How to properly care for skin with open and closed comedones
If the skin is prone to oiliness and the formation of closed and open comedones, it requires special care. Necessary:
- wash your face and use alcohol-free tonics and lotions containing acids;
- minimize the use of foundation and other cosmetic products that clog pores;
- do self-massage and tone the skin with contrasting washes and showers;
- use sunscreen cosmetics;
- monitor cell renewal, use home peelings and special brushes for washing, do not bring the skin to a critical condition;
- moisturize and nourish the skin from the outside to avoid drying and peeling. Restoring the water balance of the epidermis is extremely important for successful treatment;
- squeeze out pimples yourself
- regularly , undergo all prescribed procedures and follow recommendations.
Millums (millet)
This type of bump occurs with equal frequency on the upper and lower eyelids. Millet grains can range in size from a poppy seed to a grain of rice and usually form in groups. Millums are the most harmless of all formations and cause only aesthetic discomfort. At its core, these are whiteheads localized in the eyelid area.
Millet removal should only be done by a cosmetologist. Since they do not carry the risk of complications, they are not considered an ophthalmological disease, but fall within the competence of a dermatologist-cosmetologist.
Prevention of millums includes caring for the eyelids, timely removal of dead epidermal cells, ensuring the cleanliness of the ducts of the sebaceous glands and pores of the skin around the eyes, as well as a balanced diet that excludes excessive consumption of fatty foods.