A scrotal abscess is an encapsulated purulent lesion in the tissues of the scrotum. May be primary or secondary, superficial or intrascrotal. Rarely seen. It develops during infection with atheromas, surgical interventions and traumatic injuries, or is a complication of a bacterial infection in the area of the testicle and its epididymis. Symptoms of a scrotal abscess are intense pain, swelling, hyperemia and local hyperthermia in the affected area. An increase in body temperature to febrile levels, weakness, fatigue, headache, pain in joints and muscles are observed. Treatment is surgical, requiring opening and drainage of the abscess along with antibacterial therapy.
General information
Scrotal abscess is a rare pathological condition. The frequency of development is unknown; isolated cases are mentioned in the literature without indicating the prevalence of the disease. It may occur primarily or develop against the background of other pathological processes. Most often, scrotal abscesses are diagnosed, which are a complication of acute purulent epididymo-orchitis.
Despite the rather superficial location of the purulent focus, the disease can present difficulties during diagnosis due to pronounced edematous-infiltrative processes and diffuse pain in the area of abundantly innervated soft tissues of the scrotum, perineum and penis. Treatment of scrotal abscess is carried out according to the general principles of purulent surgery. Treatments are carried out by specialists in the field of andrology and urology.
Abscess of the scrotum
Risk factors
The appearance of an abscess in the male gonads can be caused by:
- STI,
- poorly performed surgical operations,
- inflammatory diseases of the reproductive system - orchitis, prostatitis, orchiepididymitis, urethritis,
- decompensated diabetes mellitus,
- infection with ARVI due to HIV,
- testicular tuberculosis,
- severe hypothermia of the scrotum.
The risk of developing an abscess increases if a man smokes or drinks alcohol for a long time. General intoxication of the body only worsens the condition during purulent inflammation.
Causes
The causative agent of the purulent process is most often hemolytic staphylococcus, Staphylococcus aureus or microbial associations. Less commonly diagnosed are scrotal abscesses caused by salmonella, brucella, spirochetes pallidum, candida and anaerobic microorganisms. Local factors contributing to the development of scrotal abscesses include
- small thickness of the epidermis
- increased moisture in the skin of the organ
- loose subcutaneous tissue
- a large number of sweat and sebaceous glands.
Due to the proximity of the urethra and anus, the skin of the scrotum gets exposed to a large number of highly virulent microorganisms that can cause an abscess. The peculiarities of blood and lymph supply to the scrotum create favorable conditions for slowing the outflow of fluid and the development of pronounced edema against the background of thrombophlebitis and lymphostasis.
Common predisposing factors that increase the likelihood of developing a scrotal abscess are
- non-compliance with personal hygiene rules by socially disadvantaged patients
- immunity disorders due to chronic somatic diseases, obesity, diabetes, malignant neoplasms, AIDS, drug addiction and alcoholism.
The immediate cause of scrotal abscess in adults is most often purulent inflammation of the testicle and its epididymis. Less commonly, pyoderma (pustular lesions, boils, carbuncles), suppuration of atheromas, open traumatic injuries (puncture and incised wounds, gunshot wounds) and infection in the area of postoperative wounds are indicated as the cause of this pathology.
Cases have been described in which a scrotal abscess in adults developed in Crohn's disease, paracolitis and acute destructive pancreatitis as a result of the spread of infection through the tissue of the retroperitoneum and pelvis. In young children, the cause of a scrotal abscess is sometimes the spread of an infectious process from internal organs to the scrotum through the patent processus vaginalis of the peritoneum.
1.General information
The testicle and its epididymis, the spermatic cord, as well as orchitis, epididymitis, funiculitis - all these terms refer only and exclusively to men. Due to the evolutionary division into two sexes and the corresponding anatomical dimorphism, functionally similar formations in women are located inside, in the abdominal cavity; they are called differently, and only their inflammations are designated according to the same principle - by adding the “inflammatory” suffix “-itis”, generally accepted in medicine.
The term “abscess” is also universal. Its features (unlike inflammation in general) are the obligatory presence of a pyogenic infectious pathogen, localization in a limited area, disintegration (purulent melting in medical terminology) of functional tissue and the formation of a high-pressure capsule filled with exudate.
The testicles, as you know, are a paired organ of the male reproductive system, hidden in a leather pouch - the scrotum, which, in turn, is located in the groin at the base of the penis. Each testicle in its rear part, mainly at the upper pole, is equipped with the so-called. epididymis, a narrow labyrinth-incubator of sperm, which, when maturing, at the right moment enter through the duct in the spermatic cord (which also serves as a mechanical “suspension” of the testicle) into the seminal storage vesicle, are saturated with the energy carrier fructose, and from there they are released into the urethra, where mixed with the secretion of the prostate gland and form the final composition of the fertilizing ejaculate, or sperm.
Sign up for a consultation
Inflammatory processes of the testicle are generalized by the term “orchitis”, of the epididymis - “epididymitis”, of both formations at the same time - orchiepididymitis. Any of these types of inflammation is dangerous in itself, and any of them can be further complicated by the formation of an abscess. In approximately every fifth case, inflammation leads to infertility; with a probability of about 65%, an atrophic process may begin in the testicular structures. In many cases, abscessation of the testicle and/or epididymis leaves no choice other than orchiectomy (surgical removal of the testicle). In other words, any signs of inflammation in these organs require immediate specialized medical care.
A must read! Help with treatment and hospitalization!
Classification
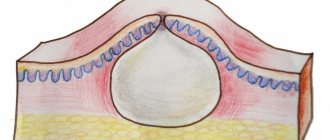
Taking into account localization, the following are distinguished:
- superficial (located in the skin and superficial layers of the organ)
- internal or intrascrotal (intratesticular and intravaginal) scrotal abscesses.
Taking into account the reasons for development, they distinguish:
- primary
- secondary (complications of another pathological process) lesions.
Superficial purulent foci can be either primary or secondary. Internal abscesses of the scrotum are usually secondary in nature and arise as a result of the spread of infection from the organs of the scrotum, less often from other anatomical areas.
Symptoms of a scrotal abscess
Scrotal abscess is characterized by rapid development. The patient experiences pain and swelling in the scrotum area. Over the next few days, there is a sharp increase in pain and progression of swelling. The skin of the scrotum turns red, and there is an increase in local temperature. Local symptoms of a scrotal abscess are combined with general signs of a purulent process. The patient complains of weakness, weakness, headaches and muscle-joint pain. An increase in temperature to 38-39 degrees is detected.
In some cases, a septic variant of the scrotal abscess is observed with rapid progression of symptoms and pronounced systemic inflammatory reactions. When infected with fungi, pale spirochete and Mycobacterium tuberculosis, an erased course with moderate pain and an increase in temperature to subfebrile levels can be observed. If left untreated, the scrotal abscess may rupture and further spread the infection. Sometimes, due to impaired blood flow in the skin of the scrotum, hemorrhages occur, followed by the formation of superficial foci of infection in the affected tissues.
Symptoms
A testicular abscess makes itself felt by the following signs of inflammatory processes:
- enlargement and swelling of the scrotum,
- pronounced pain in the testicle on the affected side,
- temperature rise to 39-40 degrees,
- chills, weakness and other manifestations of intoxication,
- admixture of blood in semen,
- pain when urinating.
With these symptoms, you cannot postpone a visit to a urologist-andrologist. As a rule, the correct diagnosis is made based on the results of a visual examination. Additional examinations may include ultrasound of the scrotum, blood tests, and PCR diagnostics to exclude tuberculosis.
Diagnostics
When examining a patient with a scrotal abscess, significant swelling, local hyperemia and hyperthermia in the affected area are revealed. The scrotum is sharply painful on palpation. The following diagnostic procedures are carried out:
- Ultrasound of the scrotum. To clarify the location and stage of the abscess, sonography is usually prescribed.
- Laboratory research. Blood tests reveal an increase in ESR and leukocytosis with a shift to the left.
If the spread of an infectious process from the pelvis, abdominal cavity or retroperitoneal space is suspected, CT and MRI are used, which make it possible to obtain information about the condition of several anatomical areas, to clarify the localization of the primary focus and the route of spread of the infection.
2. Reasons
The main routes of infection into the testicle are hematogenous (through the bloodstream) and lymphogenous (through the lymphatic ducts); The pathogenic agent almost always enters the appendage with blood. It is generally accepted that up to half of all cases of orchiepididymitis are caused by chlamydia, but the causative agent of the inflammatory process in the testicle can be almost any pathogenic or opportunistic microorganisms - viruses, bacteria, intracellular parasites, fungal cultures - delivered from the primary foci of acute or chronic infectious diseases. inflammatory process (lungs, intestines, urethra, skin, oral cavity, nasopharynx, etc.). Trauma, partial torsion, seminal granulomatosis, treated or untreated STDs and other factors that disrupt the integrity, anatomy or natural protection of the testicle can play a provoking role.
Visit our Urology page
Treatment for scrotal abscess
The patient is urgently hospitalized in the andrology or urology department. In the early stages, antibacterial and anti-inflammatory drugs are prescribed. After the abscess has “matured,” the scrotal abscess is opened and drained. In case of severe destructive processes in the testicular area, an orchiectomy is performed. When the purulent process spreads from other anatomical areas, the scope of intervention is expanded. Subsequently, dressings are performed and antibacterial therapy is adjusted taking into account the sensitivity of the microflora.
3. Symptoms, diagnosis
It is almost impossible not to notice the inflammatory process in the testicle, and even more so with the formation of an abscess: the main subjective symptom is intense pain. Sometimes patients describe it as pulling or aching, depending on the position of the body, erection and/or ejaculation, periodic - but most often the pain is sharp, constant and increasing. The affected testicle also reacts with acute pain to diagnostic palpation. In addition, there is often a significant increase in local and general temperature, severe malaise, and irradiation of pain to adjacent areas. The testicle increases in size (in severe orchitis - more than five times), turns red, becomes tense, and the epididymis becomes significantly denser.
A clinical blood test is diagnostically informative (a characteristic shift in the leukocyte formula is revealed); According to indications, ultrasound or other imaging methods are prescribed. In situations of differential diagnosis, when it is necessary to exclude, for example, a rapidly growing tumor, testicular tuberculosis, etc., a biopsy is performed.
About our clinic Chistye Prudy metro station Medintercom page!
Forecast
The prognosis for life with a scrotal abscess is usually favorable. With a long course of the disease, the formation of fistulas and edema in the perineal area and perirectal tissue is possible. A rare but dangerous complication of scrotal abscess is Fournier's gangrene - fulminant necrosis of scrotal tissue. The probability of death from this complication, according to various sources, ranges from 50 to 80%. In the long-term period after a scrotal abscess, dysfunction of the testicle, epididymis and vas deferens is sometimes observed with the development of androgen deficiency or male infertility.
You can share your medical history of what helped you in treating a scrotal abscess.