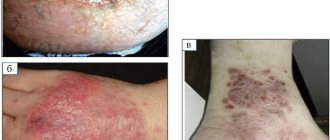
Seborrheic eczema in the photo
Photo 1. Seborrheic eczema of the face
Photo 2. Seborrheic eczema of the neck
Photo 3. Seborrheic eczema on the head
Photo 4. Seborrheic eczema
Like seborrheic dermatitis, seborrheic eczema develops due to the activity of microorganisms: Pitysporum ovale, Candida fungi and Staphylococcus bacteria. Patients with seborrheic dermatitis and related neuroendocrine diseases have an increased risk of developing seborrheic eczema, but in general it can develop at any age and regardless of gender.
True eczema
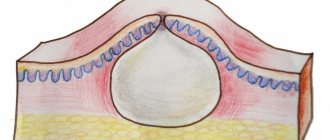
This variant of the disease is characterized by frequent exacerbations and is manifested by inflammatory reactions in symmetrical areas of the skin. The affected areas become red and swollen, and weeping surfaces with a large number of small blisters filled with serous contents are found. After the vesicles break through, small erosions form. Their surface resembles “serous wells” due to opalescent droplets of exudate.
As the disease progresses, the number of newly formed blisters decreases, erosions become covered with crusts, which subsequently transform into a scaly, scaly surface.
The main clinical manifestation of true eczema is a pronounced polymorphism of the elements of the rash. On the affected areas of the skin, rashes are detected at various stages of their resolution.
The basis for diagnosing this disease is the typical clinical picture. Most patients have a history of allergic conditions or recent emotional distress.
Causes of seborrheic eczema
Seborrheic eczema, like seborrheic dermatitis, occurs due to the proliferation of microorganisms in the mouths of the sebaceous glands. However, the main causative agent of the disease - Pitysporum ovale - is present on the surface of the skin of almost any person, but rashes occur only in a small percentage of the population. Scientists and dermatologists still cannot answer exactly why this happens, but possible reasons for the development of seborrheic eczema have been identified:
- heredity;
- hormone imbalance and metabolic disorders;
- disruption of the endocrine system;
- disruption of the digestive system, including the liver and gallbladder, intestines;
- weak immunity and hypovitaminosis;
- physical and psychological fatigue.
Seborrheic eczema worsens in winter, when the body suffers from a lack of vitamins and microelements. It is worth remembering that the acute period is accompanied by severe itching, which leads to the formation of wounds. Due to reduced immunity, these wounds become gateways for infection.
Types of eczema:
Eczema is an idiopathic disease. The reasons why it appears are not fully understood. Doctors know several factors that, in combination or individually, can trigger a particular set of symptoms. For example, gastrointestinal pathologies, thyroid dysfunction, varicose veins, and psycho-emotional stress can lead to the development of eczema rash.
True eczema
True eczema is chronic, manifested by a cyclical development from exacerbations to relapses. A distinctive feature of the disease is the presence of symmetrical inflammation on the body. This diagnosis can be made based on the indicated symmetrical distribution of the rash, the presence of small vesicles (small pappulous rash), and polymorphism. By identifying an allergy to something and a history of stress, the accuracy of the diagnosis increases.
Stages:
- erythematous - the skin becomes noticeably red;
- papulovesicular - vesicles appear;
- weeping - the bubbles burst and microerosions form in their place;
- crusts appear.
As a rule, all stages are observed simultaneously.
Inflammations in this type are swollen, reddened, the surface becomes wet from the secreted exudate. A characteristic manifestation is the “serous well” syndrome, when the secretion lies in drops, resembling dew. Within the focus of inflammation there are vesicles with contents and crusts. In addition to foci of inflammation, there are scattered dry rashes on the body. If a person has been suffering from this disease for a long time, the quality of the skin gradually changes. Such patients are characterized by infiltration, hyperemia, and hyperpigmentation. The skin pattern becomes more pronounced, the skin thickens.
Microbial eczema
The causes of microbial eczema are factors associated with varicose veins (varicose eczema), trauma (paratraumatic), and fungal infections (mycotic). The cause of development is the basis for selecting treatment.
The lesions are asymmetrical, as is the case with the previous type. As a rule, foci of inflammation are located in the lower part of the body - in the projection of the veins. The second option is skin folds where intense sweating occurs. The basis for diagnosis is anamnesis, symptoms, microscopy, bacteriological, histological examination:
- microscopy reveals signs of mycosis in the form of mycotic cells;
- a bacteriological study determines the type of fungus and the drug to which it is sensitive;
- histology reveals widespread lymphoid infiltration with plasmacytic elements, epidermal localization of blisters, sclerotic changes in the skin (if microbial eczema has lasted for a long time).
The spots have uneven edges, the skin around them is thickened, red and blue. There are weeping crusts on the spots. Dry single rashes may form on the periphery. Often this type is complicated by additional diseases.
Seborrheic eczema
Eczema is localized in a characteristic way - on the head, in anatomical folds, behind the ears, on the folds. In the area of hair growth, dry skin and redness are noticeable, peeling marks separate from the spots, and the patient experiences itching. Inflamed spots have defined boundaries. They are dry, but sometimes serous-purulent or serous crusts appear, after removal of which eroded weeping spots appear.
With inflammation in the folds, deep cracks, swelling, and swelling appear. Sometimes lesions appear on the body, mainly in the lower part. They are clearly defined, yellowish-pink in color, flaky, and a rash is observed in the middle part. Some doctors consider seborrheic eczema to be seborrheic dermatitis or true complicated eczema. However, these diseases can be distinguished histologically.
The cause of occupational eczema is regular contact with irritating substances. The trigger for the onset of the disease can be microtraumas, chemical and aggressive drugs, and dust. In combination with existing allergies or impaired vascular permeability, this results in rashes. The clinical picture is similar to true eczema. Rashes are localized in areas of contact with the allergen, but can occur throughout the body.
The diagnosis is made taking into account the clinical picture and evidence that exacerbations occur upon contact with certain substances. This type may also be indicated by the fact that the symptoms disappear during the holidays.
Dyshidrotic eczema
The causes of dyshidrotic eczema are disturbances in the activity of the sweat glands. Additional causes include contact with substances that are known to be allergenic. Exacerbations are typical during summer time or periods of severe stress. As a rule, the first symptoms affect the fingers - rashes begin to appear on the sides, after which they spread to other areas.
Treatment of seborrheic eczema
Seborrheic eczema requires long and painstaking treatment, which includes not only getting rid of symptoms, but also treating the underlying disease. Thus, parallel treatment by a gastroenterologist or endocrinologist is required if the cause of the development of seborrheic eczema is a disease of the gastrointestinal tract or endocrine system. In addition, it is necessary to take antibiotics and antimycotic drugs orally.
In parallel with the treatment of concomitant diseases, agents for external use are prescribed. To block inflammatory receptors, glucocorticoid ointment is prescribed. It eliminates itching and accelerates cell regeneration. Depending on the causative agent of the disease, antifungal or antibacterial ointments are used. Measures may also be prescribed to degrease the skin, for example, treating wet wounds with brilliant green, an alcohol solution with the addition of salicylic acid, or powder with the addition of sulfur or resin. These measures are designed to normalize the functioning of the sebaceous glands and reduce the intensity of weeping wounds.
If the rashes are localized on the scalp, the same treatment is prescribed as for seborrheic dermatitis, namely the use of shampoos containing naphthalan, tar, selenium sulfide, salicylic acid, sulfur, zinc pyrithione.
Diagnostics
The identification and treatment of seborrheic type eczema is carried out by a dermatological specialist. Basically, an external examination of the affected areas of the patient is sufficient to make a diagnosis.
Studies may be ordered to confirm
:
- dermatoscopy;
- analysis of scrapings of the affected area for fungus;
- histological examination, etc.
During diagnostic measures to detect side pathologies and infections, patients may be prescribed consultations with specialists in other fields: gynecologist, ENT specialist, endocrinologist, etc. In addition, additional examinations may be required: ultrasound of the abdominal cavity and pelvic organs, gastroscopy, blood tests, rhinoscopy, etc. As part of the diagnosis, it is necessary to distinguish seborrheic eczema from occupational eczema, from skin diseases such as microsporia, psoriasis, etc. All these pathologies have outwardly similar symptoms.
Treatment of seborrheic eczema with drugs Losterin
Patients with seborrheic eczema should avoid regular cosmetic shampoos, as well as shower gels and soaps, mainly because perfume compositions and surfactants irritate the skin. It is preferable to replace hygiene products with gels specially designed for sensitive and irritated skin, for example, “Losterin” gel. It carefully cleanses damaged skin, disinfects its surface and has antimycotic and antibacterial effects. Another advantage of the “Losterin” gel is that it softens and nourishes the skin due to the content of vegetable oils.
After the acute period has passed, products are needed to remove crusts, restore the epidermis and reduce itching. Under no circumstances should crusts be removed “dry”, otherwise open wounds will form and treatment will not make sense. If the crust is ready to come off, it can be easily removed with olive or sea buckthorn oil by soaking a cotton swab in it. Then a cream is applied to the exposed delicate surface to promote cell regeneration, strengthen collagen fibers, and normalize metabolism in the epidermis. These creams may contain tar, zinc, deresined naphthalan, panthenol, retinol, sulfur, salicylic acid and urea.
Losterin cream is preferred for the treatment of seborrheic eczema due to its powerful regenerative properties. Urea and salicylic acid in its composition have a keratolytic effect, and nutrition and cell restoration are ensured by the simultaneous action of almond oil, dexpanthenol and Japanese Sophora extract.
Physical therapy can also help speed up recovery. For patients with seborrheic eczema, cryomassage, laser and magnetic therapy, and darsonval are prescribed.
To avoid exacerbation, patients are prescribed to adhere to a hypoallergenic diet (especially in winter) with the exception of citrus fruits, seafood, nuts, whole milk, honey and canned foods.
Principles of treatment
Treatment begins with the establishment and elimination of provoking factors, which are partially listed at the beginning of the article. It will not be possible to cure the disease if you are under stress and psychophysical strain, constantly in contact with substances that cause allergic manifestations, without eliminating microbial or fungal infection.
For any type of eczema, the following have a positive effect:
- drug treatment - taking sedatives and antihistamines;
- plasmapheresis and other methods of extracorporeal hemocorrection;
- vitamin therapy (local and internal) for cell regeneration.
In case of exacerbation, generalized nature and inability to stop the recurrence of the disease, glucocorticosteroids can be added to treatment. Ointments and pastes with keratolytic properties are effective for local treatment. They save the patient from itching and contain anti-inflammatory components. To facilitate the drying of inflammation, special powders, mash, and ointments are used. Spots should be protected from aggressive external influences - wind, frost, sun.
A wide range of physiotherapeutic procedures are used for treatment:
- ozone therapy - flowing carbonation with a special mixture of gases or irrigation and lotions with ozonized water;
- magnetic therapy – the patient is exposed to a magnetic field in a special device;
- laser treatment;
- cryotherapy - use of a cryosauna or cryotreatment of affected areas;
- ultraviolet irradiation;
- baths.
A physiotherapist selects a set of procedures on an individual basis.
In most cases, treatment can be carried out at home, but for some types of disease (cellulitis, herpetic eczema, exfoliative dermatitis), the doctor may recommend hospitalization. To the treatment procedures it is necessary to add a special diet, cessation of smoking and alcohol, enhanced hygiene to avoid infection of wounds, and the correct selection of detergents and creams.
The diet is selected individually. As a rule, smoked products, spicy foods, pickles, canned food, coffee, citrus fruits, bakery and confectionery products are completely excluded. Porridge, fermented milk products, and vegetable soups help cope with exacerbations with balanced therapy.
Prevention of seborrheic eczema
Preventive measures for seborrheic eczema are aimed at preventing exacerbation. These include:
- diet – it is necessary to minimize the consumption of potentially allergenic foods;
- personal hygiene – excessive sebum production makes it necessary to shower 1-2 times a day. The water should be warm, for hygiene it is necessary to use products specially designed for sensitive skin;
- limiting external irritants - chemicals can irritate and injure the skin. Therefore, it is necessary to do work that involves contact with chemicals, wearing gloves, and dressing in natural, well-ventilated fabrics;
- timely treatment of chronic diseases;
- regular examinations by a dermatologist and tests.
Prevention
The manifestations of seborrheic eczema can be kept under control by organizing a healthy lifestyle with careful skin care throughout the body.
Of great importance are:
- balanced diet with the exclusion of allergens;
- regularly wash your hair with a gentle shampoo;
- refusal of cosmetics with aggressive components;
- course intake of vitamins and minerals;
- ensuring a stable psycho-emotional state.
Properly organized treatment and subsequent supportive measures will bear fruit - the skin will be cleared of scales, oily shine will disappear, and there will be no need to mask defects in other ways.
Bibliography
- Ado A.D. General allergology. M.; "Medicine", 1970.-543 p.
- Results of a study of the effectiveness of non-halogenated corticosteroids in the treatment of chronic eczema / I.M. Korsunskaya, N.A. Lukashova, Z.A. Nevozinskaya, E.E. Agafonova // Clinical. dermatology, venereology. 2008. - No. 4. — P. 101-105.
- Ryzhko, P.P. The use of antihistamines in the treatment of various dermatoses / P.P. Ryzhko // Ukr. magazine dermatology, venereology, cosmetology. 2002. - No. 1. — P. 39-41.
- Skripkin, Yu.K. Allergic dermatoses / Yu.K. Skripkin, B.A. Somov, Yu.S. Butov. M.: Medicine, 1975. - 245 p.
- Tishchenko, A.L. Optimal therapeutic doses of vitamin A in patients with eczema and psoriasis / A.L. Tishchenko // Vestn. dermatology and venereology. 1998. - No. 4. — P. 36-38.
- Turchina, I.P. Complex treatment of patients with eczema and neurodermatitis localized on the lower extremities / I.P. Turchin // Dermatovenerology, cosmetology, sexopathology. 2002. - No. 1-2 (5). - S. 98101.
- Yusupova, L.A. Treatment of patients with eczema / L.A. Yusupova, R.Kh. Kha-fizyanova // Ross. magazine skin diseases. 2005. - No. 6. — P. 20-22.
- Brazzini, B. New and established topical corticosteroids in dermatology: Clinical pharmacology and therapeutic use / B. Brazzini, N. Pimpinelli // Am. J. Clin. Dermatol. 2002. - N3. — P. 47-58.
- Buznikov, GA Serotonin and serotonin-like substances as regulators of early embryogenesis and / GA Buznikov, HW Lanbert, JM Lauder //Cell Tissue Res. 2001.-N 39.-P. 177-186.
- Catania, A. Inhibition of acute inflammation in the periphery by central action of salicylates / A. Catania, J. Arnold, A. Macaluso et al. //Proc. Natl Acad Sci USA. 1991. -Vol.88, N19. -P. 8544-85
Why does eczema develop?
Medical science does not yet have a clear answer to this question.
There are several key points:
- Hereditary hyperreactivity of the skin. That is, in response to a minor impact, an inadequately significant reaction occurs.
- Functional disorders of various systems (nervous, endocrine, digestive), both congenital and acquired; changes in trophism (nutrition) of tissues.
- Sensitization, that is, increased sensitivity (aka allergy) to various agents. They can be external: chemicals, medicinal, food, household, industrial, biological, microbial allergens. And also come from the internal environment of the body: products of altered metabolism, microbial allergens from foci of chronic infection.
For each type of eczema, certain factors are of greater specific importance.
Effective treatments for eczema
Cryotherapy
NeoGen procedure
Plasma therapy
One of the fairly common skin diseases is eczema. It is an inflammation accompanied by redness, itching and the appearance of tiny blisters with liquid. It is the latter that explains the name of the disease: such bubbles resemble the boiling of water, from the Greek eczeo means “to boil.”
According to statistics, up to 2% of the world's population suffers from eczema. And in the practice of dermatologists, such pathology occurs in almost 40% of all skin diseases. Most often, patients come with the problem of the appearance of foci of inflammation on the arms, legs, body and head. The rash goes through several stages of development, over time developing from simple redness into weeping erosion and severe peeling. Against the background of such pathology, secondary purulent infections often develop. Without treatment, noticeable cosmetic defects remain on the skin that do not go away over time.
Let's figure out why eczema occurs, how to suspect its development and how such a pathology is treated.
Stages of the disease
If we talk about the features of the course of the disease, then there are usually three stages of its development:
- Spicy. It is characterized by the appearance of vesicles on swollen skin, point erosions with weeping, serous crusts, etc. The rashes are multiple in nature.
- Subacute. This stage is characterized by erythema, redness and scaling.
- Chronic. It is characterized by infiltration and strengthening of the “skin pattern”, the appearance of pigmentation.
Symptoms of eczema
Depending on the cause of the disease and the location of the inflammation, symptoms can vary significantly. Most often, patients experience the following manifestations of skin eczema:
- At the erythematous stage, red inflammatory spots appear, which gradually merge with each other.
- At the papular stage, bright red nodules with clear boundaries are formed.
- At the vesicular stage, bubbles with transparent contents appear.
- At the stage of weeping, the bubbles open, point erosions are formed with the release of exudate.
- At the cortical stage, grayish-gray crusts are found, under which the skin heals.
- At the peeling stage, crusts and scales are removed from the surface of the skin.
Symptoms of the disease go away with the elimination of provoking factors. However, the healed area of skin has an uneven color and dense texture.
What other symptoms may indicate the development of eczema:
- The scaly layer at the border of the scalp. Develops with seborrheic eczema. At the initial stage, it manifests itself as single yellowish nodules that quickly grow. Subsequently, a scaly layer forms along the border of the hair.
- Round rashes on hands. Appear in almost 80% of cases of eczema development. At the initial stage they have a rounded shape, but over time they lose it.
- Rashes with clear edges. Most often found on the legs. They can be seen with varicose veins, the rashes have a round shape and pronounced borders.
Symmetrical rashes on the body. They are located all over the body and often peel off. At the initial stages they look typical - they are bubbles with liquid, later areas of thickened skin with severe peeling appear.- Callus-like rashes on the palms. Such formations, especially in places atypical for calluses, also indicate eczema. Bubbles form, but due to the thick skin they may not open.
- Bubbles in the armpit with a hair in the center. Rashes with a hair in the center are a sign of sycosis - damage to the hair follicles. As a rule, such rashes are accompanied by itching and redness.
- Lumps on the face and hands. Such formations do not ooze or crust, and often appear on the face.
- Itchy redness on the arms and legs. Indicate true or microbial eczema. Accompanied by multiple vesicles.
- Suppuration around the wounds. With the development of microbial pathology, purulent crusts and skin hyperemia appear.
The symptoms of eczema are often similar to atopic dermatitis. However, it is worth understanding that pathologies also have significant differences. Dermatitis usually occurs in childhood, while eczema is found in adults and even elderly patients. Another difference is that the first pathology is most often localized on the elbows and knees, neck and face, while eczema can be located on any area, but more often on the hands and legs. Dermatitis occurs suddenly and often disappears. Eczema appears regularly and is often the immediate result of exposure to a specific allergen.
Diagnosis of eczema
The diagnosis is made based on examination and questioning of the patient. In some cases, additional tests may be prescribed to differentiate eczema from other skin diseases. With true eczema, the clinical picture of the disease is typical. In other cases, symptoms may be similar to atopic dermatitis, toxicerma and allergic contact dermatitis.
The diagnostic process may include:
- general blood analysis;
- tissue scraping for examination under a microscope;
- allergy tests to identify the source of allergies;
- histological examination of tissues.
Treatment is prescribed only after confirmation of the diagnosis and determination of the existing type of pathology.
Features of treatment
The key to treating eczema is to identify and minimize triggers. In addition, systemic or local therapy is prescribed, as well as various physiotherapeutic procedures:
- Systemic therapy. It is based on taking antihistamines, which help prevent an acute allergic reaction. Sedatives, glucocorticosteroids and a number of hormonal drugs are also used.
- Local therapy. May include the use of retinol ointment, anti-inflammatory and antiseptic agents. Therapy is selected taking into account the identified form of eczema and the causes of its occurrence. For example, treatment for a virus or fungal infection may be required.
- Physiotherapy. As a rule, it includes ozone therapy, magnetic therapy and laser therapy. In difficult cases, it is possible to treat eczema lesions using cryotherapy. Medicinal and mud baths, exposure to ultraviolet radiation, etc. are often prescribed.
Preventive measures
Diet and lifestyle play an important role in preventing the development of new exacerbations. The diet should exclude any foods that can trigger allergic reactions. Typically this is:
- red berries;
- citrus;
- Fish and seafood;
- chocolate;
- dairy products.
Patients are also advised to give up alcohol and smoking.
Personal hygiene is also important. If eczema of the feet, legs, arms and face develops, it is recommended to avoid scented soaps. Water-based creams can be used to moisturize the skin.
And most importantly, improper treatment of skin diseases can trigger eczema. This means you should not self-medicate. If any rashes and redness appear, do not delay a visit to a dermatologist, because this can be the key to a quick and successful recovery.
If you are faced with the symptoms of eczema and do not know how to get rid of such a disease, then the dermatologists of our KallistoMed clinic are ready to help in this matter. We will be waiting for you at the reception - sign up using the website or by calling the numbers provided!
How to deal with eczema?
This is far from an easy task. Indeed, despite the fact that all types of eczema develop approximately according to the same scenario, the triggering factors in each case are completely different.
You must understand that in order to successfully combat the disease, it is advisable to identify and eliminate them. And if the wound heals, and mycosis can be successfully treated, then it is already more difficult to eliminate advanced varicose veins. But it is generally beyond our power to grow a new limb in place of a stump or change the genetic constitution.
Therefore, the battle with eczema is a long process that requires constant interaction between the patient and the doctor and constant work to follow the recommendations (diet, regimen, skin care).
You must be prepared for the fact that even if you have the most competent doctor and carefully follow all the advice, exacerbations will still occur from time to time. After all, we cannot influence all provoking factors.
The main thing to remember is that everything passes, and this exacerbation will pass. The main thing is to maintain a calm and positive attitude, since stress is the primary provocateur of all illnesses.
Some recommendations
Nutrition for eczema
Eczema is an allergic disease, so following a hypoallergenic diet is one of the most important points in the fight against the disease.
Naturally, not every person suffering from eczema has intolerance to all those foods that are recommended to be excluded from the diet.
Dietary restrictions are based on the fact that many foods, simply by virtue of their composition, are capable of provoking and maintaining the inflammatory process. For example, histamine is formed in sea fish when frozen. This is exactly the substance to which we owe burning, itching, redness and swelling during allergic reactions.
Rational skin care
We all know that we must observe personal hygiene measures, keep ourselves clean, etc.
However, among northern peoples who live in harmony with nature, but do not have the habit of taking a hot shower every day, eczema does not occur.
Healthy skin is covered with a protective water-fat mantle. This peculiar film has a certain composition, a slightly acidic reaction and is inhabited by our “native” microorganisms. All this, together with the stratum corneum of the epidermis, prevents excess moisture loss and protects against the penetration of unwanted substances and creatures into the skin.
It has been proven that after intensive washing in hot water with soap and a washcloth, protective mania is restored within 24 hours. Accordingly, if you wash with fanaticism, even a healthy person can be driven to eczema.
If eczema has already occurred, then the skin barrier is already broken. Therefore, water procedures are generally prohibited in the acute stage, and limited in the chronic stage.
The skin of a patient with eczema is constantly in a state of combat readiness to respond with inflammation to minor irritation. Therefore, the water should be warm (37 - 38 °C), the sponge should be soft, the soap should be thin (and preferably not alkaline), and the towel should be fluffy. After washing, the skin should not be rubbed, but blotted.
To restore the barrier and stop water loss through the skin, emollients (moisturizers) are always included in the eczema treatment complex. These are preparations in the form of milk or cream that have a specially selected composition and do not contain fragrances, dyes or preservatives (so as not to provoke an allergic reaction). At this stage, the choice of such products in pharmacies is very wide.
If the skin of the hands is affected
The skin of the hands receives the maximum number of harmful effects, so hand eczema is one of the most common manifestations, especially in women.
Some useful tips for this case:
- Wash your hands with water at room temperature using a soap substitute. It is advisable to exclude soap.
- Avoid direct contact with irritating substances (household chemicals, solvents, fuels and lubricants), and with the ground. If possible, with shampoo when washing your hair (wash your hair with plastic gloves).
- Do not wear rings as liquids and detergents will accumulate underneath them.
- Avoid latex gloves (many people are allergic to it). You can use polyethylene, polyvinyl chloride, nitrile gloves.
- Do not use gloves with talc - it dries out and irritates the skin.
- Do not wear gloves for more than 20 minutes without a break. You can wear cotton gloves under protective gloves.
- In cold weather, be sure to wear mittens or gloves outside to prevent chapped skin.
These recommendations should be followed for at least 6 months after the symptoms of eczema disappear, since skin resistance is not restored immediately.
Adequate sleep and rational physical activity
Eczema is a dermatosis in which there are disorders of both the nervous and vascular systems. It is impossible to organize their work if a person is overtired and stressed.