Eyelids are movable folds of skin that protect our eyes from dryness, dust, bright light and other negative factors of the surrounding world.
The top of the eyelids is covered with thin and delicate skin, penetrated by a large number of blood vessels.
Beneath the skin is muscle tissue that allows you to easily open and close your eyes.
1
Diseases of the skin around the eyes and eyelids. Diagnosis and treatment
2 Diseases of the skin around the eyes and eyelids. Diagnosis and treatment
3 Diseases of the skin around the eyes and eyelids. Diagnosis and treatment
At the back of the eyelid are the meibomian glands, which produce a liquid secretion to keep our eyes moist and improve the contact between the eyelids and the ocular surface.
The mucous membrane of the eye is lined by the conjunctiva with lacrimal glands, which contributes to additional hydration of the eyeball and protection against infections.
Inflammation of each of the organs that make up the eyelid causes the development of a number of characteristic diseases.
Why does swelling of the eyelid occur?
The skin's ability to stretch, loose structure and a large number of blood vessels lead to fluid quickly accumulating in the eye area.
There are various reasons for the appearance of swelling of the eyelids, but from the symptoms you can understand what triggered fluid retention in the body.
If the swelling of the eyelid is bilateral, combined with other edema of the body, and the skin on the eyelids is pale and cold to the touch, this indicates renal or heart failure, as well as severe anemia.
Swelling of the eyelid also occurs with head injuries and angioedema.
Many inflammatory eye diseases, such as the following, are also accompanied by swelling of the eyelids:
- stye, abscess, blepharitis, contact dermatitis and other inflammations of the eyelids;
- diseases of the paranasal sinuses;
- acute purulent, pseudo- and membranous conjunctivitis;
- phlegmon, acute dacryocystitis and other diseases of the lacrimal sac;
- ednophthalmitis, iridocyclitis and other pathologies of the eyeball.
Swelling of the eyelids (most often unilateral) is characterized by redness of the skin, pain on palpation and a local increase in temperature.
Symptoms
In the early stages, pigmentation appears in the form of small spots of a light shade. The mechanism of occurrence of the pathological area is associated with the destruction of melanocytes. The area under the eyes is susceptible to vitiligo, as it is the most sensitive area.
At the initial stage of development, the disease is observed by the appearance of small white zones. As the disease progresses, the spots unite together, which externally forms large-scale affected areas. Patients are often diagnosed with a chronic form of the disease, but exacerbations of the pathology are possible in the spring and autumn. It is advisable to protect the affected areas from exposure to ultraviolet radiation.
Symptomatically, vitiligo is accompanied by:
- changeable pigmentation under the visual apparatus;
- redness in this area;
- intensive production of sebaceous secretions;
- peeling;
- areas with thickenings;
- discoloration of hairs on the skin;
- sweating disorders.
The patient's general condition remains normal. A patient with vitiligo experiences psycho-emotional discomfort in society.
Causes of inflammation of the eyelids
Inflammation of the eyelids can be caused by the following reasons:
- pathological activity of mites living in the skin (a common phenomenon when the immune system is weakened);
- allergic reactions to certain types of medications, plant pollen, food;
- viral and microbial infections in the body;
- chemical, thermal and mechanical eye injuries;
- disruption of the cardiovascular and nervous systems;
- endocrine and hormonal disruptions.
1 Diseases of the skin around the eyes and inflammation of the eyelids. Diagnosis and treatment
2 Diseases of the skin around the eyes and inflammation of the eyelids. Diagnosis and treatment
3 Diseases of the skin around the eyes and inflammation of the eyelids. Diagnosis and treatment
Prevention of milia
To prevent the appearance of milia, careful facial skin care is required using cleansers and moisturizers appropriate to the skin type, scrubs, peels, cosmetic masks that normalize the activity of the sebaceous glands; elimination of provoking factors, proper and rational nutrition, healthy lifestyle. Salon cosmetic procedures, including mechanical, ultrasonic, vacuum facial cleansing, peelings (chemical, mechanical - microdermabrasion), laser resurfacing, are quite effective in preventing the appearance of milia.
Types of skin diseases around the eyes and eyelids
Among the huge number of diseases caused by inflammation of the eyelids, several of the most common groups can be distinguished:
- bacterial lesions of the skin of the eyelids (abscess of the eyelid, phlegmon);
- inflammatory diseases of the glands and edges of the eyelids (blepharitis, barley, chalazion, meibomitis, demodicosis);
- violations of the shape and position of the eyelids (entropion, eversion, ptosis, lagophthalmos);
- allergic diseases (eczema, dermatitis, angioedema);
- developmental abnormalities of the eyelids and tumors (coloboma, papilloma, lipoma, nevus).
Bacterial lesions of the skin of the eyelids
Abscess of the century
An abscess is inflammation and redness of the eyelid with the formation of a cavity filled with pus. Often an abscess appears after an infected eyelid wound.
Causes of eyelid abscess:
- ulcerative blepharitis;
- boils;
- barley;
- purulent processes in the paranasal sinuses and orbit of the eye.
Sometimes the abscess opens on its own, and the inflammation subsides. But in most cases, a non-healing fistula appears at the site of inflammation.
Treatment of an abscess is sanitation of the eyelids and opening of a purulent formation on the eyelids with the mandatory use of antibiotics and sulfonamides.
Phlegmon
Cellulitis is an extensive inflammation of the tissues of the eyelid that occurs against the background of untreated stye. It is characterized by fever, headache, severe swelling of the eyelid and redness of the skin.
Treated with antibacterial agents, antihistamines.
Inflammatory diseases of the glands and edges of the eyelids
Blepharitis
Blepharitis is an inflammation of the eyelids, which causes redness, burning, itching and pain on the skin.
The following types of blepharitis are distinguished: allergic, meibomian, demodectic, infectious, scaly. Read more about blepharitis here.
Barley
Barley is an acute, infectious inflammation of the eyelids, resulting from pathogens entering the eyelash hair follicle or the sebaceous gland of the eyelid. Visually, stye looks like a small nodule on the eyelid.
You can read about how to properly treat stye on this page.
Meibomyitis and chalazion
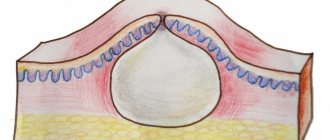
Meibomyitis and chalazion are diseases associated with the appearance of a pathological process in the meibomian glands.
Meibomia appears when the duct of the sebaceous gland of the eyelid is clogged. Characterized by an acute course of the disease.
Chalazion is a chronic form of meibomitis. If a chalazion is left untreated for a long time, it turns into an eyelid cyst. Sometimes, for diagnostic purposes, it is necessary to puncture the eyelid cyst to identify the nature of the neoplasm.
Treatment and removal of a cyst on the eyelid occurs using classical techniques or laser treatment.
For more information about the symptoms and treatment of this pathology, see here.
Demodicosis
A disease of the eyelids caused by the Demodex mite. It is characterized by the appearance of yellow mucus in the eyes, gluing and breaking of eyelashes, itching and burning of the eyes.
To cleanse the eye from foci of infection, cleaning (sanitation) and rinsing of the lacrimal ducts are used. Read about the treatment of demodicosis on this page.
1 Diseases of the skin around the eyes and eyelids. Diagnosis and treatment
2 Diseases of the skin around the eyes and eyelids. Diagnosis and treatment
3 Diseases of the skin around the eyes and eyelids. Diagnosis and treatment
Violations of the shape and position of the eyelids
Turn of the century
When the eyelid is inverted, its main edge is turned onto the eyeball. Because of this, the eyelashes touch the surface of the cornea and conjunctiva, the eyes become red, irritated, and tears constantly flow from them.
Causes of pathology:
- convulsive or spastic contractions of some parts of the orbicularis oculi muscle;
- cicatricial contractions of the conjunctiva and cartilage of the eyelid that occur in certain chronic eye diseases (for example, trachoma).
The most effective method of treatment is surgery. Plastic surgery for entropion of the eyelid is also possible.
Eversion of the century
Ectropion is an inversion of the edge of the eyelid. With this inflammation of the eyelid, the conjunctiva turns out in a certain area or throughout the entire eyelid, which leads to its drying out.
The fact that the eye is constantly open, even at night, contributes to clouding of the cornea, the appearance of keratitis and other diseases.
Causes of eversion of the eyelid:
- age-related changes in the eye with sagging of the lower eyelid;
- paralysis of the orbicularis oculi muscle;
- tightening of the skin of the eyelids due to injuries, burns (cicatricial eversion), systemic diseases of the body.
First, it is necessary to eliminate the main causes that caused this disease. Surgical procedures can then be used.
Ptosis
Ptosis is an abnormally low position of the upper eyelids in relation to the eyeballs. This leads to vision defects and rapid eye fatigue. Ptosis can be congenital or acquired.
Causes of ptosis:
- damage to the oculomotor nerve;
- damage to the muscle that elevates the upper eyelid;
- strokes, encephalitis and other neurological diseases.
Treatment of the disease is mainly surgical.
Lagophthalmos
Lagophthalmos is incomplete closure of the palpebral fissure, which leads to damage and drying of the cornea and conjunctiva.
Causes of the disease:
- eyelid injuries,
- jades,
- short eyelids from birth.
In addition to treating the underlying disease, artificial tears and disinfectant drops are prescribed. In severe forms of the disease, surgical intervention with partial suturing of the palpebral fissure is used.
Allergic inflammation of the eyelids
Allergic diseases of the eyelids are accompanied by severe itching, swelling and inflammation of the eyelids.
In eczema , the skin of the eyelids is covered with papules, vesicles and pustules. Characteristic rashes appear not only on the skin of the eyelids, but also on the body. The pathology develops after suffering eyelid dermatitis or contact with allergens. At the end of the disease, crusts and serous exudate appear on the skin of the eyelids.
Characteristic signs of urticaria are swelling of the eyelids, itching and burning of the skin of the eyelids. Subsequently, blisters appear on it.
With contact dermatitis , 6 hours after contact with the allergen, swelling and inflammation of the eyelids develop with itchy papules and vesicles. Usually both eyes are affected at once.
Treatment of allergic inflammation of the eyelids is medicinal.
1 Diseases of the skin around the eyes and eyelids. Diagnosis and treatment
2 Diseases of the skin around the eyes and eyelids. Diagnosis and treatment
3 Diseases of the skin around the eyes and eyelids. Diagnosis and treatment
Anomalies of eyelid development and tumors
Coloboma
Coloboma of the eye is one of the most unpleasant diseases, which is expressed in the absence of some eye membranes. Coloboma of the eyelid is the most common. The pathology appears on the upper eyelids, but sometimes affects the lower eyelids too.
Coloboma is usually triangular in shape, where the base of the triangle is the ciliary edge of the eyelids. Since the defect affects all layers of the organ of vision, there are no eyelashes and glands in the area of coloboma.
In most cases, it is congenital, but can also occur as a result of injury and other illnesses. Another type of congenital coloboma, iris coloboma, is one of the main causes of vision loss in childhood.
Coloboma is a serious danger to the eye, as it leads to degeneration of the cornea, keratitis and other secondary diseases of the organs of vision, as well as blindness!
The most effective treatment for coloboma is surgery. Surgery for coloboma involves excision of damaged tissue and movement of a musculocutaneous flap to the site of the defect. With the help of plastic surgery, the correct edge of the eyelids is formed, which prevents the appearance of ptosis, entropion, and other complications.
Benign formations of the century
Papilloma of the eyelids
Papilloma appears on the lower eyelid usually in people over 60 years of age.
It grows slowly, looks like gray-yellow papillae, and has a spherical or cylindrical shape. In 1 case out of 100, papilloma can turn into cancer. Treatment of eyelid papilloma is surgical.
Senile wart
A senile wart is a flat and even formation of brown, yellow or gray color. It grows in older people along the lower ciliary edge of the eyelids. Treatment: cryodestruction or laser removal.
Cutaneous horn
The cutaneous horn is a dirty gray formation protruding above the eyelid. Electro- and laser excision are used for treatment.
Nevi
Nevus (or mole ) is a benign formation on the skin, from light brown to black. Nevi on the eyelid can be inherited, appear due to long exposure to the sun, disruptions in the hormonal system, or after taking certain medications. Hanging moles can appear in old age. If the formation does not bother you, there is no need to treat it.
If unpleasant symptoms appear: itching, pain, growth, blurred vision, you must consult an ophthalmologist to investigate the nature of the mole and receive the necessary treatment.
Atheroma
Eyelid atheroma ( epidermal cyst ) is a painless, dense formation that appears on the eyelid due to blockage of the sebaceous gland ducts.
Over time, the atheroma begins to increase in size and can impair vision. In this case, surgical procedures are performed. After removal of atheroma of the eyelid, there are usually no complications.
How to care for oily skin?
Since milia are mainly characteristic of the dermis, which is prone to excessive sebum production, proper care will help prevent their formation. Recommendations for caring for oily skin:
- Cleansing. It must be carried out in such a way that the protective barrier of the skin is not damaged. Products with mild formulas will help get rid of excess fat, but will not upset the balance. It is not recommended to use regular soap for cleansing; formulations in the form of foam or gel are more suitable. Products may contain calendula, chamomile, aloe, and hyaluronic acid. The main thing is to always remove makeup before going to bed.
- Toning. Helps restore acid-base balance and eliminate the effects of environmental exposure. Tonics against blackheads, millet and oily shine mattify well, gently cleanse the skin, moisturize and refresh. They never contain alcohol and contain thermal water and other components.
- Exfoliation. Oily skin needs a scrub that provides a drying, soothing, cleansing effect. The procedure is aimed at eliminating keratinized scales.
- Hydration. In formulas for oily skin, the ratio of components is more water, less oil. These are light cream textures with a matting effect.
Getting rid of milia is not difficult, but this procedure should be entrusted to a professional cosmetologist. You can independently carry out only preventive measures aimed at preventing the formation of millet grass.
Treatment of skin diseases around the eyelids
If suspicious inflammation in the eyelid area, redness, or pain appears, you should consult an ophthalmologist. After the examination, the doctor will make an accurate diagnosis and explain what to do for eyelid swelling and other symptoms, prescribe adequate treatment, and recommend preventive measures. This can be a massage of the eyelids with rinsing of the lacrimal ducts, opening of formations on the eyelid, the use of ointments and medications.
Ophthalmologists at the MedicCity clinic will quickly find the cause of your eye disease.
We use high-precision diagnostic equipment and the latest methods for treating various ophthalmological diseases!
Come to us, we will take care of your vision!
Physiotherapy and massage in the treatment of meibomitis
After the acute period, at the stage of suppression and extinction of the infection, physiotherapeutic procedures with the effect of dry heat (for example, UHF or ultraviolet heating) are effective.
Massage of the eyelids in case of disease is aimed at improving the outflow of secretions from the glands. It is carried out with a glass rod and only by a specialist (ophthalmologist), because if the technique is incorrect, it can lead to generalization of the inflammatory process and the development of serious complications (abscess and phlegmon of the eyelid).
With recurrent variants of meibomitis, a thorough comprehensive examination is necessary to identify the causes and mechanisms of such a course (first of all, the level of sugar in the blood and urine is examined; a detailed analysis of hormonal levels may be necessary). Treatment may include, in particular, brewer's yeast and/or autohemotherapy.
In some cases, depending on the identified pathogen, the dynamics and severity of the process, oral antibiotic therapy is prescribed (which must be taken in strict accordance with the prescribed dosages and timing), washing the gland, etc.
Finally, if the applied therapeutic regimens are ineffective, the festering capsule sometimes has to be opened surgically. However, this procedure is quite simple, it is performed on an outpatient basis and, given the power of modern anesthetics, is practically painless.
Diagnostics
Removing milia on the face is the task of a cosmetologist. Before the procedure, the specialist must conduct appropriate diagnostic studies.
- The doctor examines the tumor and determines its clinical picture.
- To exclude a malignant process, a biopsy is performed, followed by sending the biomaterial for histological examination.
Chalazion in children
Chalazion is rare in children unless there is a congenital predisposition. The composition of fat secretion is different for everyone, as are the properties of the skin. If you have a predisposition to eye diseases and gland blockage, then there is a high probability that your child may inherit this feature.
Children aged 5 to 10 years are at risk. The difficulty is that the child is inattentive to eye hygiene. Pay attention if your child rubs his eyes frequently. Find out if he is bothered by itching or burning.
Treatment of chalazion in children is no different from treatment in adults. The only difference is that surgery cannot be performed using a laser if the child is under 14 years old.